Unveiling the Crucial Role of Ambulance Control Rooms
Explore the vital functions of ambulance control rooms, their technological advancements, and the challenges they face in managing emergency responses. Discover how these control rooms coordinate lifesaving services and handle increasing call volumes with efficiency and precision.


Ambulance control rooms, formally known as Emergency Operations Centres (EOCs), function as the indispensable central nervous system of emergency medical services. Their critical role extends beyond mere logistical coordination, encompassing initial call management, sophisticated patient triage, dynamic resource allocation, and seamless inter-agency collaboration. The efficiency and expertise within these centers directly determine the effectiveness of the entire emergency response pathway, from the initial public contact to definitive patient care and hospital handover, thereby profoundly influencing patient outcomes and the overall sustainability of the healthcare system.
This report highlights that EOCs operate under a dual imperative: achieving rapid response for critical emergencies while simultaneously ensuring the most appropriate, often less resource-intensive, care for non-emergencies. This complex balance is facilitated by advanced technologies such as Computer-Aided Dispatch (CAD) systems and next-generation communication networks. However, the full potential of these technological advancements is realized only through synergistic integration with highly skilled human operators, who form an "unseen clinical workforce" performing high-stakes assessments and delivering vital pre-arrival instructions. Despite their crucial contributions, control room staff face immense pressure, leading to significant burnout, high turnover, and systemic mental health challenges. Addressing these issues through proactive support and cultural shifts is paramount. Furthermore, the report underscores the direct impact of EOC actions on patient survival rates for time-sensitive conditions like cardiac arrest and stroke, emphasizing the critical importance of integrated multi-agency coordination, as exemplified by frameworks like JESIP. The future of EOCs will be characterized by increasing technological sophistication, particularly with the careful integration of Artificial Intelligence (AI) to augment human capabilities, and an even greater emphasis on seamless multidisciplinary collaboration. Recommendations for policymakers and healthcare leaders emphasize continuous investment in human capital, strategic technological adoption, and fostering robust inter-agency partnerships to enhance overall emergency response capabilities and ensure public safety.
The Nerve Centre of Emergency Response
Ambulance control rooms, frequently referred to as Emergency Operations Centres (EOCs), represent the pivotal central hubs for managing emergency medical responses. These facilities serve as the initial point of contact for individuals seeking urgent medical assistance, typically through emergency telephone numbers such as 999 in the United Kingdom or 911 in the United States. Beyond emergency calls, EOCs also manage non-emergency requests and facilitate inter-hospital patient transfers.
The foundational importance of EOCs to the emergency healthcare chain cannot be overstated. They are accurately described as the "nerve center" of emergency response operations. Their operational efficiency and the precision of their decision-making directly influence the entire response pathway, from the moment a call is received to the delivery of patient care and subsequent hospital handover. This comprehensive influence directly impacts critical patient outcomes and contributes to the overall sustainability of the broader healthcare system. Key responsibilities within EOCs include the reception and triage of incoming calls, the dispatch of appropriate emergency services, the provision of vital pre-arrival medical advice, and the effective management of available resources.
This report aims to provide a comprehensive understanding of the crucial role played by ambulance control rooms. It will delve into their core functions, operational procedures, staffing dynamics, the significant challenges faced by their personnel, their measurable impact on patient outcomes, their essential inter-agency coordination efforts, and the current trends and future innovations shaping their evolution.
A fundamental aspect of the control room's role is its function as the "first first responder." Control room operators are tasked with dealing with incoming emergency calls, prioritizing them, meticulously gathering necessary information, assessing the urgency of each incident, determining the most appropriate course of action, and subsequently directing emergency services teams to the scene. Furthermore, when an immediate ambulance response is not required, EOCs are equipped to provide assessment and treatment advice, a practice often termed 'hear and treat'. The Medical Priority Dispatch System (MPDS), a standardized protocol utilized by dispatchers, explicitly includes "pre-arrival instructions". These instructions are designed to empower the caller to act as an immediate intervener by providing potentially life-saving guidance, such as instructions for cardiopulmonary resuscitation (CPR), the use of a defibrillator, the Heimlich maneuver, or techniques for bleeding control. This capacity for immediate, actionable medical advice, delivered even before paramedics physically arrive, means that the control room is not merely a logistical hub. It is an active and critical participant in the earliest phase of patient care. This direct intervention can significantly influence the "golden hour" for patients with critical conditions. This establishes the control room as the initial point of clinical intervention, highlighting a proactive clinical role that extends far beyond mere dispatch. This paradigm underscores the immense responsibility and specialized skills required of call handlers, as their immediate guidance can be the difference between life and death, effectively extending emergency care into the pre-hospital phase before physical resources arrive. This also implies a continuous need for robust training and rigorous quality assurance for the delivery of these pre-arrival instructions.
Core Functions and Responsibilities
Ambulance control rooms, or Emergency Operations Centres (EOCs), perform a multifaceted array of functions that are central to the effective delivery of emergency medical services. These responsibilities span the entire spectrum of emergency response, from initial contact to ongoing resource management and major incident coordination.
The primary function of an EOC involves the management of incoming emergency calls, typically through 999 in the UK. Emergency services control room operators serve as the first point of contact for members of the public seeking urgent medical assistance. Beyond individual emergencies, EOCs are also responsible for receiving and triaging 999 calls related to major incidents, which require a coordinated, large-scale response. In the UK, the London Ambulance Service (LAS) further expands this role by operating 111 urgent care services, managing a substantial volume of calls for non-emergency health concerns and providing appropriate advice or referrals.
A critical responsibility within the EOC is the prioritisation and triage of these incoming calls. Operators must assess the urgency of each incident and make rapid decisions. Emergency Call Handlers utilize sophisticated systems such as the Medical Priority Dispatch System (MPDS) or NHS Pathways to conduct an initial assessment of both the patient's condition and the scene. These systems are designed to categorize the seriousness of the illness or injury, ensuring that patients with the most critical needs receive the fastest and most appropriate response. MPDS, a system refined since 1976, employs standardized protocols, including a series of key questions, pre-arrival instructions, and dispatch priorities, allowing for systematic categorization of calls based on chief complaint and severity.
Following triage, the EOC is responsible for dispatching appropriate resources. Based on the assessment, operators determine the best course of action and direct an emergency services team to the incident. This involves deploying a range of assets, including ambulances, rapid response vehicles (RRVs), helicopter crews, and specialized units such as Hazardous Area Response Teams (HART). Dispatchers leverage the triage system to select the most suitable staff and vehicles, taking into account the severity of the situation and the availability of resources.
Another vital function is providing pre-arrival instructions and advice, often referred to as "hear and treat." When callers do not require an immediate ambulance response, the EOC provides medical assessment and treatment advice over the phone. MPDS protocols specifically enable dispatchers to give instructions to callers while emergency assistance is en route. This empowers callers to perform potentially life-saving actions, such as cardiopulmonary resuscitation (CPR) or bleeding control, under remote guidance. Emerging technologies, such as the 'Luscii' app, further enhance this capability by allowing remote care clinicians within the control room to receive real-time patient vital signs and determine the most appropriate next steps, which could range from a referral to a General Practitioner (GP) or self-care advice to the dispatch of an ambulance. This innovation supports the overarching aim of providing the right care or advice, in the right place, every time.
Maintaining continuous contact with field teams and ensuring optimal resource efficiency are also core responsibilities. Control room staff maintain ongoing communication with teams at the scene of an incident to stay updated on the evolving situation and to ensure the safety of personnel. They are also tasked with ensuring the most effective use of available resources and that response teams adhere to agreed response time standards. This involves implementing dynamic deployment strategies, where resources are strategically moved closer to areas of predicted future call demand. This data-driven approach allows for more efficient resource allocation and better alignment of services with the specific needs of the communities served.
Finally, EOCs play a crucial role in managing non-emergency transfers and coordinating responses to major incidents. They handle requests from healthcare professionals for the transport of patients between hospitals or from the community into a hospital setting. In the context of major incidents, EOCs are central to the response, dispatching appropriate services as Category 1 providers under the Civil Contingencies Act 2004. During such large-scale events, the control room often assumes a tactical command role, coordinating the broader emergency response.
The operation of ambulance control rooms is driven by a dual imperative: achieving rapid response times for critical emergencies and ensuring the most appropriate, often less resource-intensive, care for non-emergencies. This means that the control room's function is not solely about speed; it is fundamentally about making the correct decision for each call. Over-dispatching resources unnecessarily can strain the entire system, while under-dispatching for genuine emergencies risks severe patient harm. The balance between providing rapid response for critical, time-sensitive cases and directing less severe cases to appropriate, non-ambulance pathways is a core tension within daily operations. This necessitates sophisticated triage systems and highly skilled clinical judgment. The control room acts as a crucial gatekeeper for the entire Emergency Medical Services (EMS) system, optimizing resource utilization and managing patient flow. Mismanagement of this delicate balance can lead to system overload, such as unnecessary ambulance dispatches, or conversely, delayed care for those who truly need it, thereby highlighting the EOC's profound role in system-wide resource optimization and patient flow.
Operational Procedures and Technology
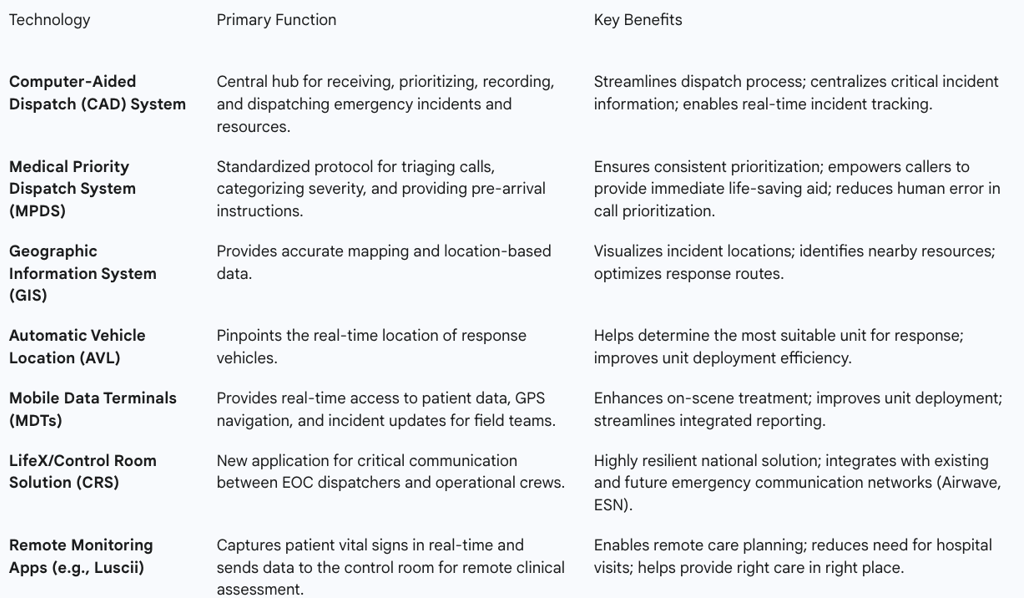
The efficiency and effectiveness of ambulance control rooms are profoundly shaped by their operational procedures and the sophisticated technologies they employ. These elements are intricately linked, forming the backbone of modern emergency medical dispatch.
Computer-Aided Dispatch (CAD) systems serve as the central technological hubs of emergency response operations. These advanced software solutions are utilized by dispatchers, call-takers, and 911 operators to systematically prioritize and record incident calls, ascertain the real-time status and location of responders in the field, and efficiently dispatch personnel. At their core, CAD systems are designed to capture, organize, and disseminate critical information related to incidents, including precise location data, caller details, incident type, and the availability of resources.
The power of CAD systems is significantly amplified through their integration with various other data systems. They commonly interface with Geographic Information Systems (GIS) to provide accurate mapping and location-based data, enabling dispatchers to visualize incident locations, identify nearby resources, and optimize response routes for faster and more efficient deployment. Automatic Vehicle Location (AVL) systems pinpoint the exact location of response vehicles, allowing the CAD system to determine the most suitable unit for a given response, while caller identification (ID) systems verify the precise location of incoming calls or incidents. Furthermore, CAD systems can integrate with Records Management Systems (RMS) to access data relevant to the current service call, providing a comprehensive operational picture.
A critical operational procedure enabled by these integrated technologies is dynamic deployment. Data derived from CAD systems, including detailed performance and activity reviews at various geographical levels, facilitates this practice. Dynamic deployment involves strategically moving emergency resources closer to areas where future calls are predicted to originate, utilizing designated standby points and continuously monitoring adherence to these plans. This data-driven approach allows for more efficient allocation of resources and ensures that services are more closely aligned with the specific needs of the communities they serve.
Data-driven performance monitoring and continuous improvement are integral to EOC operations. Ambulance services leverage data from CAD systems and other specialized reporting tools, such as the Department of Health (DH) ambulance reporting tool, to identify emerging trends, predict future needs, and allocate resources with greater efficiency. This analytical capability assists operational managers in pinpointing performance issues, directing improvement efforts, and evaluating the performance of individual call takers and dispatchers. Performance improvement strategies often involve a detailed process view of call and patient flow, identifying and addressing bottlenecks, and simplifying or expediting operational processes.
Advanced communication networks are fundamental to the seamless operation of control rooms. The Ambulance Radio Programme (ARP) is actively deploying a new LifeX application, known as the Control Room Solution (CRS), specifically designed for critical communication between EOC dispatchers and operational crews in the field. This system is designed to integrate with existing Airwave solutions and will eventually connect with the Emergency Services Network (ESN). Mobile Data Terminals (MDTs) are also transforming EMS operations by providing field teams with real-time access to patient data, GPS navigation, and incident updates, thereby enhancing efficiency. Furthermore, advanced communication hubs offer multiple redundancies, including 5G connectivity, dual modems, and optional geostationary and low earth orbit (LEO) satellite connections, ensuring continuous communication even in remote areas or mobile blackspots.
Emerging technologies are also beginning to shape the future of EOC operations. The 'Luscii' app, for instance, captures a patient's vital signs, such as heart rate and blood oxygen levels, and transmits this data in real-time to the ambulance control room. Remote care clinicians can then analyze this information to determine the appropriate next steps in care planning, which could include a referral to a GP, self-care advice, or the dispatch of an ambulance resource if necessary. This technology aims to facilitate care closer to home and reduce the necessity for hospital visits, thereby alleviating strain on healthcare services.
The effectiveness of ambulance control rooms is not solely dependent on the deployment of advanced technology but rather on the symbiotic integration of sophisticated systems with highly skilled human operators. While Computer-Aided Dispatch (CAD) systems, Geographic Information Systems (GIS), and real-time data streams provide an unparalleled informational foundation, the critical interpretation of this data, nuanced decision-making in complex situations, and empathetic communication with distressed callers remain firmly within the human domain. For example, dispatchers use intuitive user interfaces within the CAD system to input and manage calls, log information, contact appropriate personnel, and monitor response status. The system also provides performance reports on individual call takers and dispatchers. This relationship demonstrates that technology augments human capability, allowing for faster, more informed decisions, but does not replace the inherent need for human judgment, especially in complex or emotionally charged situations. This signifies that technological advancements must be accompanied by continuous human training and adaptation to fully leverage their potential, emphasizing that technology serves as an enabler, not a replacement, for expert human judgment.
Table 3.1: Key Technologies and Their Functions in Ambulance Control Rooms
Staffing, Qualifications, and Training
The operational effectiveness of ambulance control rooms is intrinsically linked to the expertise and dedication of their diverse staff. These professionals work collaboratively within a structured hierarchy to manage the complex demands of emergency medical dispatch.
Ambulance control rooms typically feature a multi-layered staffing structure designed to handle various aspects of emergency response. Key roles include:
Emergency Medical Advisors (EMAs) / Call Handlers: These individuals represent the first point of contact for 999 calls, bearing the crucial responsibility of taking essential details, prioritizing calls, and delivering vital pre-arrival instructions. While some ambulance trusts may combine the roles of call handler and dispatcher, others maintain them as separate functions.
Clinical Advisors: These are registered healthcare professionals, such as nurses or paramedics, who operate within the Clinical Assessment Hub. Their role involves providing telephone triage for clinically complex 999 calls, leveraging their clinical knowledge and specialized decision-support software to assess patient needs and arrange appropriate care, including directing patients to non-ambulance pathways when suitable.
Dispatch Officers: These personnel are responsible for the critical task of dispatching ambulances and other emergency resources based on the information provided by EMAs and Clinical Advisors. They must expertly manage a dynamic workload, liaise continuously with ambulance crews, and ensure that resources are allocated with maximum efficiency.
Team Leaders / Control Shift Officers / Supervisors: Occupying a supervisory role, these individuals oversee teams of dispatchers and call handlers. Their responsibilities encompass shift management, performance monitoring, providing essential staff support, and escalating significant issues to higher command levels.
The required qualifications and essential skills vary depending on the role within the control room. For entry-level positions such as EMAs or Call Handlers, candidates typically require a GCSE (or equivalent) in English at Grade C or above (Grade 4–9). Notably, previous healthcare or medical training is not a prerequisite for these roles, as comprehensive training is provided. Essential skills for these positions include excellent verbal and written communication, active listening, strong problem-solving abilities, the capacity to prioritize tasks and make rapid decisions, maintaining composure under pressure, proficiency in IT systems, and customer service experience. Clinical Advisors, given their specialized function, must possess a current valid HCPC (Health and Care Professions Council) or NMC (Nursing and Midwifery Council) registration, coupled with at least two years of post-registration experience and a willingness to complete NHS Pathways and/or PACCs training. Dispatch Officers typically require GCSE grades C/4-9 in Maths and English, IT competence, customer service experience, and the crucial ability to multitask and manage competing priorities effectively.
Training pathways and continuous professional development are integral to maintaining high standards within EOCs. Most training is delivered on the job, with new staff working alongside experienced personnel, supplemented by more formal courses. For instance, new EMAs receive comprehensive training and mentoring, which includes an intensive 11-12 weeks of classroom learning, during which they also undertake supervised 999 call-taking shifts. Training modules are tailored to the organization's specialization but generally cover community awareness, problem-solving skills, computer system usage, administrative paperwork, and advanced listening and questioning techniques. Specific training for dispatchers can encompass customer service, contact centre operations, and certification in the International Computer Driving Licence (ICDL). More advanced training for emergency medical dispatchers includes handling complex medical emergencies, refining communication techniques, and understanding the legal aspects pertinent to dispatching. Career progression within the ambulance service often begins as an emergency call handler, with opportunities to advance to team leader, manager, or duty manager roles. Further training can also enable staff to transition into roles such as emergency care assistant or paramedic.
In the UK, the hierarchy and team structure within ambulance control rooms are well-defined. The London Ambulance Service (LAS), for example, operates its Emergency Operations Centres (EOCs) from two primary sites: Waterloo and Newham. The 999 Operations department is responsible for providing the staff who work in these EOCs, including call-takers and dispatchers. This department also houses a dedicated clinical hub, staffed by clinical advisors who conduct "hear and treat" assessments and clinical team navigators who provide clinical support to frontline crews and other EOC staff, while maintaining oversight of clinical safety at the operational level. Control rooms operate on a shift basis, providing 24-hour, 7-day-a-week coverage. The overarching organizational structure includes a Trust Board and various directorates, with EOCs falling under the Accident and Emergency Operations directorate. During major incidents, command structures typically follow a nationally recognized Gold (strategic), Silver (tactical), and Bronze (operational) system, with control rooms often fulfilling tactical (Silver) command functions.
Ambulance control rooms house a unique and often underestimated "unseen clinical workforce." While frontline paramedics are directly responsible for delivering patient care at the scene, the staff within EOCs, particularly Emergency Medical Advisors (EMAs) and Clinical Advisors, perform initial, high-stakes clinical assessments, conduct critical triage, and deliver potentially life-saving pre-arrival instructions over the phone. This necessitates a training curriculum that instills not only operational protocols but also foundational clinical reasoning and sophisticated communication skills, effectively transforming these individuals into remote clinicians. This signifies that these roles are not merely administrative or logistical; they involve direct, impactful clinical decision-making from a distance. This highlights the need for greater public recognition, appropriate remuneration that reflects the immense responsibility and skill involved, and the establishment of specialized professional development pathways for these roles, acknowledging their direct and profound impact on patient outcomes.
Challenges Faced by Control Room Staff
Despite their crucial role, ambulance control room staff confront a myriad of significant challenges that profoundly impact their well-being and the efficiency of emergency services. These challenges are often rooted in the high-pressure nature of their work and systemic issues within the broader healthcare environment.
One of the most pervasive challenges is the immense pressure, burnout, and profound psychological toll experienced by 999 call handlers. These individuals operate under relentless stress, making split-second decisions that directly affect lives. They frequently deal with highly distressing calls, including incidents involving suicides, stabbings, shootings, and the tragic reality of patients dying before an ambulance can reach them. This constant exposure to trauma and high-stakes situations leads to significant psychological strain, burnout, and mental ill health. Data from the 2023 NHS staff survey revealed that 44% of control room staff reported feeling burnt out, a figure higher than that for other ambulance personnel.
This intense pressure contributes directly to high staff turnover and elevated sickness absence rates. High turnover among call handlers is frequently attributed to a perceived lack of adequate support and the non-stop, distressing nature of the calls. Over a three-year period, from April 2021 to April 2024, more than half a million days were lost to call handler illness across the UK, equating to over a month of sick leave per call handler in 2023/24. Some ambulance organizations have reported as many as 50% of their employees leaving the workforce, with poor staff mental health and organizational culture cited as primary contributing factors.
The impact of complex emergencies and distressing calls is particularly acute. Staff are often required to handle intricate situations, such as mental health crises, during long shifts (e.g., 12 hours) with limited breaks. The continuous exposure to critical incidents and work-related traumatic events, compounded by the everyday stressors of increasing demand for EMS services, significantly compromises mental health. Personal experiences within calls can deeply affect staff, sometimes leading to extended periods of sick leave.
Systemic issues, notably resource limitations and lengthy hospital handover delays (Ambulance Patient Offload Time - APOT), further exacerbate the pressure on control room staff. The inherent limitations in available resources intensify the demanding nature of the work. Prolonged APOT at hospitals creates a critical bottleneck within both the EMS and wider healthcare systems, preventing ambulance crews from returning to the road to respond to new emergencies. This directly reduces ambulance availability, impedes response times, and places immense strain on financial and human resources, contributing significantly to burnout among both dispatchers and paramedics. Staffing shortages in both EMS and Emergency Departments (EDs) further compound the APOT crisis, creating a vicious cycle of delays and increased pressure.
A significant challenge frequently cited by staff is the perceived lack of consistent support and issues within the organizational culture. Call handlers often report that supervisors rarely check in on their well-being after difficult or deeply upsetting calls. Employees express a desire for proactive well-being checks and genuine concern from their organizations, rather than a perceived fulfillment of mere organizational obligation. Cultural factors, such as machismo and stigma, can also act as significant barriers, discouraging staff from seeking the mental health support they need.
In response to these critical issues, several specific mental health support programs have been implemented in the UK. The Ambulance Staff Charity (TASC) operates an independent and confidential crisis phoneline, offering immediate and ongoing suicide and mental health care specifically for UK ambulance staff. TASC also provides a range of counselling and specialist services for trauma and Post-Traumatic Stress Disorder (PTSD). Mind Charity offers valuable resources tailored for emergency responders, including those in the ambulance service, focusing on coping strategies for difficult experiences and guidance for supporting colleagues. Some NHS ambulance trusts have developed in-house initiatives; for example, the South Western Ambulance Service (SWAST) provides a confidential "Staying Well Service" for all its personnel, addressing physical, mental, social, and emotional needs. The North East Ambulance Service (NEAS) launched a "Mental Maintenance" campaign, aiming to shift the focus from crisis response to a proactive, regular approach to mental health through tailored toolkits, education, and peer support. This initiative has led to increased staff confidence and improved perceptions of managerial support. Additionally, the London Ambulance Service (LAS) has integrated specialist mental health clinicians within its emergency control room to provide remote clinical assessment and facilitate referrals for patients with mental health issues.
The data reveals a pervasive and systemic mental health crisis within ambulance control rooms, where the immense pressure and constant exposure to traumatic events lead to alarmingly high rates of burnout, sickness, and staff turnover. This situation is not merely an individual problem for specific employees but represents a critical operational vulnerability for the entire emergency medical service. The "heroism" often associated with emergency services, while admirable, inadvertently contributes to a culture where seeking mental health support might be stigmatized or perceived as a weakness, thereby exacerbating the underlying problem. The broader implication is that without significant, proactive investment in comprehensive mental health infrastructure, fundamental cultural shifts within organizations, and consistent, empathetic supervisory support, the sustainability and effectiveness of ambulance control rooms will continue to be compromised. This, in turn, directly impacts patient safety and the entire emergency response chain, as stressed and depleted staff are less able to perform their life-critical duties effectively.
Impact on Patient Outcomes and Response Times
Ambulance control rooms exert a profound and direct influence on patient outcomes and emergency response times across a spectrum of medical conditions. Their initial decisions and ongoing management are critical determinants of patient well-being.
Control rooms directly influence response times for various call categories by efficiently prioritizing incoming calls and dispatching appropriate resources. However, delays in ambulance response, particularly those exacerbated by prolonged Ambulance Patient Offload Time (APOT) at hospitals, can severely jeopardize patient outcomes and impede the ability of EMS to respond to new emergencies. For instance, in one documented case, the average response time for a Category 2 call was nearly three times slower than the NHS target, with significant repercussions for patient health.
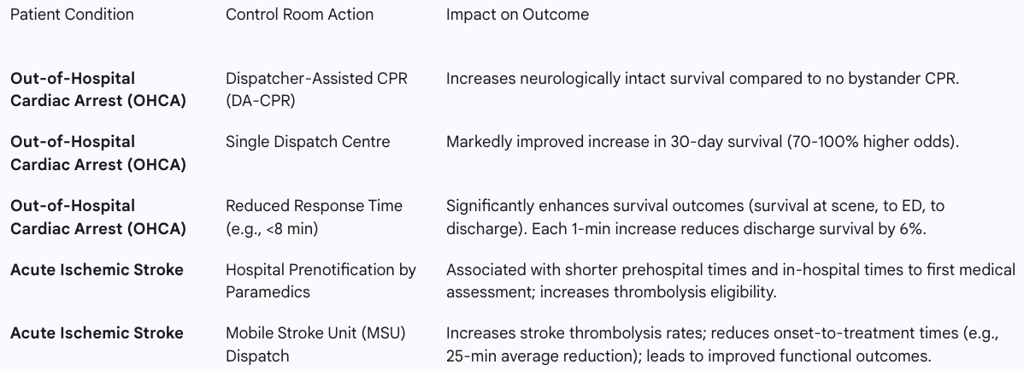
The role of control rooms in improving survival rates for time-sensitive conditions, such as cardiac arrest and stroke, is particularly notable:
Cardiac Arrest (Out-of-Hospital Cardiac Arrest - OHCA): Research consistently demonstrates that dispatcher-assisted cardiopulmonary resuscitation (DA-CPR) significantly increases neurologically intact survival rates compared to situations where no bystander CPR is initiated. Studies also indicate that a single dispatch centre, as opposed to multiple centers, is associated with a markedly improved increase in survival among OHCA patients. This improvement is linked to a reduced time from the first call to the first attempted CPR and a significantly higher proportion of bystander CPR in single dispatch center systems. In King County, for example, the ability of 911 dispatchers to quickly identify cardiac arrest and coach bystanders through CPR contributed to a significantly higher survival rate (nearly 19%) compared to the national average (approximately 10%). Furthermore, a critical finding indicates that each one-minute increase in response time for OHCA cases decreases the likelihood of survival to hospital discharge by 6%.
Stroke: Ambulance call-takers and paramedics are strategically positioned to identify and respond rapidly to suspected stroke events. Hospital prenotification by paramedics is strongly associated with shorter prehospital times and reduced in-hospital times to the first medical assessment, which in turn increases a patient's eligibility for thrombolysis, a time-critical treatment for ischemic stroke. Mobile Stroke Units (MSUs), specialized ambulances equipped with diagnostic capabilities, have been shown to increase stroke thrombolysis rates and significantly reduce onset-to-treatment times, leading to improved functional outcomes for patients. Despite these advancements, challenges remain in the accuracy of initial assessment; while the Medical Priority Dispatch System's (MPDS) Stroke Diagnostic Tool shows some capability in identifying stroke/TIA, a substantial proportion of calls dispatched as potential stroke are not ultimately confirmed as such, indicating complexities in initial telephone assessment.
The consequences of delays and inefficiencies originating within or impacting the control room are severe for patient health. Lengthy delays have a devastating impact on patients. Prolonged APOT not only diminishes ambulance availability but also exacerbates overcrowding in emergency departments, leading to a reduced quality of care, increased patient risk, and potentially adverse outcomes. Moreover, fatigue and stress experienced by control room staff can negatively affect patient safety, highlighting the interconnectedness of staff well-being and patient care quality.
The impact of ambulance control rooms on patient outcomes, particularly survival, is not a simple linear correlation with overall response times. While rapid response is undeniably critical for highly time-sensitive conditions such as Out-of-Hospital Cardiac Arrest (OHCA), where every minute directly influences survival , broader medical research suggests that the relationship between general response time and overall mortality is more complex. This complexity arises because existing research may fail to account for the "endogeneity of incident severity and response times" , meaning that patients with more severe conditions might inherently experience longer response times due to the nature of their emergency or location, making a direct causal link harder to isolate across all scenarios. This implies that control rooms must employ highly sophisticated triage and dispatch algorithms, such as MPDS, to accurately identify and prioritize cases where an ultra-fast response is truly life-saving. Simultaneously, they must optimize resource allocation for other call types to prevent system strain and ensure appropriate care delivery. The overarching focus should therefore be on delivering the "right care at the right time" rather than simply striving for the fastest response time for every incident, recognizing the nuanced impact of time on different medical emergencies.
Table 6.1: Impact of Control Room Actions on Key Patient Outcomes
Integration and Coordination with Other Emergency Services and Healthcare Providers
The effectiveness of ambulance control rooms is not confined to their internal operations but is critically dependent on their seamless integration and coordination with other emergency services and healthcare providers. This multi-agency collaboration is paramount for a coherent and efficient emergency response system.
Effective multi-agency coordination is a crucial factor in emergency care systems, ensuring the delivery of integrated, person-focused care across diverse settings. In the United Kingdom, the Joint Emergency Services Interoperability Principles (JESIP) framework provides a standardized approach to multi-agency working, encompassing training and awareness products for all responding organizations. JESIP's overarching objective is to ensure that emergency services work together coherently to save lives and reduce harm.
Communication and information sharing are at the heart of this coordination. Control rooms play a vital role in managing the early stages of multi-agency incidents by adopting a swift and joint approach. This involves multi-agency discussions among control room supervisors, where information from all available sources, immediate resource availability, and decisions are shared. A "talk not tell" procedure encourages open dialogue, and the nomination of a single point of contact (SPoC) in each control room, along with agreed communication methods (e.g., telecommunications links, multi-agency interoperable talkgroups), is deemed essential. Electronic data transfer is preferred to minimize congestion on voice channels and prevent misunderstandings. The London Ambulance Service's command and control system, for instance, is electronically linked with that of the Metropolitan Police. During major incidents, structured reporting using the M/ETHANE mnemonic (Major incident, Exact location, Type of incident, Hazards, Access, Number of casualties, Emergency services required) is crucial for initial situation reports and ongoing updates, ensuring all agencies have shared situational awareness.
The management of major incidents and complex emergencies necessitates sophisticated coordination. EOCs receive and triage 999 calls related to major incidents and dispatch appropriate responses as Category 1 providers under the Civil Contingencies Act 2004. During incidents such as the Clapham high street shooting, the London Ambulance Service's tactical operations centre demonstrated rapid decision-making and inter-service coordination by dispatching multiple crews to a rendezvous point, where they awaited police armed response before entering the scene. Major incidents, by definition, require an extraordinary allocation of resources and frequently involve responders from multiple services and jurisdictions. The UK typically employs a Gold (strategic), Silver (tactical), and Bronze (operational) command structure. Control rooms often operate at the Silver (tactical) level, managing the incident from a central point and coordinating with on-scene commanders. Challenges can arise, however, including difficulties in obtaining comprehensive information early in an incident and delays in forming Strategic Coordinating Groups (SCGs) for multi-agency discussion.
Joint training exercises and co-location strategies are vital for fostering effective multi-agency collaboration. Joint training exercises involving ambulance, police, and fire services are considered essential for testing operating procedures in realistic and challenging environments. These exercises aim to improve the collective response and ensure preparedness for major incidents. JESIP specifically trains control room managers and supervisors in joint ways of working, emphasizing the development of shared situational awareness, joint decision-making, and the avoidance of single-service language. While control rooms generally operate from separate fixed locations and cannot physically co-locate, virtual co-location through interoperable Airwave talkgroups, teleconferencing, and video conferencing is utilized to achieve coordination objectives. Physical co-location of commanders at the scene, when possible, is considered essential for optimal coordination. Examples of such joint exercises include a scenario in Warwickshire involving suspected explosives and rogue individuals , and "Exercise Joint Endeavour" in Merseyside, which involved nearly 1,000 personnel from various agencies to test joint operability and decision-making over a 14-hour period.
The evolution of emergency response, particularly in the context of major incidents, has moved beyond siloed operations towards a critical emphasis on integrated command and control, exemplified by frameworks like JESIP. Public inquiries following significant incidents, such as the London bombings in 2005 and the Derek Bird shootings in Cumbria in 2010, revealed that while emergency services performed well independently, their collective effectiveness was hampered by a lack of seamless coordination. This recognition directly led to the development of frameworks like JESIP, which provide a structured approach to multi-agency working, training, and communication. Ambulance control rooms are pivotal in this paradigm shift, serving as the central nervous system for multi-agency coordination. Their ability to establish shared situational awareness, facilitate joint decision-making (even through virtual co-location when physical presence is not feasible), and ensure seamless communication across police, fire, and other healthcare entities directly determines the efficacy of a large-scale response. This signifies that ongoing investment in joint training initiatives, interoperable communication technologies, and fostering a culture of collaborative leadership within control rooms is not merely an operational enhancement but a fundamental requirement for national resilience and public safety in an increasingly complex threat landscape.
Trends and Future Innovations
The landscape of ambulance control rooms is continually evolving, driven by advancements in technology and a growing imperative for enhanced efficiency and patient outcomes. Artificial Intelligence (AI) and sophisticated communication technologies are at the forefront of these transformative trends.
The emerging role of Artificial Intelligence (AI) in dispatch, triage, and resource optimization is revolutionizing pre-hospital care, with the potential to enhance decision-making, improve patient outcomes, and ultimately save lives.
Rapid Call Analysis and Triage: AI-powered dispatch systems leverage predictive analytics to optimize resource allocation. AI algorithms can swiftly analyze caller information, identify the severity of a situation, and dispatch appropriate resources, thereby saving valuable time and reducing human error in prioritization. AI can process information rapidly, assisting dispatchers in prioritizing urgent calls. It can analyze voice patterns, transcribe calls in real-time, and identify keywords associated with life-threatening events like cardiac arrest, potentially spotting more such cases faster than human dispatchers within the first minute.
Resource Prioritization and Dynamic Allocation: AI analyzes historical and current data, including caller location and symptoms, to suggest the most efficient deployment of emergency units. This ensures that the most serious cases receive immediate attention and optimizes the utilization of limited resources. AI can also predict demand patterns, enabling more effective resource allocation and proactive response strategies.
Management of Non-Emergency Calls: AI-powered chatbots and virtual agents are increasingly capable of handling routine or low-urgency inquiries. This capability has been shown to reduce the volume of calls requiring human intervention by approximately 30-36% in some urban areas, freeing human dispatchers to focus on critical emergencies.
Enhanced Situational Awareness: AI-powered analytics can rapidly process vast amounts of data from multiple sources, including unstructured text and multimedia, to identify patterns, predict trends, and provide real-time insights to call handlers and dispatchers, thereby improving decision-making during critical incidents.
Language Translation and Emotion Recognition: AI tools can provide real-time translation and transcription, which significantly assists non-English speakers in communicating their emergencies effectively and speeds up emergency response in diverse communities. Furthermore, AI is developing the capability to understand caller emotions, such as anger or fear, providing dispatchers with additional context to de-escalate tense situations before responders arrive.
Advancements in communication technologies are equally transformative. The integration of 5G offers ultra-fast data sharing and extended coverage, which is particularly crucial for coordinating responses during mass casualty incidents. Next-generation radio systems are enhancing range, clarity, and security, with multiband radios enabling improved cross-agency coordination and Push-to-Talk Over Cellular (PTT) solutions combining traditional radio communication with mobile LTE networks. Mobile Data Terminals (MDTs) and OnTrack CAD solutions are streamlining EMS operations by providing field teams with real-time access to patient data, GPS navigation, and incident updates. Additionally, wearable devices worn by patients with ongoing health issues can continuously track vital signs and alert emergency services to sudden problems, enabling earlier intervention and potentially preventing conditions from worsening.
While AI offers significant benefits, its implementation in ambulance control rooms presents both opportunities and challenges. The benefits include faster dispatching, reduced human error in prioritization, and AI-driven insights for better emergency planning. AI can also alleviate dispatcher workload and burnout by handling non-emergency reports and assist with documentation, potentially completing up to 90% of a report. However, several challenges must be addressed. Privacy and security concerns are paramount, as AI systems handle sensitive patient and caller information, necessitating robust cybersecurity and data protection measures. Overreliance on AI can lead to mistakes or missed critical details, as AI may misinterpret distressed speech, dialects, or slang. Algorithmic bias, stemming from biased training datasets, can result in unfair delays for certain demographic groups, underscoring the need for diverse training data and independent audits. Human oversight remains crucial; AI should assist, not replace, trained dispatchers, who are essential for complex, sensitive, or ethically nuanced cases. Public trust and transparency are also vital, as skepticism or distrust can arise from AI-driven responses, necessitating public education and transparent reporting on AI's capabilities and limitations. Furthermore, the initial funding and ongoing maintenance costs for AI systems can be substantial , and poor interoperability among existing legacy systems remains a persistent national problem that AI integration must navigate.
Beyond technology, flexible staffing models and integrated multidisciplinary teams are emerging trends. Hospitals are exploring flexible scheduling options, such as part-time or on-call workers, to align staff numbers with fluctuating patient demand, using data to predict peak times. Emergency care is also moving towards integrated multidisciplinary teams comprising paramedics, doctors, X-ray specialists, and surgeons, with clear communication protocols designed to expedite patient care.
The future of ambulance control rooms involves an "augmented dispatcher" model, where Artificial Intelligence functions as a powerful co-pilot rather than a direct replacement for human operators. While AI demonstrates exceptional capabilities in rapid data analysis, efficient triage, and automating routine tasks, thereby freeing human dispatchers to concentrate on critical incidents and complex cases, its implementation is not without inherent risks. These include algorithmic bias, significant privacy concerns, and the fundamental inability to fully grasp human nuance or emotional distress in the same way a human can. This necessitates a strategic implementation approach that prioritizes robust human oversight, ensuring that dispatchers receive continuous training to effectively collaborate with AI systems, and maintaining transparent communication with the public to build and sustain trust. The ultimate objective is to leverage AI's efficiency gains to enhance, rather than diminish, the human element of compassionate, intelligent, and effective emergency response, ensuring that the unique cognitive and emotional capabilities of human dispatchers remain central to the system.
Conclusion and Recommendations
Ambulance control rooms are undeniably the crucial nerve centers of emergency medical services, performing indispensable functions from initial call intake and triage to dynamic resource dispatch and inter-agency coordination. Their operational efficiency and the expertise of their staff directly underpin the effectiveness of the entire emergency response chain and significantly influence patient outcomes.
The comprehensive analysis reveals several key findings and their implications:
Multifaceted Functions: Emergency Operations Centres (EOCs) are dynamic hubs responsible for managing a diverse range of call types, including both 999 emergencies and 111 urgent care requests. They provide critical pre-arrival instructions that can be life-saving and coordinate complex major incidents, demonstrating their broad operational scope.
Technology as an Enabler: Advanced technologies such as Computer-Aided Dispatch (CAD) systems, Geographic Information Systems (GIS), and next-generation communication networks are vital for optimizing response times and resource allocation. However, their full potential is realized only through synergistic integration with the interpretive skills, nuanced decision-making, and empathetic communication of human expertise.
The Unseen Clinical Workforce: Control room staff, particularly Emergency Medical Advisors (EMAs) and Clinical Advisors, perform high-stakes clinical assessments and interventions remotely. This highlights their critical role as remote clinicians, directly impacting patient care from the first point of contact.
Systemic Mental Health Challenges: The inherently demanding and often traumatic nature of the work leads to significant burnout, high staff turnover, and pervasive mental health issues among control room personnel. This necessitates robust and proactive support systems that address both individual well-being and organizational culture.
Direct Impact on Outcomes: EOC actions, such as the provision of dispatcher-assisted CPR and efficient stroke prenotification, demonstrably improve survival rates and functional outcomes for time-sensitive medical conditions like cardiac arrest and stroke. While the relationship between general response time and overall mortality is complex, the targeted impact on critical conditions is clear.
Inter-agency Imperative: Frameworks like the Joint Emergency Services Interoperability Principles (JESIP) underscore the critical need for seamless, integrated multi-agency coordination. Control rooms are at the heart of this integration, facilitating information sharing and joint decision-making across police, fire, and other healthcare entities.
AI's Transformative Potential: Artificial Intelligence offers significant promise for enhancing efficiency, automating routine tasks, and improving decision-making in emergency dispatch. However, its implementation requires careful consideration to address ethical concerns, ensure data privacy, mitigate algorithmic bias, and maintain essential human oversight and public trust.
Based on these findings, the following strategic recommendations are put forth to enhance the effectiveness and sustainability of ambulance control rooms:
Invest in Human Capital and Well-being:
Implement comprehensive, continuous training programs that blend technical proficiency in dispatch systems with advanced clinical assessment and communication skills. This acknowledges and further develops the "unseen clinical workforce" within EOCs.
Prioritize and adequately fund proactive mental health and well-being programs for all control room staff. This includes fostering a supportive organizational culture that actively destigmatizes seeking help, ensuring regular, mandated breaks, and providing consistent supervisory check-ins. Access to independent, confidential support services, such as those provided by TASC and Mind Charity, should be readily available and promoted.
Review remuneration and career progression pathways to ensure they adequately reflect the immense pressure, responsibility, and specialized skills required for these roles, thereby attracting and retaining highly skilled personnel.
Leverage Technology Strategically:
Continue strategic investment in advanced CAD systems, GIS, AVL, and next-generation communication networks (e.g., 5G, LifeX/CRS). This will enhance real-time situational awareness, enable dynamic resource allocation, and ensure robust communication redundancies, even in challenging environments.
Adopt AI solutions with caution and a clear, ethical strategy. The focus should be on augmenting human capabilities in triage, non-emergency call management, and complex data analysis, rather than replacement. Prioritize the development and adherence to ethical guidelines, ensure robust data privacy and bias mitigation strategies, and maintain strong human oversight to build public trust and prevent overreliance on automated systems.
Strengthen Inter-agency Collaboration:
Reinforce adherence to established multi-agency frameworks like JESIP, promoting shared understanding, standardized communication protocols (e.g., M/ETHANE), and joint decision-making across all emergency services.
Increase the frequency and realism of multi-agency training exercises that specifically involve control room staff. These exercises are crucial for testing and refining interoperability in diverse, high-pressure scenarios, including major incidents, ensuring a cohesive response.
Develop and implement standardized data sharing platforms and communication channels that facilitate seamless information exchange between control rooms and other healthcare providers (e.g., hospitals, mental health services). This is essential for optimizing patient flow, reducing handover delays, and ensuring continuity of care.
Optimize Resource Allocation and Patient Pathways:
Continuously refine triage protocols, such as MPDS and NHS Pathways, to ensure the most appropriate resource dispatch. This involves balancing rapid response for critical, time-sensitive cases with effective "hear and treat" or alternative care pathways for non-emergencies, thereby optimizing resource utilization across the entire system.
Address systemic bottlenecks, such as Ambulance Patient Offload Time (APOT), through collaborative initiatives with hospitals. This should focus on improving Emergency Department (ED) throughput and addressing staffing shortages in both EMS and EDs to ensure ambulances can return to service promptly.
The future outlook for ambulance control rooms will be characterized by increasing technological sophistication, particularly with the careful and strategic integration of AI to augment human capabilities. There will also be an even greater emphasis on seamless multi-agency and multidisciplinary collaboration. As demand for emergency services continues to rise, these vital centers will evolve into highly intelligent, resilient, and integrated command hubs. This evolution will necessitate continuous adaptation, strategic investment in both cutting-edge technology and human capital, and a profound commitment to supporting the dedicated professionals who serve at their heart, ensuring they remain capable of delivering life-saving care in an ever-complex environment.
Frequently Asked Questions (FAQ)
Q: What is the role of ambulance control rooms?
A: Ambulance control rooms coordinate emergency medical services by receiving and dispatching emergency calls, managing ambulance crews, and ensuring timely patient care1.
Q: How have call volumes to ambulance control rooms changed?
A: Call volumes have surged, with some control rooms handling millions of calls annually due to factors like an ageing population and increased awareness of emergency services2.
Q: What technological advancements are being used in ambulance control rooms?
A: New telephony and communications systems, such as the LifeX solution, enhance communication and streamline information processing in control rooms3.
Q: What challenges do ambulance control rooms face?
A: Challenges include ensuring adequate staffing, integrating new technologies, and managing sudden surges in call volumes2.
Q: How has the Welsh Ambulance Service improved its control room capabilities?
A: The Welsh Ambulance Service has implemented the LifeX multimedia communication solution, which improves communication and resource coordination3.
Q: What is the role of control room staff in Thames Valley Air Ambulance?
A: Thames Valley Air Ambulance control room staff receive and coordinate 999 calls, working closely with other ambulance services to ensure efficient resource dispatch6.
Q: How does the London Ambulance Service handle high call volumes?
A: The London Ambulance Service has invested in a new high-tech control room and a Computer-Aided Dispatch (CAD) system to handle over one million 999 calls annually5.
Q: What is the impact of the COVID-19 pandemic on ambulance control rooms?
A: The pandemic highlighted the need for surge capacity planning, as control rooms experienced unprecedented call volumes and had to adapt quickly.
Q: How do ambulance control rooms ensure efficient communication?
A: Control rooms use advanced communication systems like LifeX, which integrate with existing and upcoming emergency services networks to ensure seamless communication4.
Q: What steps are being taken to recruit and retain control room staff?
A: Ambulance services actively recruit and provide training to ensure adequate staffing levels and retain qualified personnel2.
Additional Resources
For those interested in exploring the topic of ambulance control rooms in more depth, the following resources provide valuable insights and further reading:
Ambulance Radio Programme - Providing critical communication solutions to ambulance services across the UK. Could you read more on Ambulance Radio Programme 7?
London Ambulance Service NHS Trust - Offering a detailed look at the control room staff and their roles in managing emergency calls. Read more on London Ambulance Service 1.
Thames Valley Air Ambulance - Insights into the day-to-day operations of an air ambulance control room and the staff who make it possible. Read more on Thames Valley Air Ambulance 6.
Welsh Ambulance Services University NHS Trust - Information on the new control room technology helping to improve emergency response times. Read more on Welsh Ambulance Services 3.
