Understanding the Manchester Triage System
The Manchester Triage System (MTS) is a standardized approach to prioritizing patients in emergency departments based on clinical urgency, ensuring that those with life-threatening conditions receive immediate attention while others are categorized appropriately for timely care.
The Manchester Triage System (MTS) serves as a pivotal clinical risk management tool within emergency care environments. Its fundamental objective is to subject all arriving patients to a structured, consistent assessment procedure to ascertain the urgency of their medical condition. This systematic approach ensures that individuals with the most critical needs are prioritized for timely medical evaluation and intervention. It is crucial to understand that the MTS is not engineered to establish a definitive diagnosis at the point of triage; rather, its focus is on assessing urgency based on the patient's presenting symptoms and signs. The system is designed to facilitate the safe and efficient management of patient flow, a particularly vital function when the clinical demand surpasses the available capacity.
The characterization of MTS as a "clinical risk management" tool elevates its function beyond that of a mere sorting mechanism. This terminology implies a proactive and systematic methodology aimed at identifying, assessing, and mitigating potential adverse outcomes that could arise from delays in care for patients with high-acuity conditions. In the high-pressure context of an emergency department (ED), the principal risk is patient deterioration or harm stemming from deferred or inappropriate medical attention. By standardizing the assessment of urgency, MTS endeavors to control this risk, ensuring that the "sickest are seen first," which is a foundational principle of contemporary patient safety initiatives.
Furthermore, a critical delineation of the MTS's scope is its design focus on prioritizing patients for their first contact with a physician, not for predicting the need for admission, forecasting resource utilization, determining a definitive diagnosis, or directing the patient to a final care stream or destination. This distinction addresses a common point of confusion regarding the capabilities of triage systems. While EDs often face operational pressures to make such comprehensive predictions early in the patient journey, the MTS is specifically tailored to address the immediate question: how quickly does this patient need to be seen by a doctor? Subsequent clinical decisions regarding diagnosis, admission, and resource allocation necessitate further, more detailed assessment that extends beyond the purview of initial triage. This positions MTS as an essential, but singular, component within a broader continuum of patient flow and clinical decision-making processes within the emergency department.
The Rationale for Standardized Triage in Emergency Care
The imperative for standardized triage systems in contemporary emergency care is deeply rooted in historical precedent and the evolving challenges of modern healthcare. The concept of triage itself, with origins tracing back to battlefield medicine in the late 18th and early 19th centuries, highlights a long-recognized necessity to prioritize care when demand overwhelms available resources, particularly in mass casualty situations. Modern emergency departments, while distinct from battlefields, face analogous pressures stemming from increasing patient volumes, ED overcrowding, and the diverse spectrum of patient acuities and presentations.
In the absence of standardized protocols, triage decisions can be inconsistent and highly subjective, potentially leading to inequitable or unsafe care. Standardized systems like the MTS aim to supplant these variable assessments with an objective, reproducible, and evidence-informed methodology. The core rationale is to ensure fairness in access to care and to optimize the allocation of finite healthcare resources by systematically identifying and prioritizing patients with the most urgent clinical needs—effectively "treating the sickest first".
The evolution of triage from its initial focus on surgical and trauma casualties in mass casualty scenarios to the comprehensive systems required in modern EDs reflects a significant shift in the landscape of emergency medicine. Contemporary triage tools must be capable of managing the full spectrum of clinical presentations, from critical illness and major trauma to minor injuries and illnesses, across all age groups, from neonates to the very elderly. This necessitates systems that are both broad in scope and adaptable to diverse patient needs, moving beyond purely life-or-limb-threatening criteria to encompass a wider understanding of clinical urgency.
A fundamental operational principle underpinning effective triage is its dynamic nature; a patient's clinical status can change rapidly, and the initial triage assessment represents a snapshot in time. Consequently, the priority level assigned by the MTS is not immutable. The system inherently requires continuous reassessment of waiting patients, particularly if their condition evolves or if the target timeframes for physician contact are breached. In such instances, a formal "secondary assessment" is mandated to document the patient's ongoing status and adjust the priority level if necessary. This dynamic aspect has significant implications for ED staffing, workflow design, and the continuous monitoring of patients in the waiting area, ensuring that changes in clinical urgency are promptly recognized and acted upon.
2. Genesis and Evolution of the MTS
Origins and Development in Manchester
The Manchester Triage System emerged from the specific clinical environment of Manchester, England, during the 1990s. Its development was a direct response to concerning observations made in 1994 regarding "surprising and inconsistent triage decisions" across various emergency departments. A particularly illustrative case, involving a 26-year-old pedestrian involved in a road traffic accident who sustained bilateral tibial and fibular fractures yet waited five hours in a minor treatment area without intervention, starkly highlighted the existing systemic deficiencies.
This incident, and others like it, catalyzed local consultations among emergency care clinicians, revealing a widespread problem and a collective desire for a standardized, common solution. A subsequent local review confirmed the pervasive lack of consistency in triage practices. In response, The Manchester Triage Group was established in 1995, a collaborative body comprising all local Emergency Physicians and Emergency Nurses. The group's explicit aim was to create and implement a unified system encompassing common nomenclature for urgency levels, precise definitions for these levels, a standardized assessment methodology, comprehensive teaching programs, and robust audit processes to ensure quality and consistency in triage.
The impetus for MTS development being problem-driven and clinician-led is a noteworthy aspect of its history. This bottom-up approach, originating from the very professionals who would ultimately use and be judged by the system, likely played a significant role in its practical design, clinical relevance, and subsequent widespread adoption. Systems designed by end-users are inherently more likely to address real-world operational needs and gain acceptance among peers, thereby facilitating smoother implementation and greater adherence.
Furthermore, the initial comprehensive focus of The Manchester Triage Group extended beyond merely creating a set of rules. They established an entire framework for the system's application, including the crucial elements of common terminology, defined assessment processes, dedicated training materials, and integrated audit mechanisms. This holistic, systems-thinking approach from the project's inception recognized that a clinical tool, however well-designed, is insufficient in isolation. Its successful and consistent application depends heavily on standardized support structures, acknowledging that human factors, education, and ongoing quality assurance are as vital as the instrument itself. This comprehensive vision laid a strong foundation for the MTS's subsequent refinement and dissemination.
Key Milestones and Subsequent Editions
The Manchester Triage Group meticulously defined the core components of the system. They established five distinct priority levels, each assigned a specific name, a corresponding color code for easy visual identification, and a maximum target time within which a patient should be assessed by a physician. Integral to the system's sustainability and quality, they also developed standardized training packages, including manuals for users and instructors, and designed audit processes for both individual practitioner performance and institutional adherence. The individual audit goals were ambitious, aiming for 0% incomplete episodes and 95% accuracy.
The MTS has not remained static since its inception; it has been subject to ongoing evolution and refinement. A significant development was the release of a Second Edition, which entailed a thorough review of existing flowchart titles and content, an update of discriminators, the introduction of new flowcharts to address presentations such as Allergy, Palpitations, and Falls, and revisions to existing charts (e.g., changing "Haematological D,V" to "D&V" and "Nasal problems" to "Facial Problems").
Responsibility for the continued development of the MTS now rests with the International Reference Group, which bases system modifications on empirical studies and clinical evidence. National reference groups in various countries are then tasked with translating these agreed-upon changes and adapting them to local health policies and contexts. A pragmatic distinction is made between "urgent" and "non-urgent" changes to the system, with urgent modifications, particularly those impacting patient safety or core functionality, prioritized for timely implementation within IT systems. The official MTS website, triagenet.net, serves as a central repository for information and emphasizes the critical importance of healthcare organizations keeping their MTS implementations current with the latest supported editions.
The system has also seen specific adaptations for distinct patient populations and contexts. Notably, modifications for pediatric emergency care have been extensively studied and proposed, leading to the development of specific pediatric versions such as MTS Version 1 (discriminator modifications) and MTS Version 2 (incorporating vital signs). Professor Janet Marsden is recognized as one of the key founders of the MTS, highlighting the significant individual contributions to this influential system.
The establishment of the International Reference Group and associated national bodies signifies a mature, structured, and evidence-based governance model for the ongoing evolution and international adaptation of MTS. This framework is crucial for maintaining the system's clinical relevance, safety, and consistency as it is adopted across diverse healthcare systems worldwide. It ensures that modifications are driven by research rather than arbitrary decisions and allows for necessary localization while preserving the core principles of the MTS. The practical approach of categorizing IT updates into urgent and non-urgent reflects an understanding of the complexities involved in modifying clinical decision support systems within hospitals, ensuring that safety-critical updates are expedited.
Moreover, the diversification of the MTS into specialized tools—such as Telephone Triage, Nursing and Residential Triage (NaRT), Pre-Hospital Pathfinder, and the Community Triage Tool —alongside specific pediatric versions, demonstrates a sophisticated recognition that a singular, one-size-fits-all approach to triage is inadequate. Different patient populations (e.g., children, elderly residents in care homes) and varied assessment contexts (e.g., telephone advice versus face-to-face emergency department presentation) necessitate nuanced methodologies and specifically adapted discriminators to ensure the validity, safety, and effectiveness of the triage process.
3. The MTS Framework: Methodology and Application
Presentational Flowcharts: Structure and Rationale
The Manchester Triage System is structured around a series of standardized presentational flowcharts. Sources indicate either 53 "Emergency Triage charts" or 52 such flowcharts. A core tenet of these flowcharts is that they are "presentation, not diagnosis based". This means the selection of a flowchart is guided by the patient's stated reason for seeking care—their chief complaint or presenting problem—rather than an attempt to prematurely diagnose their condition. Examples of flowchart titles include common presentations like "Headache," "Shortness of breath," "Wounds" , as well as broader categories such as "Unwell adult" or "Abnormal behaviour".
The MTS employs a "reductive" methodology, meaning that all patients are conceptually considered to be at the highest priority level (Priority 1) at the outset of the triage assessment. The triage nurse then works through the selected flowchart to actively rule out criteria for higher urgency levels before a lower priority can be assigned. The selection of the most appropriate flowchart, based on the patient's primary presenting problem, constitutes the initial step in the triage process. This choice then directs the nurse to a specific, ordered set of discriminators relevant to that presentation.
The principle of being "presentation, not diagnosis based" is fundamental to the MTS's design and usability. It empowers nurses to conduct effective triage assessments without the necessity of establishing a definitive medical diagnosis, an activity often unfeasible or inappropriate at the initial point of contact in a busy ED. This approach accelerates the triage process and maintains focus on the severity of symptoms and signs, which aligns with the nurse's scope of practice and the time-sensitive nature of emergency care. By categorizing based on observable phenomena or patient reports (e.g., "chest pain") rather than diagnostic labels (e.g., "myocardial infarction"), the system facilitates rapid, standardized risk stratification.
The "reductive" nature of the MTS, wherein patients are initially presumed to be Priority 1 , serves as an inherent safety mechanism. The onus is on the triage nurse to systematically consider and exclude discriminators indicative of higher urgency before settling on a lower priority category. This default to higher acuity ensures that the most critical conditions are actively considered first, minimizing the likelihood of under-triaging a patient with a life-threatening problem.
The Role of Discriminators: General and Specific
Within each presentational flowchart, the decision-making process is guided by a series of "discriminators." These are specific clinical signs, symptoms, or relevant anamnestic data points that indicate varying levels of urgency. Discriminators are meticulously ranked by priority within each flowchart, meaning that the most critical indicators are assessed first.
MTS utilizes two main types of discriminators:
General Discriminators: These are indicators of potentially severe physiological compromise or high-risk features that appear across multiple, if not all, flowcharts. Examples include "Airway compromise," "Active Seizure," "Severe pain," "Hot child" (fever), altered level of consciousness, and extreme derangements in vital signs. A key feature of general discriminators is that they consistently assign the patient to the same high-urgency level, regardless of the specific presentational flowchart being used.
Specific Discriminators: These pertain to signs and symptoms more narrowly associated with particular groups of presentations or specific flowcharts. For example, a discriminator related to "sudden onset of neurological deficit" might be prominent in the "Stroke" or "Neurological Problems" flowchart but not in a "Minor Injury" flowchart.
The triage process involves the nurse systematically assessing the patient against these discriminators. The selection of any positive discriminator effectively halts the triage process at that point, and the patient is allocated to the urgency category linked to that specific discriminator. For IT system implementations of MTS, the predefined order of discriminators within each presentation is binding, ensuring a consistent and logical assessment pathway.
The concept of general discriminators, which consistently yield the same urgency level irrespective of the flowchart context, is a cornerstone of the MTS's simplicity and contributes significantly to its inter-rater reliability. For instance, a patient exhibiting clear signs of "Airway compromise" will invariably be triaged to the highest urgency category (Red), whether their initial presenting complaint was "shortness of breath," "allergic reaction," or "trauma." This standardization for universally critical conditions simplifies the learning curve for nurses and reduces ambiguity in application, thereby enhancing the consistency of triage decisions.
Furthermore, the mandated binding order of discriminators within flowcharts reinforces the system's reductive and safety-oriented design. Triage nurses are compelled to systematically evaluate and exclude higher-urgency conditions before they can consider assigning a patient to a lower-urgency category. For example, in a "Chest pain" flowchart, discriminators related to hemodynamic instability or acute ischemic changes will be positioned and must be assessed before those indicative of less immediately life-threatening causes. This structured, hierarchical approach ensures a methodical search for red flags, aligning with the "reductive" principle and minimizing the probability of overlooking a critical symptom or sign.
Assigning Clinical Priority: The Step-by-Step Process
The practical application of the Manchester Triage System by the triage nurse follows a defined, sequential process. Ideally, the triage assessment is conducted immediately upon the patient's arrival at the emergency department, preferably even before administrative registration processes are completed, to ensure prompt identification of high-risk individuals.
The process unfolds as follows:
Flowchart Selection: Based on the patient's chief complaint or primary reason for seeking emergency care, the triage nurse selects the most appropriate presentational flowchart from the available set.
Discriminator Assessment: The nurse then systematically works down the list of discriminators presented within that chosen flowchart. This assessment must follow the predefined order of the discriminators, starting with those indicative of the highest urgency.
Priority Assignment: If a discriminator is found to be positive (i.e., the patient meets the criteria for that discriminator), the triage process stops at that point. The patient is then assigned the clinical priority level (e.g., Red, Orange, Yellow, Green, Blue) that is directly associated with that specific positive discriminator.
Time Window Allocation: This assigned urgency level dictates the maximum permissible time window within which the patient should have their first contact with a physician or, in some interpretations, an advanced practice provider. It is critical to note this target time is for first assessment, not necessarily the commencement of definitive treatment.
Documentation: The documentation of excluded discriminators (i.e., those assessed as negative) is not typically performed on an individual basis for each negative finding. Instead, a "summary confirmation" is made at each level of priority, indicating that all higher-level discriminators were considered and found to be absent before the chosen priority level was assigned.
The "summary confirmation" approach to documenting excluded discriminators represents a pragmatic balance between the need for thoroughness in assessment and the demand for speed and efficiency in a high-volume ED setting. This method implies a cognitive checklist process undertaken by the nurse, where they mentally (or guided by the IT system) review and rule out more urgent criteria before arriving at the final priority. While more efficient than exhaustive documentation of every negative finding, it still presupposes a systematic and comprehensive review, which is crucial for maintaining patient safety.
The ideal of conducting the triage assessment "before the patient's administration" highlights a potential point of tension with traditional hospital administrative workflows, which often prioritize registration and data collection upfront. The MTS philosophy, however, unequivocally prioritizes rapid clinical risk assessment to ensure that critically ill patients are identified without delay. This suggests that ED operational processes should be designed to facilitate immediate clinical triage upon patient arrival, potentially necessitating a re-evaluation and adaptation of conventional patient intake procedures to align with this clinical imperative.
The Five Priority Levels: A Detailed Examination
The MTS categorizes patients into five distinct priority levels. Each level is associated with a specific color code for immediate visual recognition and, crucially, a maximum target time within which the patient should have their initial assessment by a healthcare professional, typically a physician. It is important to reiterate that this target time refers to the first physician contact and not necessarily the initiation of definitive treatment.
The five priority levels are detailed in Table 1 below:
Table 1: MTS Priority Levels, Target Times, and Clinical Descriptors
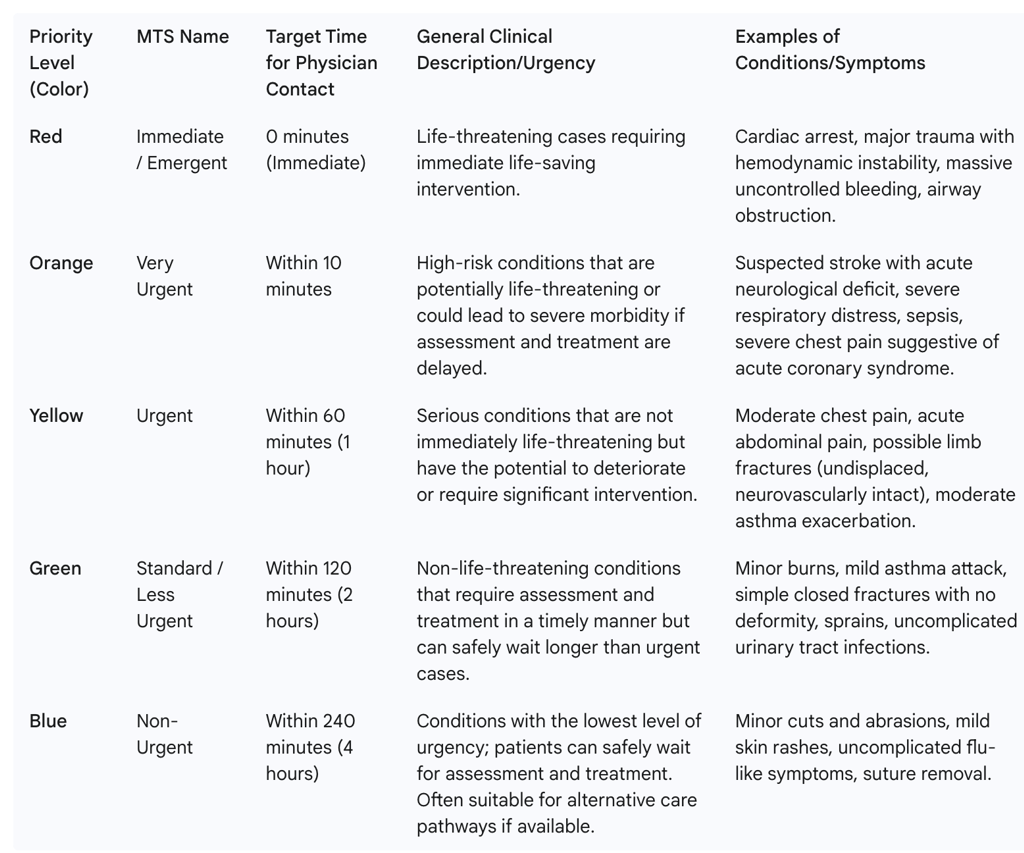
The explicit definition of target times for first physician contact, rather than the commencement of treatment , is a critical nuance of the MTS. Meeting this initial contact target signifies adherence to the MTS-defined timeframe for that urgency level. However, it does not guarantee that comprehensive treatment will begin immediately thereafter. Subsequent delays can still occur due to various factors, including the need for diagnostic tests, specialist consultations, or the availability of inpatient beds. Understanding this distinction is vital for setting realistic expectations regarding what the MTS aims to achieve and for recognizing the importance of measuring other downstream process times within the ED to gain a complete picture of patient flow and efficiency.
The inclusion of a "Blue/Non-Urgent" category with a 4-hour target wait time indicates that the MTS is designed to accommodate a very broad spectrum of patient acuities, including those whose conditions might, in some healthcare systems, be more appropriately managed in primary care or urgent care settings. The presence of such low-acuity patients in EDs is a common reality. This category can contribute to ED crowding if these patients consume significant resources or staff attention that could otherwise be directed towards higher-acuity cases. However, it also underscores the potential utility of the MTS at a "common counter" or single point of entry, where it can be used to stream patients effectively to the most appropriate service, such as an out-of-hours primary care clinic that may be co-located with or integrated into the ED services.
4. Implementation and Scope of MTS
Adoption in Emergency Departments
The Manchester Triage System is engineered for broad applicability across diverse emergency care settings. It is suitable for implementation in hospitals of all care levels, from large tertiary referral centers to smaller community hospitals, and across various organizational models, including dedicated emergency rooms (NA) and mixed elective/emergency outpatient clinics. This inherent flexibility has contributed to its status as one of the world's most extensively utilized systems for determining clinical priority based on urgency. The system's design, which accommodates a wide range of patient presentations and institutional sizes, suggests a high degree of scalability and adaptability. This characteristic is a significant factor in its widespread international adoption, as it obviates the need for fundamentally different triage systems for different hospital contexts, allowing for a degree of standardization in approach and training.
MTS in Pediatric Emergency Care
The MTS is widely implemented in pediatric emergency departments, although its application in this specific population presents unique challenges and has been subject to considerable study and adaptation. Of the standard MTS flowcharts, 49 are considered applicable to children. Research has characterized its use in pediatric settings, identifying frequently used flowcharts such as "worried parents" (accounting for 22.4% of presentations in one study) and prevalent discriminators like "recent event" (15.3% in the same study). Patient outcomes, including hospitalization rates (e.g., 10.4% in one pediatric ED study) and the need for periods of observation, are often tracked in conjunction with MTS categorization.
However, the validity of the standard MTS in pediatric populations has often been described as "moderate". A consistent finding is that the system tends to err on the side of caution, resulting in significantly more over-triage (assigning a higher urgency level than clinically necessary) than under-triage (assigning a lower urgency level than clinically necessary). This pattern is particularly evident in younger children and those presenting with medical problems as opposed to trauma, where triage assessment can be especially challenging. The common utilization of the "worried parents" flowchart in conjunction with the observed high rates of over-triage suggests a potential causal relationship. Parental anxiety, while a valid concern, is a subjective factor that may influence nurses to select higher urgency categories, particularly when assessing non-verbal infants or young children where objective signs may be subtle. This highlights an inherent tension between subjective inputs and objective clinical assessment in pediatric triage.
In response to these challenges, specific modifications to the MTS for pediatric use have been developed and evaluated. An international multicenter study examined two such modified versions: MTS Version 1, which incorporated specific discriminator modifications, and MTS Version 2, which added the consideration of vital signs. MTS Version 1, which included age-specific adjustments to discriminators like "hot child" (fever), "persistent vomiting," "not feeding," "prolonged or uninterrupted crying," "scalp hematoma," "unable to talk in sentences," and "wheeze," demonstrated slightly improved performance compared to the original MTS. This was particularly notable for febrile children, where reclassification occurred in 46% of patients, leading to significant increases in diagnostic odds ratio and c-statistic without an increase in under-triage. Conversely, MTS Version 2, which involved the addition of vital signs as overarching discriminators, did not show a significant improvement in triage performance. This outcome suggests that targeted, evidence-based refinements to existing clinical rules within the MTS framework are likely more effective than simply incorporating additional data points, especially if those data are not integrated in a nuanced, context-specific manner. The inherent difficulties in triaging very young children and those with complex medical presentations underscore the limitations of a general triage system when applied to highly specialized subpopulations, reinforcing the continuous need for focused research, system refinement, and specialized training for staff working in pediatric emergency care.
Broader Applications: Telephone Triage, Nursing Homes, Community Settings
The core principles and framework of the Manchester Triage System have demonstrated adaptability beyond the traditional physical emergency department, leading to the development of specialized MTS tools for a variety of other healthcare contexts:
MTS Telephone Triage and Advice: This adaptation utilizes the same fundamental principles, presentational charts, assessment methodology, and discriminator definitions as the standard Emergency Triage system. It is designed for use by Ambulance Services for emergency call handling and by other clinical telephone triage services to provide remote assessment and advice. A notable implementation was in the Azores in 2013, where it was integrated into the management of emergency calls, contributing to an award-winning system for ensuring appropriate care dispatch. However, it is important to note that some research has indicated that telephone triage, when implemented in isolation, may require further refinement and validation to ensure its safety and effectiveness, as remote assessment inherently lacks visual cues and the ability for physical examination.
Nursing and Residential Triage (NaRT): Specifically developed from the MTS Emergency Triage 3rd edition, NaRT is tailored to support nursing and care staff working in nursing homes and residential care facilities in assessing acute changes in residents' conditions and determining the need for escalation or transfer to emergency services.
Pre-Hospital Pathfinder: This tool is designed for use by Ambulance Service personnel during face-to-face patient contact in the pre-hospital environment, guiding assessment and decisions regarding the most appropriate care pathway or destination.
Community Triage Tool: This version of MTS is intended for use by community-based healthcare teams, including first response assessment teams and providers of pendant alarm services, to facilitate risk assessment and appropriate care routing for individuals in community settings.
The expansion of the MTS into these diverse settings, particularly telephone and community-based triage, reflects a broader strategic trend in healthcare towards pre-hospital risk assessment and more effective patient streaming. The aim is often to manage demand on busy emergency departments by directing patients to the most appropriate level of care from the earliest point of contact. The success of these adaptations critically depends on the ability to maintain the core MTS principles of safety, consistency, and evidence-based decision-making, even when applied in different modalities or by staff with varying levels of acute care experience. The caution raised regarding telephone triage highlights that direct transposition of ED-based tools to new contexts requires careful validation and may necessitate different supporting processes, specialized training, or modified discriminator sets to account for the unique challenges of each setting.
Global Reach and Variations
The Manchester Triage System has achieved significant international penetration, particularly across European countries where it is widely used and often considered a de facto standard. Its adoption has been noted in numerous nations, including the United Kingdom (its origin), the Netherlands, Sweden, and Portugal, with studies also documenting its validation and use in countries like Italy and by Brazilian healthcare institutions. The official MTS website, triagenet.net, plays a crucial role in facilitating its global dissemination by providing access to resources, training information, and updates.
Despite its widespread use in high-income countries, the direct applicability of five-tier triage systems like MTS in low- and middle-income countries (LMICs) has been questioned. The differing epidemiological profiles, variations in service demands, and, most critically, disparities in resource availability in LMICs may render systems developed in resource-rich environments less suitable. This has led to the development and promotion of alternative or adapted triage tools, such as the Interagency Integrated Triage Tool, specifically designed for use in low-resource settings. The underlying assumptions of the MTS regarding the availability of physicians within specified target times, access to diagnostic capabilities, and capacity for intervention may not consistently hold true in all global healthcare contexts. This necessitates a careful consideration of local conditions before implementation and may favor simpler, contextually adapted triage tools in LMICs.
Even within high-income countries that have adopted the MTS, a degree of localization is often necessary. The existence of national reference groups tasked with the translation and adaptation of MTS changes to align with national health policies and linguistic requirements underscores this point. While the core methodology aims for international standardization, effective implementation requires sensitivity to local factors. These can include language, nuances in healthcare-seeking behaviors, the structure of the national health system, and specific health policy directives. This reflects a dynamic balance between maintaining the integrity of an internationally recognized standard and ensuring its practical applicability and cultural resonance within diverse national healthcare landscapes.
IT System Integration and Requirements
In modern emergency departments, the effective and consistent implementation of the Manchester Triage System frequently involves its integration into computerized Hospital Information Systems (HIS) or dedicated ED information systems. Such integration is not merely a matter of convenience but is critical for maintaining the fidelity and safety of the triage process. There are stringent requirements for how MTS should be mapped into IT systems to ensure its logic is accurately reflected and consistently applied.
It is considered imperative that all approved presentational flowcharts and their associated discriminators, including any explanatory notes or definitions, are implemented unchanged within the IT system. Any deviation, alteration, or omission could inadvertently modify the triage logic, potentially leading to incorrect priority assignments and compromising patient safety. Furthermore, the predefined order of discriminators within each flowchart is binding and must be strictly adhered to in the IT system's configuration. This ensures that the systematic, reductive assessment process, which prioritizes the exclusion of more critical conditions first, is maintained.
Another specific requirement for IT mapping is the correct display of the "risk limit" (German: ‘Risiko-Grenze’) within the relevant diagrams or interfaces presented to the triage nurse. While the precise nature of this "risk limit" is not fully elaborated in the provided materials, its mandated inclusion suggests it serves as an important visual or logical cue within the IT application. It may represent a threshold or a specific combination of factors that, when approached or met, indicates a patient is nearing or crossing into a higher urgency category, thereby aiding the nurse's decision-making and risk assessment.
The documentation of the triage assessment within the IT system also follows a specific MTS principle: the exclusion of discriminators by the user is not recorded individually for each negative finding. Instead, a "summary confirmation" is documented at each level of priority assigned. This confirms that all higher-level discriminators were considered and excluded before the final priority was determined. Finally, when updates or changes to the MTS are released by the International Reference Group, those designated as "urgent" are expected to be implemented within the hospital's IT systems in a timely manner to ensure that practice remains aligned with the most current, evidence-based version of the tool. These rigorous IT requirements underscore the understanding that the computerized system is not a passive repository of information but an active component of the clinical decision support process in triage, and its accuracy and fidelity are paramount for patient safety.
5. Evaluating MTS: Validity, Reliability, and Performance
Assessing Validity: Sensitivity, Specificity, and Predictive Value
The validity of the Manchester Triage System—its ability to accurately measure true patient urgency—has been a subject of extensive research. Assessments typically involve comparing the urgency levels assigned by triage nurses using MTS against an independent reference standard. This reference standard may be derived from expert panel consensus, patient outcomes such as admission to an Intensive Care Unit (ICU) or mortality, or a composite of clinical variables.
Studies have yielded a range of validity estimates, often varying by patient population and study setting:
For adult patients:
When predicting ICU admission or death at the ED, sensitivity has been reported to range from 0.80 to 0.86, with specificity ranging from 0.84 to 0.91.
Using a 3-category reference standard for overall urgency, sensitivity for detecting high-urgent adult patients has ranged from 0.47 to 0.87, while specificity has ranged from 0.84 to 0.94.
For pediatric patients:
For ICU admission or death, sensitivity has ranged from 0.66 to 0.91, with specificity from 0.82 to 0.87.
Against a 3-category reference standard, sensitivity for high-urgent children ranged from 0.65 to 0.83, and specificity from 0.83 to 0.89.
The MTS is generally considered to be highly sensitive in identifying critically ill patients and those presenting with conditions such as acute cardiac chest pain. Furthermore, it has demonstrated utility as a good predictor of the need for hospitalization and of subsequent hospital mortality. Diagnostic odds ratios, which provide an overall measure of test performance, have been reported to range from 13.5 to 35.3 in adult populations and from 9.8 to 23.8 in children. However, a consistent finding across multiple studies is that MTS performance can vary considerably between different emergency departments and tends to be lowest in the youngest pediatric patients and in elderly patients.
Table 2 provides a summary of key metrics from various studies evaluating the validity and reliability of the MTS.
Table 2: Summary of MTS Validity and Reliability Studies (Key Metrics)
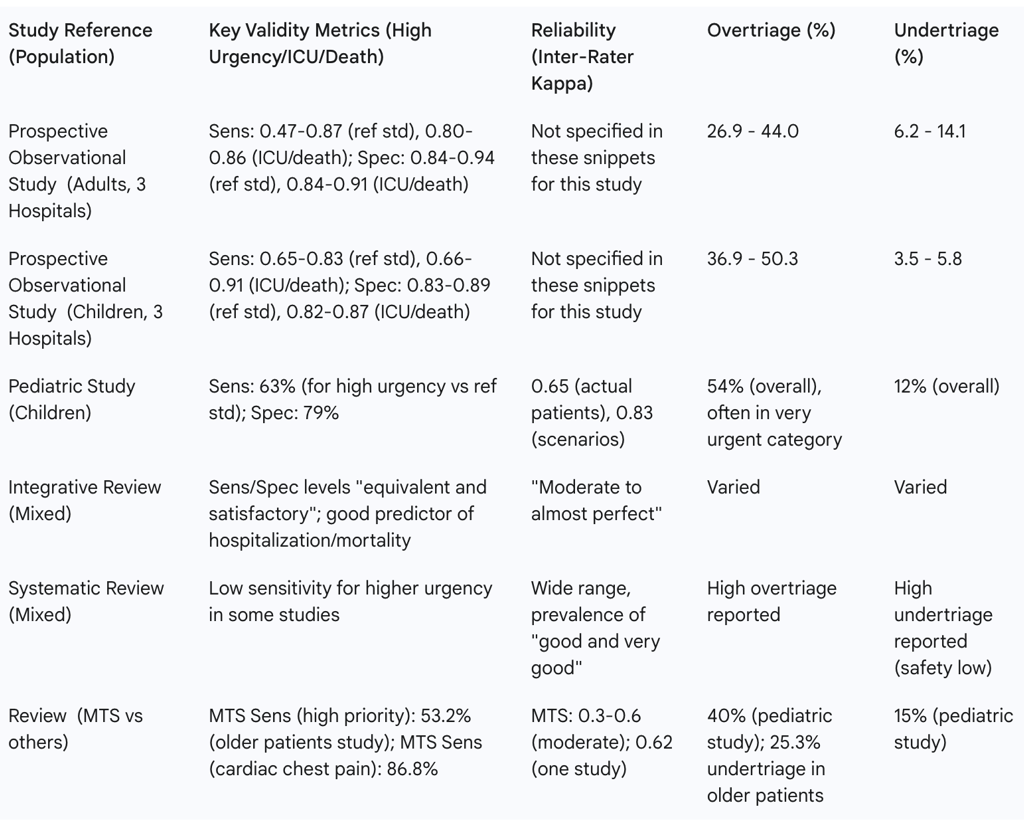
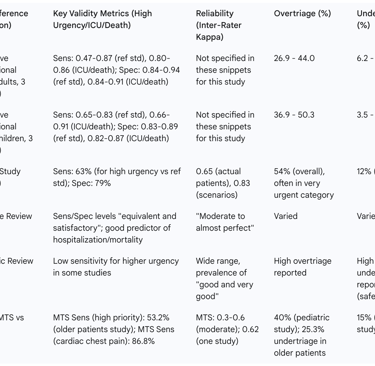
The overall assessment of MTS validity is often characterized as "moderate to good". However, the notable variation in performance metrics observed across different EDs, even when ostensibly using the same triage tool , strongly suggests that local implementation factors play a crucial role. These factors can include the quality and consistency of staff training, the rigor of audit and feedback mechanisms, staffing levels and experience, the case mix of the patient population, and the fidelity of adherence to the MTS protocol. This implies that the tool itself is only one component influencing its real-world effectiveness; the context of its application is equally important.
A recurring theme in validity studies is the diminished performance of MTS in the youngest pediatric patients and in elderly individuals. These demographic extremes often present with atypical symptoms, face communication challenges, and may have different physiological reserves or responses to illness, making standardized triage assessment more complex. This vulnerability highlights a need for specific considerations, potential modifications, or adjunct tools when triaging these populations.
While the MTS generally demonstrates good predictive value for serious outcomes like hospitalization and mortality , its sensitivity for identifying all high-urgency patients is not absolute. For instance, some studies report sensitivities for detecting high-urgent adults as low as 0.47 in particular hospital settings. This indicates that a proportion of genuinely urgent patients may be initially misclassified into lower urgency categories, which poses a potential patient safety risk due to delayed assessment and intervention. This "miss rate" is a key focus for ongoing system improvement efforts.
Reliability and Inter-Rater Agreement
The reliability of a triage system, particularly its inter-rater agreement (the consistency of triage decisions made by different nurses for similar patient presentations), is a critical determinant of its utility. If different assessors assign varying priority levels to comparable patients, the standardization and fairness sought by the system are undermined.
Studies evaluating the inter-rater reliability of the MTS have reported a range of findings. Some reviews describe it as "moderate to almost perfect" or generally "good". However, other analyses, particularly those using the kappa statistic, have placed MTS inter-rater reliability in the "moderate" range, with kappa values often cited between 0.3 and 0.6. In contrast, one pediatric study reported a weighted kappa of 0.83 for written case scenarios (indicating very good agreement) but a lower kappa of 0.65 for simultaneous triage of actual patients in the ED (moderate to good agreement). Some comparative reviews have suggested that other systems like the Canadian Triage and Acuity Scale (CTAS) or the Emergency Severity Index (ESI) may achieve higher inter-rater reliability in certain studies.
This variability in reported inter-rater reliability for the MTS suggests that while the system provides a structured framework, its consistent application is significantly influenced by factors beyond the tool itself. The quality and standardization of training programs, the clinical experience of the triage nurses, strict adherence to the defined protocols and discriminator definitions, and the effectiveness of ongoing audit and feedback mechanisms all play a substantial role in achieving and maintaining high levels of consistency. Attaining robust inter-rater reliability is not a one-time achievement but requires continuous effort and quality improvement initiatives.
The observation that reliability tends to be higher in controlled settings, such as when assessing written case scenarios, compared to the dynamic environment of actual patient triage , is an expected finding. Written scenarios provide complete and unambiguous information, free from the pressures of a busy ED. Real-world triage, however, is often characterized by incomplete patient histories, communication barriers (e.g., language differences, altered mental status), high workload, frequent interruptions, and significant time constraints. These complexities can impact the consistency of decision-making. This underscores the importance of practical, simulation-based training that mirrors real-world challenges, alongside efforts to optimize the ED work environment to support accurate and reliable triage.
The Challenges of Over-triage and Under-triage
Two primary types of classification errors are associated with any triage system: over-triage and under-triage. Both are documented challenges with the Manchester Triage System, each carrying different implications.
Over-triage occurs when a patient is assigned a higher urgency level than their clinical condition objectively warrants. This is frequently reported as being more common than under-triage with the MTS. It is particularly prevalent in pediatric populations, where over-triage rates of 40% to 54% have been observed in some studies. While potentially erring on the side of safety by ensuring patients are seen promptly, systematic over-triage can lead to inefficient use of ED resources, increased workload for staff attending to non-critical patients, and potentially longer waiting times for other appropriately triaged urgent patients.
Under-triage involves assigning a patient a lower urgency level than is appropriate for their actual clinical condition. This is a more significant patient safety concern, as it can lead to critical delays in assessment and treatment for patients with serious or life-threatening conditions, potentially resulting in deterioration, adverse outcomes, or even mortality. Reported under-triage rates with MTS vary. Some comparative studies in adult populations have shown rates between 11% and 20%. One pediatric study found an overall under-triage rate of 12%. Certain patient groups appear more vulnerable to under-triage, including children with abnormal vital signs and older adult patients, where under-triage rates as high as 25.3% have been noted in specific study cohorts.
The tendency for the MTS, particularly in pediatric applications, to "err on the safe side" by producing more over-triage than under-triage may reflect either a deliberate design philosophy embedded within its pediatric flowcharts and discriminators or a behavioral adaptation by triage nurses. When faced with uncertainty, especially in vulnerable populations like children, clinicians may opt for a higher urgency category as a precautionary measure. While this approach aims to maximize sensitivity (i.e., not missing critically ill patients), it does so at the expense of specificity (i.e., correctly identifying patients who are not severely ill), leading to the aforementioned resource inefficiencies.
Although often less frequent than over-triage, under-triage carries a substantially higher immediate risk to patient safety. The identification of specific patient characteristics or clinical factors consistently associated with under-triage—such as abnormal vital signs in children or advanced age —is crucial for developing targeted interventions. These might include enhanced training modules focusing on these risk factors, refinement of relevant discriminators within the MTS, or the implementation of clinical decision support alerts.
The persistence of both over-triage and under-triage, despite the use of a highly structured and standardized system like MTS , underscores the ongoing influence of human factors and systemic pressures on triage accuracy. Elements such as decision-making under pressure, cognitive biases, individual clinician experience , and prevailing resource constraints within the ED can all contribute to classification errors. This implies that strategies to improve triage accuracy must extend beyond merely refining the tool itself; they must also address human factors engineering, optimize the work environment, and ensure adequate staffing and resources.
Impact on ED Efficiency: Waiting Times, Length of Stay, and Patient Flow
The influence of the Manchester Triage System on key emergency department efficiency metrics, such as waiting times and length of stay (LOS), is complex and not always straightforward. A prospective before-and-after study investigating the impact of MTS implementation found that while the overall median waiting time for patients did not significantly decrease after MTS was introduced, the distribution of waiting times across the different urgency levels improved. Specifically, patients assigned to higher urgency categories experienced shorter waits, while those in lower urgency categories waited longer, which aligns with the system's primary goal of prioritization.
However, the same study reported that for admitted patients, both treatment time (time from entering the treatment room to admission) and the subsequent inpatient length of stay were significantly longer after MTS implementation, although the total ED LOS (from registration to discharge or admission) did not show an overall significant difference. Other research suggests that MTS can contribute to improved patient flow management generally , and there is consistent evidence that higher MTS priority categories are strongly associated with increased utilization of ED resources (e.g., diagnostic tests, procedures) and a higher likelihood of hospital admission.
The observation that MTS may not necessarily reduce overall ED waiting times but rather redistributes these times according to clinical urgency is a critical finding. It underscores that the fundamental objective of MTS is to ensure that the sickest patients are seen first, not necessarily to make every patient wait less time. Therefore, evaluating the success of MTS solely on its ability to decrease average waiting times might be a misapplication of its intended purpose. Its effectiveness in this domain lies more in achieving appropriate prioritization according to clinical need.
The counterintuitive finding of increased treatment times and subsequent inpatient LOS for admitted patients following MTS implementation in one study warrants careful consideration. Several factors could contribute to this observation. Firstly, if MTS is more effective at identifying sicker patients who genuinely require more intensive and prolonged treatment, then longer treatment times and LOS would be an expected consequence of better case identification. Secondly, it is possible that while triage itself became standardized, downstream ED processes—such as diagnostic turnaround times, availability of specialist consultations, or inpatient bed allocation—were not sufficiently optimized to handle the newly prioritized patient flow, leading to internal delays. The authors of that study concluded that implementing MTS in isolation is not sufficient to improve the overall efficiency and quality of EDs, suggesting that triage is but one component in a complex system requiring holistic process redesign.
The consistent association between higher MTS priority levels and increased resource utilization and hospitalization rates serves as an important form of predictive validity. It suggests that, on the whole, the system is successfully differentiating patients based on the severity of their condition and their genuine need for more intensive investigation and care. This correlation indicates that MTS is generally effective in identifying those patients who will ultimately require more significant healthcare interventions.
Patient Safety Outcomes: Mortality and Adverse Events
A critical dimension for evaluating any triage system is its impact on patient safety, particularly its ability to identify patients at high risk of mortality or other serious adverse events. The Manchester Triage System has been identified in multiple studies as a good predictor of in-hospital or short-term mortality. Patients assigned to the higher priority categories (Red, Orange, and often Yellow) consistently demonstrate a significantly higher risk of death compared to those in lower priority categories. For instance, one study reported that 96.6% of patients who subsequently died had been triaged to MTS priority 1 (Red) or 2 (Orange). This strong correlation between high MTS urgency and mortality is a powerful validation of the system's capacity to flag patients who are critically ill and at imminent risk, which is arguably one of its most vital functions.
However, while the system demonstrates good predictive capability at a population level, errors in triage, especially under-triage, can have severe consequences for individual patients. Such errors can lead to delays in essential medical assessment and treatment, potentially resulting in patient deterioration, preventable harm, and an increased risk of mortality. The high stakes associated with triage accuracy mean that even if the system performs well on average, individual errors can lead to catastrophic outcomes. This underscores the imperative for robust quality assurance measures, continuous professional development for triage staff, and ongoing efforts to refine the system to minimize such errors. The link between triage inaccuracies and adverse patient outcomes reinforces that striving for the highest possible accuracy in MTS application is a fundamental patient safety imperative.
Patient Satisfaction with MTS
Patient satisfaction is an increasingly recognized component of healthcare quality, and the implementation of a structured triage system like MTS can have a mixed impact on this dimension. A notable before-and-after study found that following the introduction of MTS, patient satisfaction with the length of waiting time and with the feeling that their problem had been sorted out actually scored better. This suggests that patients may perceive the prioritization process as fairer or that improved outcomes for some contributed to higher satisfaction in these areas.
Conversely, the same study reported that patient satisfaction with the provision of information during the triage process and with the opportunity to explain their problems scored lower after MTS implementation. This finding may indicate that the structured, algorithm-driven nature of a formal triage assessment, while efficient, might be perceived by patients as more hurried or less personal compared to a less formalized interaction. Triage nurses, focused on systematically working through flowcharts and specific discriminators, may have less time or inclination for broader conversation or detailed explanations, potentially leading to this perception.
Interestingly, the study also noted a non-significant trend suggesting that patients triaged to lower urgency levels (e.g., Green) reported higher satisfaction rates on all questions compared to those in higher, but not life-threatening, urgency levels (e.g., Yellow). This could imply that if the triage process effectively communicates a patient's lower acuity status and manages their expectations regarding anticipated waiting times, even a longer wait can be perceived as more acceptable and result in greater satisfaction. This highlights the crucial role of clear communication by the triage nurse regarding the assigned priority level and the rationale for the expected wait as a key component in shaping the patient's overall experience and satisfaction with their ED visit.
6. MTS in Context: Comparisons with Other Triage Systems
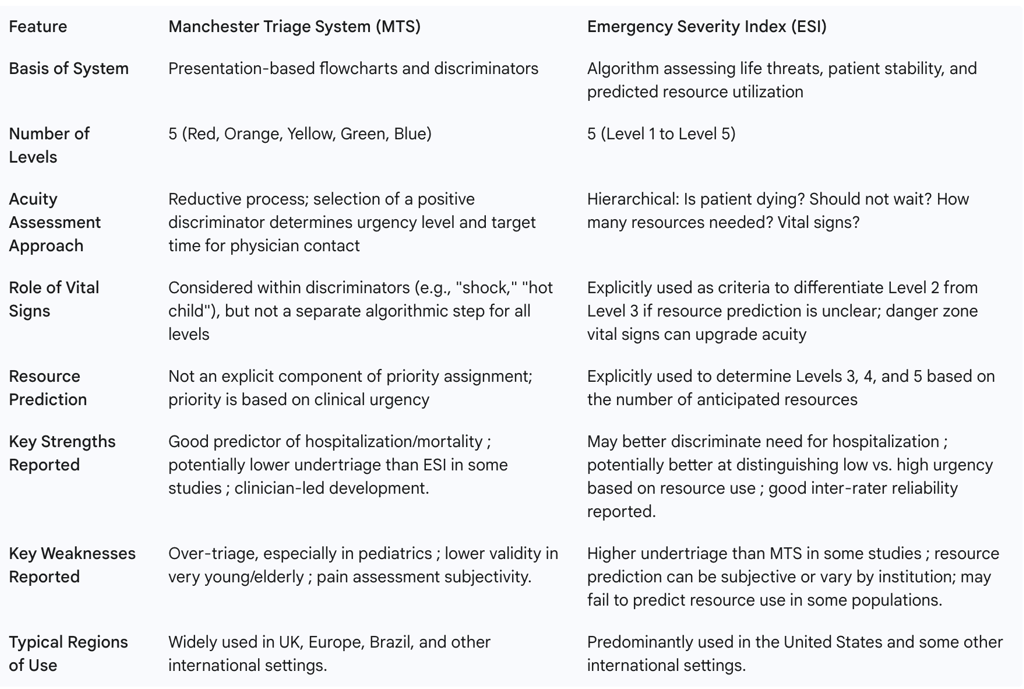
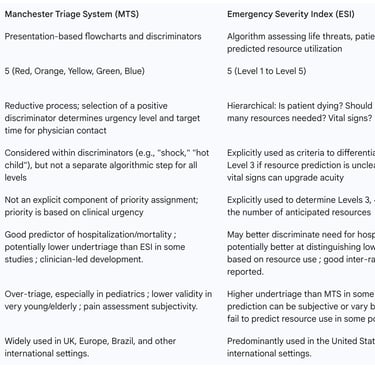
The Manchester Triage System is one of several internationally recognized five-level triage systems. Understanding its characteristics in relation to other prominent systems, such as the Emergency Severity Index (ESI) and the Canadian Triage and Acuity Scale (CTAS), provides valuable context for assessing its strengths and limitations.
MTS vs. Emergency Severity Index (ESI)
The ESI, widely used in North America, shares the five-level structure with MTS but employs a different underlying logic for categorization, particularly for mid-to-low acuity patients.
Methodology: MTS relies on approximately 52 presentation-based flowcharts and specific discriminators to assign an urgency level tied to a maximum waiting time for physician assessment. In contrast, the ESI algorithm first assesses for immediate life-threatening conditions (Level 1) and then for high-risk situations where a patient should not wait (Level 2). For patients not meeting Level 1 or 2 criteria, ESI Levels 3, 4, and 5 are determined by predicting the number of different types of resources (e.g., labs, imaging, IV fluids, consultations) the patient is likely to require. The ESI also incorporates vital signs more explicitly in distinguishing between certain levels, particularly between Level 2 and Level 3.
Performance and Outcomes:
Undertriage: Some studies suggest that ESI may be associated with higher rates of undertriage compared to MTS. For example, one study found an undertriage rate of 20% with ESI versus 11% with MTS when compared against an expert panel reference standard.
Prediction of Admission/Hospitalization: Both systems generally predict the likelihood of hospital admission well, with some evidence suggesting ESI might be a slightly better predictor or may better discriminate the need for hospitalization. Conversely, a study comparing MTS with the National Early Warning Score (NEWS), which shares some conceptual underpinnings with ESI's vital sign considerations, found MTS to be superior in predicting hospitalization and ICU admission.
Resource Utilization: ESI explicitly incorporates predicted resource consumption into its algorithm for Levels 3-5. One multicenter study indicated that ESI might be more effective in distinguishing between patients with low and high urgency based on actual resource use and mortality in the lowest urgency level. However, another study found that ESI failed to predict resource consumption or ED length of stay effectively in their specific patient population.
Length of Stay (LOS): In a study focused on trauma patients, the mean ED LOS was found to be significantly lower for patients triaged with MTS compared to ESI.
Overall Comparability: Despite these specific findings, several systematic reviews and comparative analyses conclude that there is no definitive preference for either system, with their overall performance often appearing comparable. Direct head-to-head comparisons across large, diverse patient populations remain relatively scarce, making definitive global judgments difficult.
The fundamental divergence in their core methodologies—MTS being primarily driven by patient presentation and specific clinical discriminators versus ESI's incorporation of explicit resource prediction for a subset of patients—likely contributes to their differing strengths in various performance areas. ESI may offer advantages in settings where early prediction of resource allocation for non-critical patients is a primary operational goal. MTS, with its direct focus on clinical urgency based on presenting signs and symptoms, may be perceived as more aligned with the immediate task of identifying how quickly a patient needs medical assessment. The conflicting findings across studies regarding which system exhibits less undertriage or better predicts specific outcomes suggest that factors such as study design, the characteristics of the patient population being studied, and the specific operational context of the emergency department heavily influence any observed comparative performance. Consequently, there may not be a universally "better" system; the optimal choice may depend on local priorities and contextual factors.
Table 3: Comparative Analysis of MTS and ESI
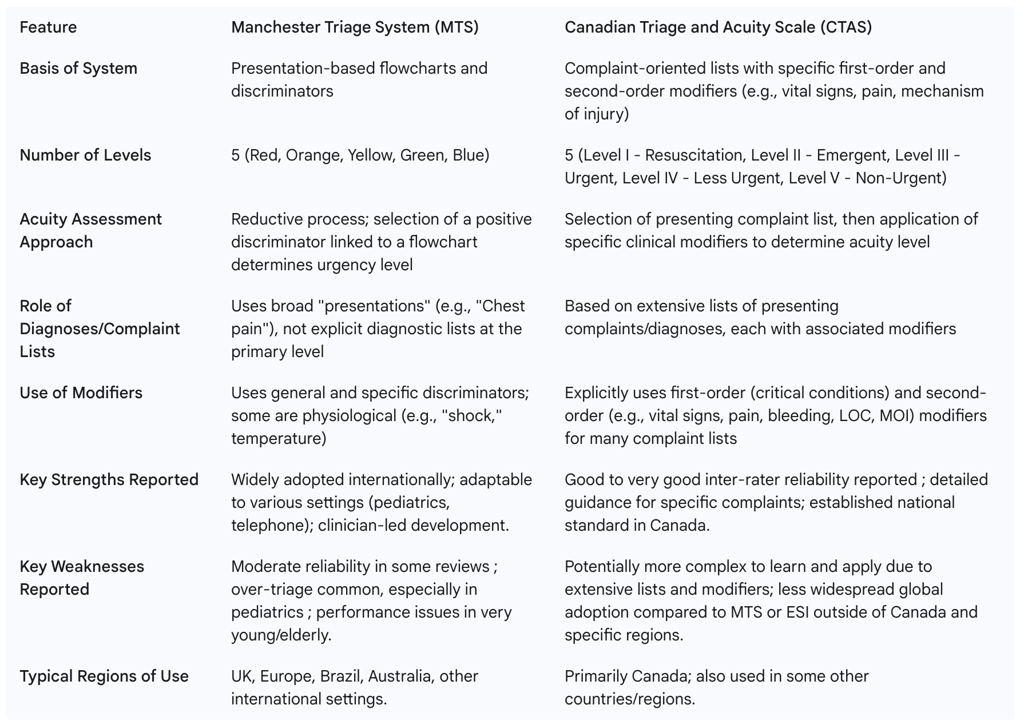
MTS vs. Canadian Triage and Acuity Scale (CTAS)
The Canadian Triage and Acuity Scale (CTAS) is another prominent five-level triage system, primarily used in Canada but also influential and adopted in some other countries, including parts of Europe.
Methodology: Like MTS, CTAS is a five-level system. However, its approach differs. CTAS is based on the Australasian Triage Scale (ATS) and incorporates lists of common presenting complaints or diagnoses. For each complaint, it provides specific first-order modifiers (critical "must-see" conditions) and second-order modifiers (e.g., vital signs, pain severity, mechanism of injury, level of consciousness, bleeding) that help the triage nurse assign the patient to one of the five acuity levels. This suggests a more granular, rule-based approach for specific presentations compared to the broader presentational flowcharts of MTS. Electronic versions, such as eCTAS, have been developed to aid in its application and potentially improve accuracy.
Performance and Outcomes:
Reliability: CTAS has generally demonstrated good to very good inter-rater reliability, with kappa statistics often reported in the range of 0.7 to 0.95. Some comparative reviews have suggested that CTAS may achieve higher reliability than MTS (where kappa values were cited as 0.3 to 0.6 in the same review). This potentially higher reliability could be attributed to CTAS's more explicitly defined criteria and physiological modifiers, which may leave less room for subjective interpretation compared to some aspects of the MTS.
Complexity: The more detailed and complaint-specific nature of CTAS, with its extensive lists of modifiers, might offer more precise guidance for a wide array of conditions. However, this increased granularity could also translate to a more complex system to learn thoroughly and apply consistently, particularly under time pressure in a busy ED.
The more structured and detailed complaint lists with specific physiological and situational modifiers in CTAS offer a contrast to the MTS's reliance on broader presentational flowcharts and a more limited set of general and specific discriminators. While CTAS's approach might enhance precision for common diagnoses and potentially contribute to its reported higher reliability, this must be balanced against considerations of ease of use, training duration, and the cognitive load placed on triage nurses.
Table 4: Comparative Analysis of MTS and CTAS
7. Criticisms, Limitations, and Areas for Development
Despite its widespread adoption and recognized strengths, the Manchester Triage System is not without criticisms and limitations. Understanding these challenges is crucial for its effective implementation and for identifying areas for future development.
Identified Weaknesses and Challenges
Several inherent and operational challenges have been associated with the MTS:
Human Error and Bias: Triage, even with a standardized tool, is performed by healthcare professionals working under considerable pressure. This environment can contribute to errors in judgment or application of the system. Furthermore, personal judgments, unconscious biases, or prejudices, though unintended, may influence the categorization process, potentially leading to inconsistencies. The interplay between these human factors and the inherent subjectivity in assessing certain common discriminators, such as pain, creates a significant vulnerability. Pain is a frequent and powerful discriminator within MTS, yet its assessment is complex and difficult to objectify entirely. Variations in a nurse's perception of a patient's pain tolerance, or a patient's ability to articulate their pain, can lead to differing triage outcomes even when standardized pain scales are employed.
Resource Constraints: The availability of staff, diagnostic services, and treatment spaces can significantly impact the effectiveness of any triage system. Even if patients are accurately and promptly triaged by MTS, limited downstream resources can lead to delays in physician assessment and treatment, negating the benefits of prioritization. Such constraints can create a detrimental feedback loop: if resources are scarce, waiting times escalate even for correctly triaged urgent patients. This can lead to patient deterioration (making the initial triage appear inaccurate in retrospect) and contribute to staff burnout, which in turn may increase the likelihood of triage errors.
Over-triage and Under-triage: As previously discussed, these misclassification issues persist. While MTS often demonstrates a tendency towards over-triage, particularly in pediatric populations , which can strain ED resources, under-triage remains a critical safety concern due to the risk of delayed care for seriously ill patients. Some studies have indicated that the system's safety margin can be low due to instances of significant undertriage and suboptimal sensitivity in identifying patients requiring the highest levels of urgency.
Performance in Specific Patient Populations: The validity and reliability of MTS have been shown to be lower in certain vulnerable patient groups, notably very young children and elderly individuals. These populations often present with atypical symptoms, communication difficulties, and altered physiological responses, making standardized assessment more challenging. In some contexts, MTS has been found to be an inadequate predictor of severity or mortality specifically in older adults.
Pace of Updates and Systemic Inertia: A broader criticism leveled at many widely used triage systems, potentially including MTS despite its structured update process, is that they may undergo minimal substantial updates even as new scientific evidence emerges. While the MTS has an International Reference Group responsible for evidence-based revisions , there can be a lag between the publication of relevant research findings (e.g., on optimal pediatric discriminators or improved assessment techniques for the elderly) and their formal incorporation into official MTS editions. Further delays can occur in the translation of these updates into local hospital IT systems and clinical practice. This potential gap between best available evidence and current operational versions of the tool can mean that known deficiencies are not addressed as promptly as might be ideal.
Implementation Complexity: The successful integration of MTS into the complex operational environment of an emergency department is not a simple task. Merely transferring the presentational flowcharts and discriminators into a Hospital Information System is insufficient; numerous interdependencies with other ED processes, staffing models, and communication pathways must be considered and managed.
The Importance of Training and Auditing
The developers of the Manchester Triage System recognized from its inception that the tool's effectiveness is intrinsically linked to the skill of its users and the quality of its implementation. This understanding is reflected in the ongoing emphasis on rigorous training and systematic auditing.
The official Manchester Triage Group (MTG) explicitly states that the MTS was developed for use exclusively by registered Health Care Professionals (HCPs). This stipulation is due to the advanced clinical skills, knowledge base, and critical judgment required to accurately assess patient needs, interpret discriminators within the clinical context, and plan appropriate care based on the triage decision. The MTG further underscores this by stating it will not support organizations that permit non-HCP staff to use the MTS, and would attest to this in any medical negligence proceedings. This firm stance highlights that MTS is not a simple checklist to be mechanically followed but a sophisticated clinical decision support tool that necessitates professional interpretation and accountability.
Complementary to robust initial training, a structured process for ongoing quality improvement through regular audits is deemed essential. The MTS guidelines define specific parameters for these audits, including recommended sample sizes (e.g., a minimum of 10 episodes per user or 2% of cases), defined test criteria for accuracy, performance targets, and a minimum audit frequency of at least once per quarter. Continuous improvement initiatives and the provision of adequate, recurrent training are consistently highlighted as vital for maintaining high standards of emergency care triage. The requirement for ongoing audit and training implicitly acknowledges that triage skills, like many complex clinical competencies, can degrade or "drift" from standardized protocols over time if not actively monitored, reinforced, and refined. Factors such as staff turnover, changes in patient demographics or case mix, or even subtle shifts in the interpretation of guidelines can impact performance. Regular audits serve to identify such deviations and trigger corrective actions, which may include targeted retraining, clarification of guidelines, or system adjustments, thereby forming a continuous quality improvement cycle.
Future Directions: Enhancements and the Role of Technology (e.g., AI)
The field of emergency triage is continually evolving, with ongoing efforts to refine existing systems like the MTS and explore innovative approaches to enhance accuracy, efficiency, and patient safety. The rapid development and increasing sophistication of Artificial Intelligence (AI) and machine learning technologies are viewed with considerable interest as potential avenues for improving risk estimation and triage assessment in emergency care.
AI-driven solutions could potentially offer real-time analysis of complex patient data, including vital signs, demographic information, past medical history, and even non-verbal cues (such as restlessness or breathing patterns, as suggested by one source in relation to video analysis tools ), to generate rapid and highly accurate triage decisions. The aspiration is that such systems might surpass human capabilities in terms of consistency, speed, and the ability to identify subtle patterns indicative of high clinical risk, particularly in mitigating the impact of human error or cognitive biases under pressure. The integration of AI into triage is seen not merely as a way to digitize current processes but as a means to create more sophisticated algorithms capable of processing a richer dataset than is typically feasible for a human triage nurse in a time-constrained environment.
Teletriage, leveraging telehealth technologies to conduct remote triage assessments before a patient physically arrives at the ED, or to direct them to alternative care pathways, is another emerging area of development. This has the potential to manage patient flow more effectively and provide earlier advice or intervention.
However, the overarching challenge for the future of triage systems, whether an enhanced MTS or a novel AI-based platform, extends beyond simply achieving more accurate prioritization. A key objective is to develop systems that can effectively "stream" patients—that is, to not only determine urgency but also to direct individuals to the most appropriate specific care pathway or resource from the outset. This might involve identifying the need for immediate access to a stroke unit, a cardiac catheterization lab, a trauma center, or even referral to general practice for less acute conditions. Such advanced streaming capabilities move beyond the current primary scope of MTS (which focuses on time to first physician contact ) towards more complex, early disposition planning. While this offers the promise of significant improvements in ED efficiency and patient outcomes, it also increases the complexity of the decision-making process and raises the stakes if streaming decisions are incorrect. The ultimate goal is to create an integrated system that accurately identifies patient need, distinguishes it from simple demand, and efficiently navigates the patient to the optimal point of care.
8. Navigating Official Resources and Guidelines
The Manchester Triage Group and Triagenet.net
For authoritative information, updates, and resources related to the Manchester Triage System, Triagenet.net serves as the official online portal. This website is maintained under the auspices of the Manchester Triage Group (MTG), the body that continues to oversee the development and dissemination of the system.
Triagenet.net provides comprehensive details on the suite of five distinct MTS tools currently available:
Emergency Triage: The foundational tool for use in Emergency Departments and by Ambulance Services during face-to-face patient contact.
Telephone Triage and Advice: Adapted for urgent and emergency care telephone assessment services.
Pre-Hospital Pathfinder: Designed for Ambulance Services in the pre-hospital setting.
Nursing and Residential Triage (NaRT): Tailored for staff in nursing and residential care homes.
Community Triage Tool: For use by community assessment teams, first responders, and pendant alarm providers.
The website consistently emphasizes two critical aspects of MTS implementation: the necessity for healthcare organizations to ensure their MTS versions are up-to-date and officially supported, and the strict guideline that MTS is intended for use only by registered Health Care Professionals (HCPs) due to the requisite clinical acumen. Beyond these core messages, Triagenet.net offers a wealth of information including news and updates on system editions and research, details regarding licensing for use of the tools, lists of software companies with official MTS licenses, and links to global learning resources and training opportunities.
The existence of a recognized, official governing body (the MTG) and a centralized, authoritative information resource (Triagenet.net) is of paramount importance for maintaining the integrity, standardization, and controlled, evidence-based evolution of a clinical system as globally utilized as the MTS. This structure provides a single, reliable source of truth for all official guidelines, updates, and support materials. It helps to prevent fragmentation of the system, ensures that modifications are disseminated accurately and consistently to all users, provides clear directives on appropriate use (such as the restriction to HCPs), and manages the licensing process for software implementations. This centralized oversight is instrumental in preserving the quality, consistency, and recognized standards associated with the Manchester Triage System brand and its underlying methodology.
NICE Guidance and its Relevance
The National Institute for Health and Care Excellence (NICE) in the United Kingdom is a highly influential body that provides national guidance and advice to improve health and social care. NICE develops evidence-based recommendations, quality standards, and performance indicators across a wide range of health topics, including emergency and acute medical care.
While the provided research materials do not detail specific NICE guidelines that explicitly endorse or mandate the Manchester Triage System by name over other triage systems, NICE's broader role in shaping clinical practice within the UK's National Health Service (NHS) is highly relevant to how MTS is implemented, utilized, and audited, particularly in its country of origin. NICE's quality standards for emergency care would undoubtedly emphasize principles such as the rapid and accurate assessment of critically ill patients, timely initiation of appropriate interventions, efficient patient flow, and robust patient safety processes.
A validated and properly implemented triage system like the MTS, which is designed to achieve these very objectives through a standardized approach to risk stratification, would inherently align with the overarching goals of NICE guidance for emergency services. Therefore, while NICE may not issue a specific "guideline on the Manchester Triage System," its recommendations concerning the quality of emergency and urgent care would create a clinical and policy environment where the use of a robust, evidence-supported triage system is implicitly supported, if not expected. Given the UK origins of MTS, its extensive evidence base, and its widespread adoption within the NHS, it would naturally be a strong candidate for fulfilling such quality requirements. Indeed, one study on MTS validity mentioned that modifications to the MTS protocol in a UK hospital were based on previous research outcomes, a practice that resonates with NICE's strong emphasis on evidence-based practice.
9. Concluding Perspectives on the Manchester Triage System
Summary of Strengths and Enduring Value
The Manchester Triage System has established itself as a significant and enduring methodology in the realm of emergency patient prioritization. Its primary strength lies in providing a standardized, systematic, and widely adopted framework for clinical risk management within the demanding environment of emergency care. The system's design, which is presentation-based rather than diagnosis-based, allows for rapid assessment by registered healthcare professionals without requiring a definitive diagnosis at the point of triage. Its structured approach, utilizing clear flowcharts and defined discriminators, coupled with a distinct five-level priority system, promotes consistency in urgency assessment.
A key element of its enduring value is its adaptability. The MTS has proven versatile, with versions tailored for various settings beyond the traditional ED, including pediatric emergency care, telephone triage, nursing homes, and community services. It is also designed for effective integration into hospital IT systems, which is crucial for modern healthcare delivery. Clinically, the MTS has demonstrated good predictive value for serious patient outcomes, including the need for hospitalization and the risk of mortality, thereby identifying patients who require more intensive care. In many contexts, it has shown moderate to good levels of validity and reliability. The clinician-led nature of its original development, combined with an established international structure for ongoing, evidence-based updates and review, further underpins its credibility and continued relevance.
Key Considerations for Effective Implementation and Continuous Improvement
The successful implementation and sustained effectiveness of the Manchester Triage System extend far beyond the mere adoption of its flowcharts and discriminators. It requires a comprehensive, multifaceted approach. Critical success factors include:
Rigorous and Ongoing Training: MTS must be used by registered healthcare professionals who have received thorough initial training and participate in regular refresher courses to maintain competency and adapt to any system updates.
Systematic Auditing and Feedback: Regular audits of triage decisions, with defined methodologies and targets, are essential for monitoring performance, identifying areas for improvement, and providing constructive feedback to staff.
High-Fidelity IT Integration: If computerized, the MTS must be accurately mapped into the IT system, with strict adherence to the approved flowcharts, discriminator definitions, and their prescribed order, to maintain the integrity of the triage logic.
Awareness and Mitigation of Limitations: Healthcare organizations must be cognizant of the known limitations of MTS, such as its potentially reduced performance in very young or elderly patients, and the persistent challenges of over-triage and under-triage. Strategies to mitigate these issues, such as specialized training or adjunct assessment tools for vulnerable populations, should be considered.
Integration with Broader Process Redesign: MTS implementation should not occur in a vacuum. Its benefits are maximized when it is integrated into broader emergency department process redesign efforts aimed at optimizing patient flow from arrival through to disposition.
Protocols for Reassessment: Given the dynamic nature of patient conditions, clear protocols for the reassessment of waiting patients, especially those whose target times for physician contact are approaching or have been breached, are crucial for safety.
Continuous Evaluation and Adaptation: Local data on MTS performance should be continuously monitored, and the system (including local protocols and training) should be adapted based on these findings and emerging research to ensure ongoing effectiveness and patient safety.
The Manchester Triage System represents a significant advancement in the effort to standardize and improve the prioritization of patients in emergency settings. It has provided a common language of urgency and a robust framework for risk assessment that has been adopted globally. However, it is not a static or infallible solution. Its ultimate effectiveness and its contribution to patient safety are critically dependent on a synergistic relationship between the tool itself, the skilled and well-trained clinicians who apply it, the rigor of local implementation and quality assurance processes, and, importantly, the capacity of the broader emergency care system to respond effectively to the priorities that the MTS identifies. The journey of the MTS from a local initiative designed to address inconsistency to an international standard reflects an ongoing endeavor to balance the benefits of standardization with the complexities of clinical nuance, and to adapt to the ever-evolving challenges of delivering safe and timely emergency care.
Conclusion
The Manchester Triage System represents a remarkable achievement in emergency medicine – a standardized approach to patient prioritization that transcends language barriers, healthcare system differences, and geographical boundaries. From its origins in 1990s Manchester to its current status as a global standard, the MTS has continuously evolved while maintaining its core principles of patient-centered, evidence-based care.
The system's strengths lie in its simplicity of application combined with clinical rigor, its focus on presenting problems rather than diagnoses, and its adaptability to various healthcare contexts. While challenges remain in certain patient populations and presentation types, ongoing research and development continue to refine and enhance the system's effectiveness.
As emergency departments worldwide face increasing demand pressures and resource constraints, the value of effective triage systems becomes ever more apparent. The Manchester Triage System provides not only a practical tool for daily clinical use but also a common language for emergency care professionals globally, facilitating collaboration, research, and continuous improvement in this critical area of healthcare delivery.
The future of the MTS lies in its integration with emerging technologies, including artificial intelligence and machine learning, while preserving the essential human judgment that remains at the heart of compassionate emergency care. By balancing technological innovation with clinical expertise, the Manchester Triage System is well-positioned to continue serving as a cornerstone of effective emergency department operations for decades to come.
Frequently Asked Questions (FAQ)
1. What is the Manchester Triage System?
The Manchester Triage System is a standardized method used in emergency departments to assess patients and determine the order in which they should receive medical attention based on clinical urgency rather than arrival time.
2. How does the Manchester Triage System categorize patients?
The MTS categorizes patients into five priority levels: Immediate (Red), Very Urgent (Orange), Urgent (Yellow), Standard (Green), and Non-Urgent (Blue), each with a corresponding maximum waiting time for medical assessment.
3. Who performs triage using the Manchester Triage System?
Triage is typically performed by specially trained nurses, though in some settings, other healthcare professionals such as paramedics or physicians may also conduct triage assessments.
4. How long does a Manchester Triage System assessment take?
A standard MTS assessment typically takes between 2-3 minutes to complete, though complex cases may require additional time.
5. Is the Manchester Triage System used worldwide?
Yes, the MTS has been implemented in over 30 countries across Europe, South America, Asia, Africa, and Australia, making it one of the most widely adopted triage systems globally.
6. How accurate is the Manchester Triage System?
Research shows the MTS has good sensitivity (87-95%) for identifying critically ill patients, though specificity is lower (65-75%) as the system intentionally prioritizes not missing serious conditions.
7. How does the Manchester Triage System handle pediatric patients?
The MTS includes specific flowcharts for pediatric presentations and modified discriminators that account for children's different physiological parameters and presentation patterns.
8. Can the Manchester Triage System be used in disaster situations?
Yes, the MTS can be adapted for mass casualty incidents, though some modifications may be necessary to account for the specific challenges of disaster response.
9. How is the Manchester Triage System updated over time?
The International Reference Group for the MTS meets regularly to review evidence and user feedback, publishing updated editions that incorporate new research and clinical knowledge.
10. How does pain assessment factor into the Manchester Triage System?
Pain is a key discriminator in the MTS, with severe pain potentially triggering a "Very Urgent" classification regardless of other factors, recognizing that pain management is an essential component of emergency care.
Additional Resources
The Manchester Triage Group - Official Guidelines and Updates
Emergency Triage: Manchester Triage Group, 3rd Edition - The definitive reference guide for MTS implementation and practice.
International Journal of Emergency Medicine - Regular publications on triage systems effectiveness and implementation.
World Health Organization Emergency Care Guidelines - Framework for emergency care system development incorporating triage principles.
Emergency Nurses Association Triage Resources - Educational materials and practice standards for emergency triage.
