Triage Systems Compared: A Comprehensive Analysis of MTS, ESI, CTAS, ATS, and SATS
Explore the strengths, weaknesses, and practical applications of the five major emergency triage systems in 2025. Learn which methodology best suits different healthcare settings and patient populations.


Emergency Departments (EDs) worldwide operate at the critical interface of healthcare, characterized by an unpredictable influx of patients presenting with a wide spectrum of illnesses and injuries. A fundamental challenge in this environment is the effective management of this demand against a backdrop of finite resources, including personnel, physical space, and diagnostic capabilities. Triage, derived from the French verb "trier" meaning to sort, is the cornerstone process established to address this challenge. It involves a rapid initial assessment of patients upon arrival to determine the urgency of their condition and, consequently, the priority with which they should receive medical attention. The primary objective of triage is to ensure that the most critically ill or injured individuals are identified and treated promptly, thereby optimizing patient outcomes and making the most efficient use of available healthcare resources.
The consequences of ineffective or delayed triage can be severe, contributing to ED overcrowding, prolonged patient length of stay, delays in the administration of essential care, and an increased risk of adverse patient events. Standardized triage systems have been developed and implemented globally to mitigate these risks by providing a structured, systematic, and ideally objective framework for prioritization.
Overview of the Five Triage Systems (MTS, ESI, CTAS, ATS, SATS)
This report provides a comprehensive analysis of five prominent emergency triage systems: the Manchester Triage System (MTS), the Emergency Severity Index (ESI), the Canadian Triage and Acuity Scale (CTAS), the Australasian Triage Scale (ATS), and the South African Triage Scale (SATS). Each of these systems represents a widely recognized and utilized tool for standardizing the complex process of patient prioritization in the emergency setting. While most of these systems employ a five-level acuity scale, they exhibit variations in their underlying methodologies, decision-making frameworks, and the specific clinical discriminators they employ.
Despite these differences, all share the common, overarching goal: to ensure that patients presenting to the ED are treated in an order dictated by their clinical urgency rather than merely their time of arrival. The existence of multiple, distinct, yet widely adopted triage systems across different international healthcare landscapes underscores a universal acknowledgment of the need for standardized emergency patient prioritization. However, the very diversity in their core operational methodologies—ranging from symptom-based flowcharts in MTS, resource prediction in ESI, the use of clinical modifiers in CTAS, a focus on physiological predictors in ATS, to the Triage Early Warning Score in SATS—suggests that no single approach is universally deemed optimal. This diversity implies that the choice and successful implementation of a triage system may be contingent upon specific local healthcare contexts, prevailing resource levels, and the characteristic patient populations served by a given emergency facility. The development of each system within a particular geographical and healthcare milieu (e.g., MTS in the UK, ESI in the US, CTAS in Canada, ATS in Australia/New Zealand, and SATS in South Africa) has inevitably shaped its focus and operational characteristics. These differences reflect varying healthcare philosophies, resource availability, or predominant patient presentations in their regions of origin, leading to distinct solutions for the common problem of emergency prioritization.
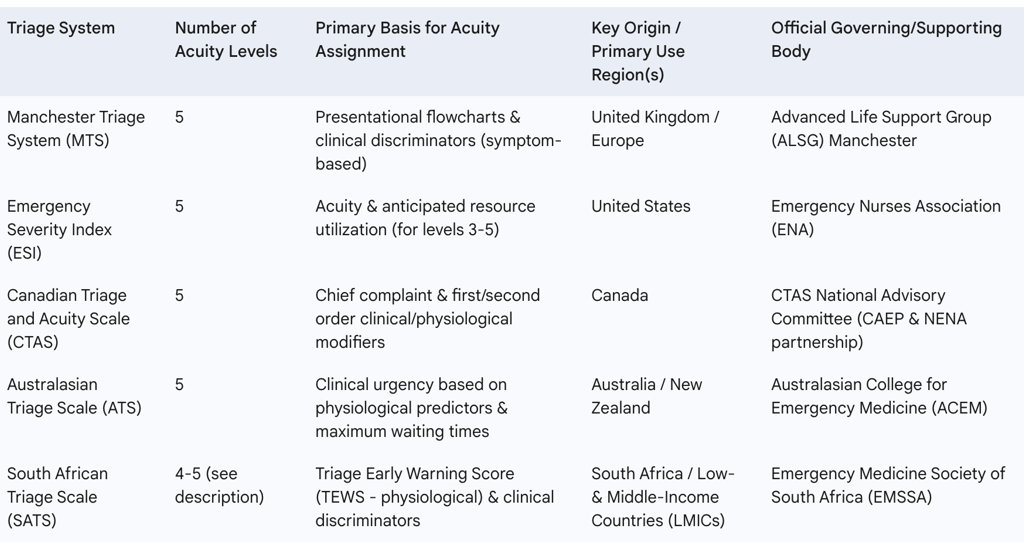
The following table (Table 1) provides a high-level comparative snapshot of the fundamental architecture and oversight of each system, serving as an orientation before a more detailed examination.
Table 1: Core Characteristics of Reviewed Triage Systems

In-Depth Analysis of Triage Systems
A. Manchester Triage System (MTS)
1. Core Methodology: Presentational Flowcharts and Discriminators
The Manchester Triage System (MTS) employs a distinctive methodology centered on the use of presentational flowcharts and clinical discriminators to determine patient priority. Upon a patient's arrival, the triage nurse selects one of approximately 52 to 53 standardized presentational flowcharts that best corresponds to the patient's chief complaint or presenting problem. These flowcharts cover a broad spectrum of presentations, categorized broadly into illness, injury, pediatric-specific issues, abnormal or unusual behavior, and major incidents. Examples include "Abdominal pain in adults," "Chest pain," "Unwell adult," "Head injury," and "Behaving strangely".
Once the appropriate flowchart is selected, the nurse systematically works through a series of "discriminators." These are structured questions focusing on specific signs, symptoms, and relevant history, designed to identify the urgency of the patient's condition. The discriminators are arranged hierarchically within each flowchart, starting with those indicative of the highest urgency. The first positive discriminator encountered determines the patient's triage category. This process is designed as a systematized protocol aiming for a rapid and dynamic assessment of the patient's needs. A notable feature of the MTS, distinguishing it from systems like the ESI, is that its primary algorithm does not incorporate the prediction of resource utilization in determining the triage level.
The highly structured, protocolized approach inherent in MTS, with its extensive array of 52-53 detailed flowcharts, offers a potential advantage in standardizing training and could facilitate ease of use, particularly for nursing staff with less emergency department experience. This detailed framework aims to guide the clinician through a logical sequence of assessments for a wide variety of common presentations. However, this very structured nature might also present limitations when clinicians are faced with atypical patient presentations, complex cases involving multiple co-existing medical conditions (which are increasingly common, especially in geriatric populations ), or rapidly evolving clinical scenarios that do not neatly align with a predefined flowchart. The frequent utilization of the "unwell adult" flowchart , and its documented lower predictive accuracy for serious outcomes in certain patient groups such as older adults , could be indicative of this tension. In instances where a patient's condition is non-specific or multifaceted, the system might default to a more general, and potentially less precise, pathway, potentially impacting the accuracy of prioritization.
2. Acuity Levels and Time-to-Treatment Targets
MTS categorizes patients into five color-coded priority levels, each associated with a maximum target time within which medical assessment and treatment should commence :
Red (Immediate): Represents life-threatening conditions requiring immediate intervention. All other activities are interrupted to initiate treatment without delay.
Orange (Very Urgent): Indicates high-risk conditions requiring treatment within 10 minutes of presentation.
Yellow (Urgent): For serious conditions that are not immediately life-threatening but may become so. Target times vary slightly by source, with some indicating treatment within 30 minutes and others within 60 minutes.
Green (Standard/Normal): Applies to non-life-threatening cases that still require timely treatment. Target times are cited as within 90 minutes or 2 hours.
Blue (Non-Urgent/Not urgent): The lowest urgency level, for conditions where patients can safely wait. Target times are reported as within 120 minutes or up to 4 hours.
It is important to note that specific implementations can vary. For instance, Charité's emergency departments in Germany utilize an "Extended MTS." This adaptation supplements the standard patient-described symptoms with an assessment of vital functions, including respiration, circulation, and consciousness. This involves measuring vital parameters such as pulse, blood pressure, respiratory rate, oxygen saturation, level of consciousness, and sometimes body temperature. Additionally, specific inquiries are made about symptoms potentially related to heart attack or stroke to facilitate early recognition and intervention. This local adaptation suggests a recognized need to enhance the standard MTS with more objective physiological data in certain settings.
The existence of such local adaptations, like the "Extended MTS" at Charité and the various pediatric modifications developed for the system , serves as a practical demonstration that the foundational MTS framework can be augmented and refined. These enhancements often aim to address specific patient populations more effectively or to improve the capture of critical clinical data. This adaptability indicates that while MTS provides a standardized core, its optimal performance and safety profile may be best achieved when healthcare institutions proactively identify its limitations within their unique operational context and patient demographics, and then strategically implement validated modifications. However, such adaptations also introduce the potential for variability in MTS application across different sites if not carefully managed, standardized where appropriate, and rigorously validated.
3. Development, Global Adoption, and Official Resources
The MTS was originally developed in Manchester, England, during the 1990s. Since its inception, it has gained widespread adoption, particularly across Europe. Countries where MTS is extensively used include Germany , Portugal, and The Netherlands. Numerous hospitals internationally have implemented the system, as evidenced by lists of participating centers.
The Advanced Life Support Group (ALSG) based in Manchester is the official body overseeing the MTS (manchestertriage@alsg.org). Triagenet.net serves as a central online hub providing access to MTS resources, training courses, information on international conferences, and details of software companies that hold valid licenses for MTS implementation.
4. Reported Reliability, Validity, Strengths, and Limitations
Strengths: MTS is recognized for offering a structured approach to patient prioritization and is one of the most widely used triage systems globally. Studies have indicated its applicability across diverse patient populations, including adults, children, and patients with specific conditions such as coronary syndromes and acute pulmonary embolism. It has been reported as a good predictor of the need for hospital admission and of short-term mortality. Furthermore, MTS is credited with improving the organization and efficiency of nursing evaluations by providing a systematic method for reviewing medical history, taking vital signs, and performing assessments. Its straightforward design is considered easy to understand and implement.
Limitations: Despite its strengths, MTS is susceptible to human error and inherent biases in clinical judgment, which can lead to inconsistencies in classification. The effectiveness of the system, even with accurate triage, can be undermined by external factors such as resource constraints within the hospital and patient flow bottlenecks, particularly during peak times or large-scale emergencies. A consistent finding in the literature is the occurrence of both under-triage (classifying a patient at a lower urgency level than appropriate) and over-triage (classifying at a higher urgency). The "unwell adult" flowchart, though frequently used, has demonstrated lower predictive ability for outcomes like hospitalization or ICU admission, particularly in older patient populations. Some earlier analyses also noted limited general information on the system's ability to correctly stratify patients against medium-term mortality, although more recent validation studies have addressed this.
Reliability and Validity: The reliability and validity of MTS have been assessed in various studies. A Dutch study reported "substantial" inter-rater reliability with a weighted kappa of 0.62 and high test-retest reliability. An Italian multicenter simulation study found an overall Cohen's kappa of 0.59 between triage nurses and an expert panel, indicating moderate agreement. In terms of validity, the Dutch study found a sensitivity of 53.2% for urgent adult patients and a specificity of 95.1%; sensitivity was notably higher for pediatric patients at 83.3%. A systematic review concluded that while most studies showed the efficacy of MTS, errors in classification persist. More recent research has demonstrated excellent discriminatory ability for predicting short-term mortality.
5. Specific Applications
Pain Assessment: Pain is one of the six general discriminators within the MTS framework and is featured in 43 of the system's flowcharts. The guidelines stipulate that pain should be assessed regardless of the patient's primary complaint. MTS advocates for the use of a pain ruler, integrating both the patient's subjective judgment of their pain and the nurse's objective perception. This dual assessment is intended to balance patient reporting with clinical observation. However, research indicates that pain assessment at triage is often performed infrequently. This may be attributed to nurses' beliefs that formal pain scoring could lead to overtriage, insufficient education on pain assessment protocols, or a lack of clarity within the MTS guidelines themselves regarding pain assessment. In some clinical settings, nurses routinely collect pain scale data as part of the MTS process.
Pediatric Adaptations: Recognizing that the original MTS might not optimally perform for all pediatric presentations, specific age-dependent modifications have been developed and implemented. These modifications aim to improve the system's accuracy, particularly its specificity, for children. Such adaptations can include updating the prioritization criteria for children with complex syndromic diseases, those presenting with symptoms related to chronic illnesses, or children with a decreased general condition (DGC). For instance, an urgency level upgrade modification has been proposed for children with Congenital Heart Disease (CHD) to mitigate the risk of under-triage in this vulnerable group. Specific changes have involved adding discriminators like "petechiae" to the "rashes" flowchart for suspected meningococcal infection and adjusting the urgency levels associated with discriminators such as "fever" (based on age), "wheeze," and "unable to talk in sentences" for pediatric patients. MTS also includes dedicated pediatric flowcharts such as "Crying Baby," "Limping Child," and "Unwell Child".
Geriatric Adaptations: The triage of older adults presents unique challenges, as this population is more frequently triaged inappropriately, potentially leading to delays in care and adverse outcomes. Frailty is a significant complicating factor in geriatric emergency care. Research has explored the integration of frailty screening tools—such as PRISMA-7 (Program of Research to Integrate Services for the Maintenance of Autonomy), ISAR (Identification of Seniors at Risk), and FRESH (Fatigue, Recent falls, Episodes of weakness, S_Sneed for assistance with daily activities)—into the MTS process. The aim is to prevent the misclassification of elderly patients who often present with atypical or non-specific complaints. The commonly used "unwell adult" flowchart has shown limitations in its predictive accuracy for serious conditions in this age group.
Mental Health Considerations: MTS addresses mental health presentations through specific flowcharts such as "Behaving strangely" and "Mental illness". It is important to distinguish the general MTS used in EDs from specialized tools like the UK Mental Health Triage Scale (MHTS). The UK MHTS, adapted from an Australian counterpart, is designed for use in specialist mental health services and often involves telephone-based screening to determine urgency and appropriate service response; these services may be co-located with general hospital EDs. The standard MTS remains a general ED triage tool applicable to all presenting patients, including those with primary mental health concerns.
B. Emergency Severity Index (ESI)
1. Core Methodology: Acuity and Resource Prediction Algorithm
The Emergency Severity Index (ESI) is a five-level triage algorithm widely used in emergency departments, particularly in the United States. Its core methodology is distinctive in that it assesses patients based on both the acuity of their medical condition and, for less acute patients, the number of resources their care is anticipated to require during their ED visit. This resource prediction component is a key differentiator from systems like MTS.
The ESI algorithm guides the triage nurse through a maximum of four decision points, labeled A, B, C, and D, which must be addressed sequentially :
Decision Point A: Is the patient unstable and in need of immediate life-saving intervention? If yes, the patient is assigned ESI Level 1. This assessment looks for conditions like unresponsiveness, active seizures, airway obstruction, or ineffective gas exchange/perfusion.
Decision Point B: Is this a high-risk situation? Is the patient likely to deteriorate, or are there signs of a time-critical problem? If yes (and not ESI 1), the patient is assigned ESI Level 2. This considers if the patient is confused/lethargic/disoriented, in severe pain or distress (physiological or psychological), or if the situation is deemed high-risk based on presentation (e.g., active chest pain suspicious for ACS, signs of stroke, immunocompromised patient with fever).
Decision Point C: How many different types of resources will this patient need? This point is addressed only if the patient is stable and does not meet ESI 1 or 2 criteria. "Resources" are defined as specific interventions or diagnostic tools beyond a basic physical examination. Examples include laboratory tests (blood, urine), ECG, radiological imaging (X-rays, CT, ultrasound), IV fluids, IV/IM/nebulized medications, specialty consultation, and simple procedures like laceration repair or Foley catheter insertion. Items not considered resources include history and physical exam, point-of-care testing, saline locks, PO medications, tetanus immunization, prescription refills, phone calls to PCP, crutches, splints, or slings.
If many resources (two or more) are anticipated, the patient is ESI Level 3.
If one resource is anticipated, the patient is ESI Level 4.
If no resources are anticipated, the patient is ESI Level 5.
Decision Point D: Do the patient's vital signs warrant a reassessment of the acuity level? After considering resources for stable patients, vital signs (heart rate, respiratory rate, oxygen saturation, and for pediatric patients, temperature) are reviewed against age-specific danger zone limits. If vital signs exceed these limits, the triage nurse must consider up-triaging the patient to ESI Level 2.
The ESI's unique incorporation of anticipated resource utilization for determining triage levels 3, 4, and 5 is a significant strength for emergency department flow management and operational planning, as it attempts to align patient prioritization with the department's capacity to deliver care. This predictive element can facilitate more efficient patient streaming and resource allocation. However, this approach also carries a potential risk. Patients with potentially serious underlying conditions that present subtly, or whose need for multiple resources is not immediately apparent at triage—especially if their initial vital signs are stable—might be assigned a lower acuity level (ESI 3, 4, or 5). This could inadvertently delay definitive care. This is particularly relevant given the findings that ESI's guidance can sometimes lead to an under-appreciation of severity in cases of advanced age, certain vital sign derangements, or specific chief complaints. A careful balance, therefore, must be struck by experienced triage clinicians to ensure that the focus on resource prediction does not overshadow a thorough acuity assessment, especially in complex or atypical presentations.
2. Acuity Levels and Decision Points
The ESI stratifies patients into five acuity levels :
ESI Level 1 (Immediate): Patient requires immediate life-saving intervention. Examples include cardiac arrest, unresponsive patient, profound hypotension, or hypoglycemia. This level is determined at Decision Point A.
ESI Level 2 (Emergency/High Risk): Patient is in a high-risk situation, is likely to deteriorate, or has signs of a time-critical problem that necessitates urgent evaluation. This includes patients who are confused, lethargic, disoriented, or in severe pain/distress. Examples: cardiac-related chest pain, asthma attack, altered mental status, suicidal/homicidal ideation. Determined at Decision Point B.
ESI Level 3 (Urgent): Patient is physiologically stable but requires multiple (two or more) resources to reach a disposition decision (e.g., admission, discharge). Examples: abdominal pain requiring labs and imaging, high fever with cough. Determined at Decision Point C.
ESI Level 4 (Nonurgent/Less Urgent): Patient is stable and requires only one resource. Examples: simple laceration needing sutures, rabies vaccination, sore throat needing a strep test. Determined at Decision Point C.
ESI Level 5 (Minor/No Resources): Patient is stable and requires no resources beyond examination. Examples: suture removal, prescription refill, minor rash. Determined at Decision Point C. Vital signs are then checked at Decision Point D, which can lead to an upgrade in acuity, typically to ESI 2, if danger zone criteria are met.
3. Development, Predominant Usage (USA), and Official Resources
The ESI was developed in 1998 by two emergency physicians, Dr. Richard Wuerz and Dr. David Eitel. It has become the predominant triage system in the United States, with an estimated 94% of U.S. EDs utilizing it as of 2019. While its primary base is in the U.S., the ESI is also being adopted by an increasing number of emergency departments globally.
Initially, the Agency for Healthcare Research and Quality (AHRQ) supported and maintained the ESI. Currently, the Emergency Nurses Association (ENA) is responsible for its maintenance and provides official training resources, including online courses and implementation support. The Emergency Severity Index (ESI): A Triage Tool for Emergency Department Care, Version 4 (published by AHRQ) and the updated ESI Triage Handbook, Version 5 (referenced in ENA materials ), are key guiding documents for implementation and training.
4. Reported Reliability, Validity, Strengths, and Limitations
Strengths: The ESI has been extensively studied and is generally found to be a reliable, consistent, and accurate triage tool across multiple languages, age groups, and countries. Its ease of use and the direct linkage of triage levels to anticipated ED resource utilization are considered significant advantages for ED operations and patient flow management. The ESI is endorsed by prominent professional organizations such as the American College of Emergency Physicians (ACEP) and the ENA.
Limitations: A significant operational challenge with ESI is that a large proportion of patients in U.S. EDs—often more than half—are triaged to ESI Level 3. This creates a very large, undifferentiated group of patients, which can complicate efficient resource distribution and effective patient queuing, potentially undermining one of the core purposes of triage by not providing sufficient granularity within this large mid-acuity cohort. Both under-triage and over-triage have been documented with ESI use. Studies have shown that under-triage, in particular, is associated with a higher rate of subsequent hospital admission and critical outcomes. Factors such as advanced age, specific vital sign derangements, and certain chief complaints, for which the ESI algorithm offers limited specific guidance, have been identified as areas where patient severity may be under-appreciated. The ESI is not recommended for use in mass casualty incidents or multi-casualty trauma events; alternative rapid triage systems like START (Simple Triage and Rapid Treatment) or JumpSTART for pediatric patients are preferred in such scenarios. Effective use of the ESI requires that triage nurses have at least one year of ED experience and have completed a comprehensive ESI triage training program. Insufficient education on the system can diminish the precision of triage assessments.
Reliability and Validity: A meta-analysis of ESI reliability demonstrated substantial agreement, with a pooled kappa coefficient of 0.791, indicating acceptable overall reliability both within and outside the USA. This analysis also found that agreement was higher when using the latest adult versions of the scale and among expert raters. However, a tendency to allocate patients to ESI Level 2 was also noted. Individual studies included in reviews have reported kappa statistics ranging from 0.46 (moderate) to 0.98 (almost perfect), highlighting some variability in inter-rater agreement depending on the study context. The ESI has been validated as an effective tool for classifying patients based on acuity and resource needs and predicting downstream outcomes like hospitalization.
5. Specific Applications
Pain Assessment: Severe pain or distress is explicitly listed as a consideration for assigning a patient to ESI Level 2, provided they do not meet ESI Level 1 criteria. While the ESI algorithm does not incorporate a separate, formal pain scale in the same way as MTS, the presence of severe pain that is deemed to put the patient in a high-risk situation contributes to a higher acuity rating.
Pediatric Adaptations: The ESI requires special considerations for pediatric patients. It is recommended that the ESI algorithm be used in conjunction with the Pediatric Assessment Triangle (PAT – Appearance, Work of Breathing, Circulation to Skin) and a focused pediatric history to assign an appropriate acuity level. The ESI Triage Handbook (both version 4 and the newer version 5) includes a dedicated chapter on pediatric triage, acknowledging that children have different physiological and psychological responses to illness and injury, and often present unique communication challenges. While initial research into ESI's specific use with children was minimal , subsequent work, including targeted studies and the development of pediatric-specific guidance within the ESI framework, has aimed to improve its application in this population.
Geriatric Adaptations: Older adults are a vulnerable population in the ED, prone to atypical presentations of serious illness and at higher risk for adverse outcomes. The ESI algorithm's relatively limited specific guidance for factors like advanced age or subtle vital sign derangements in the elderly can lead to an under-appreciation of their true severity. While no specific geriatric-focused modification of the ESI algorithm itself is detailed in the provided materials, comprehensive geriatric ED care guidelines emphasize the need for broader assessments that go beyond the acute chief complaint. This holistic approach might not be fully captured by ESI's resource-focused methodology for stable patients if not supplemented by strong clinical judgment and awareness of geriatric syndromes.
Mental Health Considerations: "Altered mental status" is provided as an example of a condition that could warrant an ESI Level 2 classification. Furthermore, an "actively suicidal or homicidal patient" is considered a high-risk situation, also typically leading to an ESI Level 2 assignment. The ESI system considers a patient's overall mental status as part of the triage assessment to determine acuity and potential risk.
C. Canadian Triage and Acuity Scale (CTAS)
1. Core Methodology: Complaint-Based with First and Second Order Modifiers
The Canadian Triage and Acuity Scale (CTAS) is a five-level triage system, ranging from Level I (Resuscitation) to Level V (Non-urgent), designed to prioritize patients in Canadian emergency departments. The determination of a CTAS level is a multi-step process. It begins by establishing a relationship between the patient's presenting complaint (chief complaint) and potential underlying causes. These presenting complaints are often aligned with the Canadian Emergency Department Information System (CEDIS) standardized complaint list, which provides a common nomenclature.
A key feature of CTAS is the use of First and Second Order Modifiers to refine the acuity level initially suggested by the presenting complaint.
First Order Modifiers are applied after the presenting complaint is determined and are related to fundamental physiological status. These include assessment of Airway, Breathing, and Circulation (ABCs), Level of Consciousness (LOC) often using the Glasgow Coma Scale (GCS), vital signs (considering respiratory distress, hemodynamic stability, and temperature), pain severity score, presence of a bleeding disorder, and mechanism of injury.
Second Order Modifiers are more complaint-specific and are applied after the first-order modifiers. They are intended to supplement the initial assessment and can include factors such as heat-related illness, specific pregnancy-related concerns (including post-partum issues), and a newly introduced frailty modifier. An important rule is that second-order modifiers should not be used to downgrade a CTAS level if a higher acuity is already indicated by the presenting complaint or first-order modifiers.
The CTAS process often incorporates a "Quick Look" assessment, allowing experienced triage personnel to rapidly identify obviously critically ill patients who require immediate high-level categorization. For paramedics utilizing Prehospital CTAS, a minimum of two CTAS scores are typically assigned: an "Arrival CTAS" reflecting the patient's condition prior to paramedic intervention, and a "Departure CTAS" determined after initial interventions, which helps inform the choice of receiving facility and reflects any change in the patient's status.
The CTAS methodology, with its structured use of first and second-order modifiers, allows for a considerably nuanced clinical assessment. This system enables triage personnel to adjust a patient's acuity level based on a wide array of physiological data, anamnestic details (like mechanism of injury), and demographic factors (such as frailty or pregnancy). This capacity for detailed adjustment offers a degree of flexibility and clinical depth. However, the complexity inherent in correctly applying numerous modifiers, accurately distinguishing between first and second-order modifiers, and adhering to rules such as not inappropriately downgrading acuity , may impose a significant cognitive load on the triage nurse. This complexity necessitates substantial training and experience for consistent and accurate application. If not consistently applied, or if training is insufficient, this intricate system could potentially lead to variability in inter-rater reliability, as suggested by studies noting that revisions to CTAS (which often involve modifier updates) were sometimes associated with less reliable scoring than previous guideline versions.
2. Acuity Levels and Time-to-Physician Targets
CTAS defines five acuity levels, each with a corresponding target time for physician assessment and a performance expectation :
CTAS Level I (Resuscitation): For conditions that are immediate threats to life or limb, or carry an imminent risk of deterioration, requiring immediate aggressive interventions (e.g., cardiac arrest, major trauma, shock states). Physician assessment should be immediate, with a target of 98% of these patients being seen by a physician accordingly.
CTAS Level II (Emergent): For conditions that are a potential threat to life, limb, or function, requiring rapid medical intervention or delegated acts (e.g., head injury with altered LOC, chest pain suggestive of ischemia, internal bleeding). Physician assessment target is within 15 minutes, for 95% of patients.
CTAS Level III (Urgent): For conditions that could potentially progress to a serious problem requiring emergency intervention. These may be associated with significant discomfort or affect the patient's ability to function. Patients often have normal vital signs, but their presenting problem suggests a more serious acute process (e.g., mild to moderate asthma, moderate trauma, limb fracture with deformity). Physician assessment target is within 30 minutes, for 90% of patients.
CTAS Level IV (Less Urgent): For conditions related to patient age, distress, or potential for deterioration or complications that would benefit from intervention or reassurance within 1-2 hours (e.g., urinary symptoms, mild abdominal pain, earache, minor lacerations). Physician assessment target is within 60 minutes, for 85% of patients.
CTAS Level V (Non-Urgent): For conditions where investigations or interventions could be delayed or the patient could be referred to other areas of the hospital or healthcare system (e.g., sore throat with no respiratory compromise, conditions related to chronic problems without acute worsening, minor psychiatric complaints with no suicidal ideation). Physician assessment target is within 120 minutes, for 80% of patients.
3. Development, National Implementation (Canada), and Official Resources
CTAS was introduced in Canada in 1999, its development influenced by the National Triage Scale (NTS) from Australia. It has since become widely accepted and is the standard triage tool in Canadian emergency departments. The assignment of a CTAS level is a mandatory data element for reporting to the Canadian Institute for Health Information (CIHI) for all Canadian hospital EDs. It is also utilized by ambulance services, for example, under the Ministry of Health and Long-Term Care in Ontario.
The CTAS National Advisory Committee, a collaborative partnership between the National Emergency Nurses Affiliation (NENA) and the Canadian Association of Emergency Physicians (CAEP), is responsible for the ongoing review and updating of CTAS guidelines and educational materials. The official website for CTAS information is ctas-phctas.ca, and NENA.ca provides access to course information and teaching documents. Recognizing the unique needs of children, a pediatric version, PaedCTAS, was developed in 2001. Furthermore, CTAS has been formally adapted for prehospital use, with Ontario legislating its use by paramedics in 2009.
A distinctive aspect of CTAS is its robust framework for prehospital application and its continuous evolution in this domain. The formal inclusion of the Paramedic Chiefs of Canada into the CTAS National Working Group in 2016 signifies a strong, ongoing commitment to integrating and refining CTAS for the prehospital environment. This collaborative approach facilitates a two-way dialogue between prehospital providers and ED clinicians, fostering improved communication, more consistent patient assessment across the care continuum, and smoother patient handovers from ambulance to hospital. This level of formalized prehospital integration and dedicated developmental effort appears more prominent for CTAS compared to some other international triage systems.
4. Reported Reliability, Validity, Strengths, and Limitations
Strengths: CTAS is generally recognized as an accurate and reliable tool for the rapid assessment of both adult and pediatric patients in the emergency setting. It is credited with improving patient flow and standardizing the prioritization process in Canadian EDs. Studies have also demonstrated its applicability and effectiveness in healthcare settings outside of Canada.
Limitations: Some research has indicated that revisions to the CTAS guidelines, particularly those introduced in 2008 involving modifier updates, appeared to be less reliably applied by nurses compared to the 2004 guidelines. Additionally, achieving the stringent time targets for physician assessment associated with each CTAS level can be a significant challenge for many EDs, often due to systemic pressures like overcrowding or staffing shortages.
Reliability and Validity: CTAS has generally demonstrated good inter-rater reliability in various studies. A meta-analysis of CTAS reliability reported kappa values ranging from 0.202 (fair) to 0.84 (almost perfect), indicating variability but overall acceptable performance. The validity of CTAS has been supported by its ability to predict resource utilization and the need for life-saving interventions, including in elderly patient populations. A study conducted in a non-Canadian hospital setting found a high compliance rate with CTAS, more accurate patient categorization and resource allocation compared to their standard triage method, and moderate inter-rater reliability (kappa = 0.42).
5. Specific Applications
Pain Assessment: Pain severity is incorporated as a first-order modifier in the CTAS system. The assessment of pain, particularly in elderly patients, can be complicated by factors such as increased stoicism, communication difficulties due to cognitive or sensory impairments, and potential physiological differences in pain perception. For patients with cognitive impairment, alternative pain assessment tools like the Iowa Pain Thermometer or the Faces Pain Scale-Revised may be utilized.
Pediatric Adaptations (PaedCTAS): The Canadian Paediatric Triage and Acuity Scale (PaedCTAS) was specifically developed in 2001 to address the unique triage needs of children. It maintains the five-level structure (Level I Resuscitation to Level V Non-urgent) and is assigned by trained ED nurses based on an initial impression of illness severity, the presenting complaint, and an assessment of the child's behavior and physiological measurements. PaedCTAS is considered a valid tool for pediatric triage and serves as a useful proxy measure for injury severity. Ongoing pediatric updates to CTAS guidelines have focused on areas such as fever standards and the recognition of hypertension in children.
Geriatric Adaptations: The CTAS National Working Group has acknowledged the specific challenges associated with triaging elderly patients. In response, a frailty modifier has been developed and incorporated into CTAS. This modifier is designed to help identify frail older adults who may be at higher risk of deterioration despite less acute initial presentations, often leading to an up-triage to CTAS Level III to ensure more timely assessment. A dedicated guidance document for applying CTAS to geriatric patients highlights common issues such as atypical presentations of serious conditions (e.g., acute coronary syndrome presenting without chest pain), the impact of cognitive impairment, co-morbid medical conditions, polypharmacy, and altered physiological responses to illness (e.g., blunted fever response, altered response to catecholamines). For older adults post-injury, a systolic blood pressure (SBP) of less than 110mmHg is an important indicator.
Mental Health Considerations: CTAS is utilized for patients presenting with mental health concerns, with "Mental Health" being a recognized CEDIS presenting complaint category that includes specific conditions like "violent/homicidal behavior" which would typically be triaged to CTAS Level I. However, a study examining the use of CTAS for mental health presentations found only fair inter-rater reliability (kappa = 0.312) among triage nurses for these scenarios, with wide variation in the accuracy of urgency ratings. The study suggested that greater accuracy was achieved when triage nurses appropriately used second-order modifiers and avoided overriding the scale.
D. Australasian Triage Scale (ATS)
1. Core Methodology: Clinical Urgency and Maximum Waiting Times
The Australasian Triage Scale (ATS) is a clinical tool primarily designed to establish the maximum appropriate waiting time for medical assessment and treatment for patients presenting to emergency departments. Its core principle is the prioritization of patients based on their clinical urgency. The triage assessment, typically conducted by an appropriately trained and experienced staff member (usually a nurse), is intended to be rapid, generally taking no more than two to five minutes. This assessment is a synthesis of the patient's presenting problem, their general appearance, and pertinent physiological observations. Key physiological predictors considered include airway patency, breathing effectiveness, circulatory status, and disability (often assessed using the Glasgow Coma Scale - GCS).
A crucial aspect of the ATS is its explicit focus: it is to be used only for the description of clinical urgency. It is not designed, nor is it considered valid, for determining other important ED metrics such as patient severity (beyond immediate urgency), complexity of care required, quality of care, departmental workload, or staffing requirements.
The primary emphasis of the ATS on "clinical urgency" and "maximum waiting time" provides a clear, direct, and universally understandable framework for initial patient prioritization. The foundational strength of this approach is evidenced by its influence on the development of other major international triage systems, including MTS and CTAS. This focus ensures that time-criticality remains paramount in the triage decision. However, this strength may also be a source of limitation. The reported challenges in reliably differentiating between the lower acuity categories (ATS 4 and 5) , and the scale's explicit unsuitability for measuring broader operational factors like workload or patient complexity , suggest that while ATS excels at defining how quickly a patient must be seen, it may lack the granularity needed for detailed operational management of the large volume of less acute patients or for comprehensive ED resource planning and staffing models. Systems like ESI, with its resource prediction component, or MTS, with its detailed clinical pathways, may offer more in these latter aspects.
2. Acuity Levels and Performance Indicator Thresholds
The ATS utilizes five categories, each defining the maximum waiting time for medical assessment and treatment, and associated with a performance indicator threshold that EDs aim to meet.
ATS Category 1 (Immediate): For immediately life-threatening conditions requiring immediate simultaneous assessment and treatment. Maximum waiting time: Immediate. Performance indicator threshold: 100% of patients in this category seen within this timeframe. Clinical descriptors include cardiac arrest, respiratory arrest, or severe behavioral disorder with immediate threat of dangerous violence.
ATS Category 2 (Emergency): For imminently life-threatening conditions, situations where important time-critical treatment is needed, or for patients experiencing very severe pain. Maximum waiting time: 10 minutes. Performance indicator threshold: 80%. Examples include airway risk (e.g., severe stridor), severe respiratory distress, circulatory compromise, or chest pain of likely cardiac nature.
ATS Category 3 (Urgent): For potentially life-threatening conditions, situations requiring urgent intervention to prevent adverse outcomes, or for severe discomfort or distress requiring relief. Maximum waiting time: 30 minutes. Performance indicator threshold: 75%. Examples: severe hypertension, moderate shortness of breath, or head injury with brief loss of consciousness (now alert).
ATS Category 4 (Semi-Urgent/Potentially Serious): For conditions that are potentially serious, may deteriorate if not assessed within the hour, involve significant complexity, or cause discomfort requiring relief. Maximum waiting time: 60 minutes. Performance indicator threshold: 70%. Examples: mild hemorrhage, minor head injury (no LOC), or moderate limb injury.
ATS Category 5 (Non-Urgent): For chronic or minor conditions where delay in assessment and treatment up to two hours is unlikely to affect the clinical outcome, or for clinico-administrative problems. Maximum waiting time: 120 minutes. Performance indicator threshold: 70%. Examples: minimal pain with no high-risk features, minor wounds not requiring sutures, or scheduled revisits.
Emergency departments commonly use specific colors as an adjunct to these numerical designations: Red (ATS 1), Orange (ATS 2), Green (ATS 3), Blue (ATS 4), and White (ATS 5).
While the ATS defines these performance indicator thresholds (e.g., 100% for ATS 1, 80% for ATS 2 to be seen within the target time) , actual performance data from health services often reveal that these targets are challenging to meet consistently, particularly for categories 2, 3, and 4. For example, one report indicated that for ATS Category 3, where the target is 75% of patients seen within 30 minutes, the actual performance was 18.8% in a given year. Such discrepancies highlight a potential gap between the ideal standards set by the triage scale and the complex operational realities of busy EDs. These realities are influenced by a multitude of factors extending beyond the triage system itself, such as overall patient volume, staffing levels, availability of inpatient beds (access block), and the efficiency of internal ED processes. This disparity raises questions about the realism of the targets in all contexts or, alternatively, points to systemic issues within healthcare delivery that prevent their achievement, even with a well-applied triage system.
3. Development, Regional Use (Australia/NZ), and Official Resources
The ATS was developed by the Australasian College for Emergency Medicine (ACEM). It evolved from a revision and update of the National Triage Scale (NTS), which had been in use in Australia since the early 1990s. The ATS was formally launched in Australia and Aotearoa New Zealand in the year 2000 and has been employed in all Australian EDs since approximately 1994 (referring to its NTS predecessor and subsequent ATS adoption).
ACEM has been the primary driving force behind the implementation, ongoing revision, and promulgation of the ATS. This includes the development of policies, guidelines for its use, and leading efforts to enhance its effectiveness. The foundational work on the ATS has been influential internationally, with several other triage scales, notably the Manchester Triage System (MTS) in the UK and the Canadian Triage and Acuity Scale (CTAS) in Canada, having been developed from or based on the principles of the ATS.
Official resources for the ATS are available through ACEM's website (acem.org.au), which hosts the ACEM Policy on the Australasian Triage Scale, Guidelines on the Implementation of the ATS in Emergency Departments, and an ACEM Literature Review on the ATS. Additionally, the Australian Government Department of Health and Aged Care provides the Emergency Triage Education Kit (ETEK), a teaching resource designed to promote consistent application of the ATS.
4. Reported Reliability, Validity, Strengths, and Limitations
Strengths: The ATS, as a five-level triage scale, is generally considered superior to older three- or four-level systems and is often regarded as a gold standard in emergency medicine for determining clinical urgency. It has been found to be a valid and reliable tool for nursing staff to assess the severity of incoming patients' conditions. The scale correlates well with important clinical and operational outcomes, including resource utilization, rates of admission for inpatient treatment, duration of emergency treatment, and the frequency of transfer to intensive care or mortality. The ATS provides a formalized and standardized process for triage, which was a key aim of its development.
Limitations: Despite its strengths, some limitations have been identified. The accurate and consistent recognition of ATS Level 5 patients by triage nurses has been reported as an area of concern. There is also a suggestion that the adult physiological predictors used within the ATS may not sufficiently differentiate between the criteria for Category 4 and Category 5, potentially contributing to lower accuracy in assigning Category 5. A significant limitation is that the ATS is not considered valid for determining waiting time performance indicators directly (despite setting maximums), nor for measuring patient severity beyond immediate urgency, patient complexity, ED workload, or staffing levels; these require separate measures. The reliability of the ATS has been found to be lower for the less acute triage categories (ATS 3, 4, and 5) compared to the high-acuity categories (ATS 1 and 2). Some studies have also suggested that the ATS may be inadequate for the correct evaluation of psychiatric patients.
Reliability and Validity: The ATS is considered valid for determining clinical urgency, with ATS Categories 1 and 2 demonstrating higher reliability than the lower categories. Overall inter-rater agreement has been reported as fair-to-good, with one study citing a Fleiss' kappa coefficient of 0.40. The lowest coefficient of reliability was observed for ATS Level 5. The implementation of nationally standardized triage nurse education programs in Australia is believed to have contributed to increased decision reliability in the application of the ATS.
5. Specific Applications
Pain Assessment: Pain is a significant factor in ATS categorization. "Very severe pain" of any cause is a clinical descriptor for ATS Category 2, indicating that humane practice mandates relief of such pain within 10 minutes. "Moderately severe pain" is a descriptor for ATS Category 3 (relief within 30 minutes), "moderate pain" (often with some risk features) for ATS Category 4 (relief within 60 minutes), and "minimal pain with no high risk features" for ATS Category 5. Pain intensity is commonly assessed using tools like the Numerical Rating Scale (NRS), ranging from 0 (no pain) to 10 (worst possible pain). Studies comparing patient-reported pain scores with nurse-assessed pain scores have often found discrepancies, with nurses tending to underestimate the patient's pain intensity.
Pediatric Adaptations: The same fundamental ATS categorization standards and principles of clinical urgency apply to pediatric patients presenting to the ED. While there isn't a distinctly named pediatric version of ATS in the same way as PaedCTAS, the World Health Organization's guidelines for Paediatric Emergency Triage, Assessment and Treatment (ETAT) provide definitions for key emergency signs in children (e.g., obstructed or absent breathing, severe respiratory distress, central cyanosis, signs of shock, coma, seizures, signs of severe dehydration) which align closely with the high-urgency principles of ATS Categories 1 and 2. It is recognized that critically ill children may initially appear stable but can deteriorate rapidly, underscoring the need for careful assessment.
Geriatric Adaptations: The ATS guidelines acknowledge that older persons often present with complex medical needs, and the potential impact of physiological, behavioral, and physical changes associated with aging on their presentation should be considered during triage. Standard trauma triage tools, which form part of the broader assessment landscape, often fail to accurately assess injury severity in older adults. This is due to factors such as age-related physiological changes (e.g., blunted heart rate response, different blood pressure norms), frailty, and polypharmacy, which can lead to both under-triage (delaying access to definitive care) and over-triage (unnecessary use of major trauma center resources). Incorporating frailty assessments and refining age-specific triage criteria are suggested strategies to improve precision in this population. No specific geriatric-focused ATS modification tool is detailed in the provided materials, but the general principles of thorough assessment and awareness of atypical presentations are crucial.
Mental Health Considerations: The ATS includes specific behavioral and psychiatric clinical descriptors for each of its five categories. For example, ATS Category 1 includes "Severe behavioural disorder with immediate threat of dangerous violence," while ATS Category 2 includes "Violent or aggressive (if): Immediate threat to self or others, Requires or has required restraint, Severe agitation or aggression." A dedicated mental health triage tool, designed as a quick reference guide, exists as part of the Emergency Triage Education Kit (ETEK). This tool details criteria for Immediate, Emergency, and Urgent mental health presentations, aligning them with the ATS categories and providing guidance on supervision and action. Despite these provisions, some critiques suggest that the standard ATS may not be as useful for clients presenting with mental illness compared to physical conditions, indicating a potential need for ongoing review or specialized approaches for this population.
E. South African Triage Scale (SATS)
1. Core Methodology: Physiological (TEWS) and Symptom-Based Discriminators
The South African Triage Scale (SATS) is a triage system specifically developed to prioritize patients based on a combination of physiological parameters and symptom-based clinical discriminators. Its core components are the Triage Early Warning Score (TEWS) and a defined list of clinical discriminators.
The TEWS is a composite physiological score. It is calculated by assigning numerical values (typically 0, 1, or 2) to various vital signs and observations, with a higher total score indicating greater physiological derangement and thus higher urgency. The parameters included in the TEWS are typically respiratory rate, heart rate, systolic blood pressure, body temperature, level of consciousness (often assessed using the AVPU scale - Alert, Voice, Pain, Unresponsive - or GCS), patient mobility, and exposure to trauma.
Clinical discriminators are specific signs, symptoms, or conditions (e.g., active bleeding, seizures, severe pain, specific high-risk presentations) that, if present, can directly determine the patient's triage category, sometimes overriding the TEWS score or being used in conjunction with it. An important feature of SATS is that it allows for the clinical judgment of a senior healthcare provider to override the systematically derived acuity score, acting as a "safety net" to prevent mis-triage in complex or atypical cases.
SATS was intentionally developed to be applicable in low-resource settings, a context common in South Africa and other Low- and Middle-Income Countries (LMICs). Its structure, which combines an objective physiological score (TEWS) with clear clinical discriminators, aims to provide a balance of objectivity and ease of use suitable for environments where advanced diagnostic capabilities or highly specialized staff may be limited. However, the successful application of SATS in these settings is not without challenges. Studies from some LMICs have reported significant rates of under-triage and incorrect TEWS calculations. This suggests that while the design of SATS is tailored for resource-constrained environments, its correct and consistent application is heavily dependent on adequate training, ongoing quality assurance, and the availability of basic equipment for vital sign measurement (e.g., thermometers, BP cuffs ). The very resource limitations that SATS aims to accommodate can, paradoxically, hinder its optimal implementation if these foundational human and material resource needs are not met.
The explicit inclusion of an override mechanism in SATS, allowing a senior healthcare provider's clinical judgment to supersede the scale-derived acuity , is a pragmatic feature. It acknowledges that no triage algorithm can perfectly capture every clinical nuance and rightly values the role of experienced clinical acumen. This "safety net" can be crucial for individual patient safety, particularly in atypical or rapidly evolving presentations. However, a frequent reliance on such overrides could also signal underlying issues. It might indicate limitations in the scale's sensitivity or specificity for certain patient groups or conditions, a lack of confidence or competence in applying the scale consistently among some users, or that experienced clinicians are routinely identifying critical factors that the scale does not adequately capture. Thus, while beneficial, a high rate of overrides might warrant investigation into the reasons to ensure the standard application of the scale is as robust as possible.
2. Acuity Levels (Colour-Coded) and Target Times
SATS typically prioritizes patients into one of four primary color-coded categories, although it is often described and validated as a five-tiered acuity system when including a category for deceased patients :
Red (Emergency): Indicates an emergency condition requiring immediate medical attention.
Orange (Very Urgent): Signifies a very urgent condition where treatment should be initiated within 10 minutes.
Yellow (Urgent): Applies to urgent conditions where treatment should commence within 60 minutes.
Green (Routine/Non-urgent): For routine or non-urgent conditions where patients can wait up to 240 minutes (4 hours) for treatment.
Blue (Deceased): This category is used to identify patients who are deceased upon arrival or after failed resuscitation attempts.
The SATS-N (Norwegian adaptation) training manual provides visual cues and criteria for Red, Orange, and Yellow priority levels based on "look for" signs and vital sign measurements.
3. Development, Use in LMICs, and Official Resources
SATS was developed in South Africa by the South African Triage Group (SATG), a multidisciplinary team comprising doctors, nurses, and paramedics. It was formerly known as the Cape Triage Score. The system was designed for nationwide use throughout South Africa and is applicable in both hospital Emergency Centres (ECs) and pre-hospital settings. It has been validated in public sector hospitals, private healthcare facilities, and by pre-hospital emergency medical services within South Africa.
A key characteristic of SATS is its widespread adoption and validation in Low- and Middle-Income Countries (LMICs) beyond South Africa, largely due to its design considerations for low-resource environments. For example, SATS has been implemented and studied in countries like Ghana , and its validity has been assessed in diverse settings such as Afghanistan, Haiti, and Sierra Leone.
Official resources, including the SATS training manual, are available through the Emergency Medicine Society of South Africa (EMSSA). Additionally, adapted versions like the SATS-N (Norwegian SATS) have their own user manuals.
4. Reported Reliability, Validity, Strengths, and Limitations
Strengths: SATS is generally considered a well-validated and reliable triage tool, particularly within its intended context of South Africa and other LMICs. It has demonstrated good validity in trauma-only settings in low-resource countries, accurately predicting an increased likelihood of mortality and hospitalization across incremental acuity levels. The TEWS component is regarded as a good fit for physiological assessment , and the system's use of simple color-coding aids in rapid communication of urgency.
Limitations: Despite its strengths, several studies have reported significant challenges with the implementation and consistent application of SATS. High rates of improper triage have been documented in some settings; for example, one study in Ethiopia reported that 92.4% of patients were improperly triaged, with 91% of those being under-triaged, and the TEWS score correctly calculated for only 7.6% of patients. Under-triage remains a significant concern, with rates varying across studies (e.g., 5.7% in a Ghanaian teaching hospital , and as high as 29.5% in a prehospital vignette-based study ). Over-triage has also been reported. Achieving the stipulated waiting time targets for each SATS category has proven difficult in some resource-constrained environments. Furthermore, the correct identification and application of clinical discriminators have been identified as a weak point, with one vignette study showing correct identification in only 58.8% of cases.
Reliability and Validity: SATS has been validated in various South African healthcare settings, including urban and rural regional hospitals, as well as district hospitals. It has shown good validity in predicting outcomes for 'green' (routine) and 'red' (emergency) patients, especially in trauma settings. However, a prehospital vignette-based study, while finding good inter-rater reliability for the overall SATS color and TEWS component, reported poor validity, primarily attributed to incorrect application or identification of the clinical discriminators.
5. Specific Applications
Pain Assessment: SATS explicitly incorporates pain assessment into its prioritization framework. Severe pain, typically defined as a score of ≥8 out of 10 on a pain scale, is a clinical discriminator that should prompt the clinician to categorize the patient as Orange (very urgent), requiring treatment initiation within 10 minutes.
Pediatric SATS (PSATS): A specific pediatric version of SATS, often referred to as PSATS, has been developed for children (generally defined as younger than 12 years or shorter than 150 cm). This version includes age-specific TEWS parameters and a distinct set of pediatric clinical discriminators to account for the unique physiological responses and presentations of illness in children. Guidelines like ETAT (Emergency Triage Assessment and Treatment), PSATS, and IMCI (Integrated Management of Childhood Illnesses) have been developed to facilitate pediatric triage in low-resourced environments.
Geriatric Adaptations: The TEWS component of SATS includes assessments of mobility and level of consciousness, which are relevant to geriatric patients who may present with functional decline or altered mental status. However, the provided materials do not detail specific geriatric modifications for SATS itself. It is noteworthy that in South Africa, downstream critical care triage guidelines, which may be influenced by initial SATS scores, have incorporated tools like the Clinical Frailty Scale. The use of such scales in resource allocation decisions has faced criticism for potentially discriminating against older adults by withholding ICU admission based on age, frailty, and comorbidities, particularly during periods of extreme resource constraint like pandemics. This highlights a complex ethical dimension in LMICs where initial triage by SATS might be appropriate, but subsequent resource allocation decisions can be heavily influenced by age and frailty considerations in a manner that has been contested.
Mental Health Considerations: SATS is primarily described as a physiology and symptom-based scale. The TEWS, a core component, focuses on physiological parameters such as vital signs and level of consciousness. While level of consciousness (e.g., AVPU) is assessed, the provided research snippets do not detail specific, nuanced mental health discriminators within SATS to the same extent as found in systems like ATS or CTAS. The emphasis appears to be more on physiological stability and overt, life-threatening symptoms.
III. Comparative Evaluation of Triage Systems
A comparative evaluation of the MTS, ESI, CTAS, ATS, and SATS reveals both shared goals and significant divergences in their frameworks for prioritization, performance metrics, adaptability to special populations, and implementation practicalities.
A. Frameworks for Prioritization: Similarities and Divergences
Similarities: A fundamental similarity is that most of these systems (MTS, ESI, CTAS, ATS, and effectively SATS when including the "Blue/Deceased" category) are five-level acuity scales. They all share the overarching aim of categorizing patients based on the urgency of their condition to ensure that those with the most critical needs receive care first. The initial assessment is typically conducted by trained nursing staff , and all systems unequivocally recognize that immediately life-threatening conditions demand prompt, often simultaneous, assessment and treatment.
Divergences: Despite these commonalities, the systems diverge significantly in their core logic for determining acuity:
MTS relies on a system of 52-53 presentational flowcharts selected based on the chief complaint, with priority determined by specific clinical discriminators within each flowchart.
ESI assesses acuity based on immediate life-saving needs and high-risk presentations for Levels 1 and 2. For Levels 3, 4, and 5, priority is uniquely determined by the anticipated number of resources required for patient disposition.
CTAS uses the patient's chief complaint (often aligned with CEDIS) as a starting point, then refines the acuity level through the application of first-order (physiological, pain, MOI) and second-order (complaint-specific, frailty, pregnancy) modifiers.
ATS determines clinical urgency based on general appearance, presenting problem, and key physiological predictors (airway, breathing, circulation, disability), directly linking each of its five categories to a maximum waiting time for medical assessment.
SATS combines a Triage Early Warning Score (TEWS), which is a composite physiological score, with a list of specific clinical discriminators to assign a color-coded priority level.
The consideration of resource utilization is an explicit component of the ESI algorithm for its lower acuity levels , whereas MTS notably excludes it from its primary decision-making. ATS guidelines state that it is not a tool for measuring workload or resource needs , while CTAS and SATS focus more directly on the patient's clinical state and physiological parameters.
The geographical origins and primary regions of use also reflect their developmental contexts: MTS in the UK and Europe, ESI predominantly in the US, CTAS in Canada, ATS in Australia and New Zealand, and SATS in South Africa and other LMICs. This can influence the implicit assumptions and patient populations for which they were initially optimized.
Furthermore, there is a varied emphasis on time targets. ATS, CTAS, and MTS explicitly define maximum waiting times or target times to physician assessment for each acuity level. ESI implies a temporal urgency through its acuity levels but does not set explicit minute-based targets in the same manner for all levels, focusing more on immediate intervention for Level 1 and risk for Level 2. SATS also incorporates target times for its color-coded categories.
The following table (Table 2) summarizes the acuity levels and associated target times for each system, facilitating a direct comparison of their operational outputs.
Table 2: Summary of Acuity Levels and Target Times for Reviewed Triage Systems
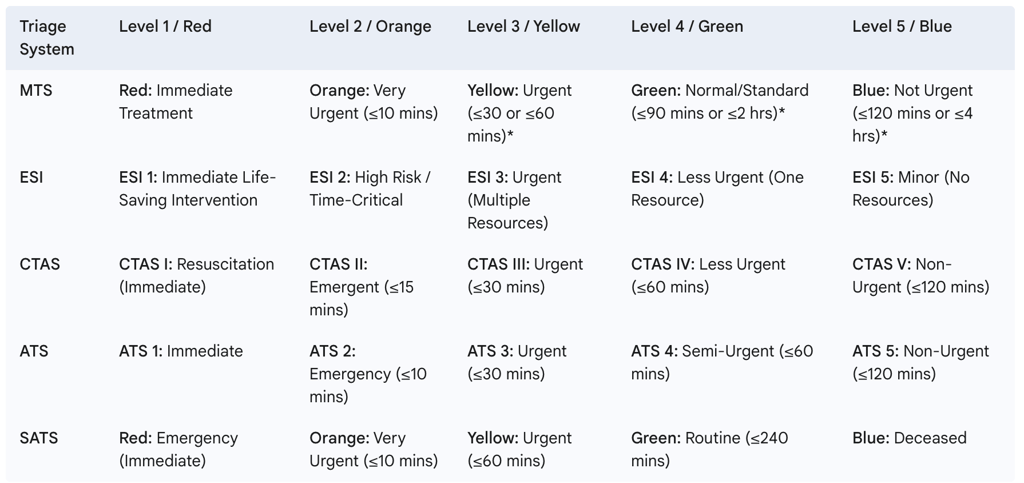
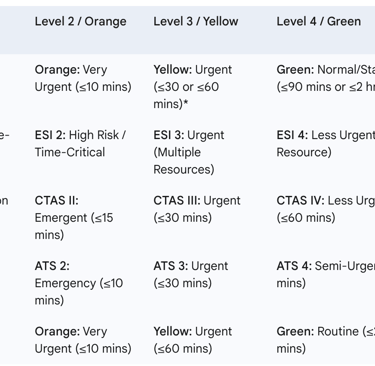
Note: MTS target times show some variation based on different sources/implementations.
B. Performance Across Key Metrics: Reliability, Validity, and Predictive Power
Reliability (Inter-rater agreement): The consistency with which different triage personnel assign the same acuity level to similar patients (inter-rater reliability) is crucial for any triage system. Generally, studies report moderate to substantial reliability for most of the reviewed systems. However, this can be influenced by the specific acuity level being assessed, the experience and training of the raters, and the nature of the patient presentation (e.g., mental health presentations for CTAS , or the lower acuity levels for ATS ).
MTS: Studies have reported weighted kappa values around 0.59 to 0.62, indicating moderate to substantial agreement.
ESI: A meta-analysis found a pooled kappa coefficient of 0.791, suggesting substantial agreement overall. Agreement tends to be higher with the latest adult versions of the scale and when used by expert raters.
CTAS: Reported kappa values show a wide range, from 0.202 (fair) to 0.84 (almost perfect) in a meta-analysis. A study in a non-Canadian setting found a kappa of 0.42 (moderate) , while for mental health presentations, a kappa of 0.312 (fair) was reported.
ATS: Overall inter-rater agreement has been described as fair-to-good (Fleiss' kappa 0.40), with the lowest reliability noted for ATS Level 5.
SATS: A prehospital vignette study indicated good inter-rater reliability for the final SATS color and TEWS component, though lower for clinical discriminators.
Validity (Accuracy and Predictive Power): Validity refers to the extent to which a triage system accurately reflects a patient's true urgency and predicts relevant outcomes such as hospitalization, mortality, or resource utilization. All five systems have generally been validated to predict such outcomes, albeit with varying degrees of success and in different contexts.
A common challenge across all systems is the occurrence of both under-triage (assigning a lower acuity than warranted) and over-triage (assigning a higher acuity than warranted). Under-triage is a particularly significant patient safety concern, as it can lead to delays in care for critically ill patients. Specific validity challenges identified include:
The MTS "unwell adult" flowchart showing lower predictive ability for older patients.
The ESI Level 3 category often becoming a large, undifferentiated pool of patients.
The ATS experiencing difficulties in consistently differentiating Categories 4 and 5.
SATS facing issues with the correct application of clinical discriminators in some settings.
C. Adaptability to Special Populations (Pediatrics, Geriatrics, Mental Health)
The accurate triage of special patient populations, including children, older adults, and individuals with mental health presentations, poses unique challenges that each system addresses with varying degrees of specificity.
Pediatrics: Most systems have developed specific adaptations or provide dedicated guidelines for triaging children.
MTS: Incorporates age-dependent modifications and dedicated pediatric flowcharts like "Crying Baby," "Irritable Child," and "Unwell Child".
ESI: Recommends use in conjunction with the Pediatric Assessment Triangle (PAT) and a focused pediatric history. The ESI handbook includes a chapter on pediatric triage.
CTAS: Features the Paediatric CTAS (PaedCTAS), a formally developed and widely used version tailored for children.
ATS: While the same core categorization standards apply, pediatric emergency signs (e.g., from ETAT guidelines) align with ATS high-urgency principles.
SATS: Includes a Pediatric SATS (PSATS) with age-specific TEWS parameters and pediatric discriminators.
Geriatrics: Triaging older adults is complicated by atypical presentations of illness, multiple comorbidities, polypharmacy, and frailty.
MTS: Research has explored integrating frailty screening tools (e.g., PRISMA-7) with MTS. Limitations of the "unwell adult" flowchart for this group are noted.
ESI: Studies have indicated that ESI may under-appreciate severity in elderly patients. General geriatric ED care guidelines are relevant but no specific ESI modification is detailed.
CTAS: Has introduced a specific frailty modifier to help identify at-risk older adults and provides a geriatric guidance document.
ATS: General considerations for the impact of aging on presentation are included in guidelines. Standard trauma triage tools, often used alongside ATS, frequently underperform in older trauma patients.
SATS: The TEWS component includes mobility and LOC assessment, relevant for geriatrics. However, concerns have been raised in the South African context about downstream critical care triage decisions for the elderly based on frailty scores, which may be influenced by initial SATS categorization.
Mental Health: Approaches to mental health triage vary.
MTS: Includes specific flowcharts like "Behaving strangely" and "Mental illness". A separate UK Mental Health Triage Scale (MHTS) exists for specialist telephone triage, distinct from the ED-based MTS.
ESI: Conditions like "altered mental status" or "actively suicidal/homicidal patient" can lead to an ESI Level 2 assignment.
CTAS: Includes mental health as a CEDIS presenting complaint category. Studies have shown fair inter-rater reliability for mental health scenarios using CTAS.
ATS: Provides specific behavioral descriptors for each triage category and has an associated mental health triage tool as part of the ETEK. However, some critiques question the utility of the standard ATS for mental illness presentations.
SATS: Focuses primarily on physiological parameters and overt symptoms; detailed nuanced mental health discriminators are less prominent in the available descriptions compared to other systems.
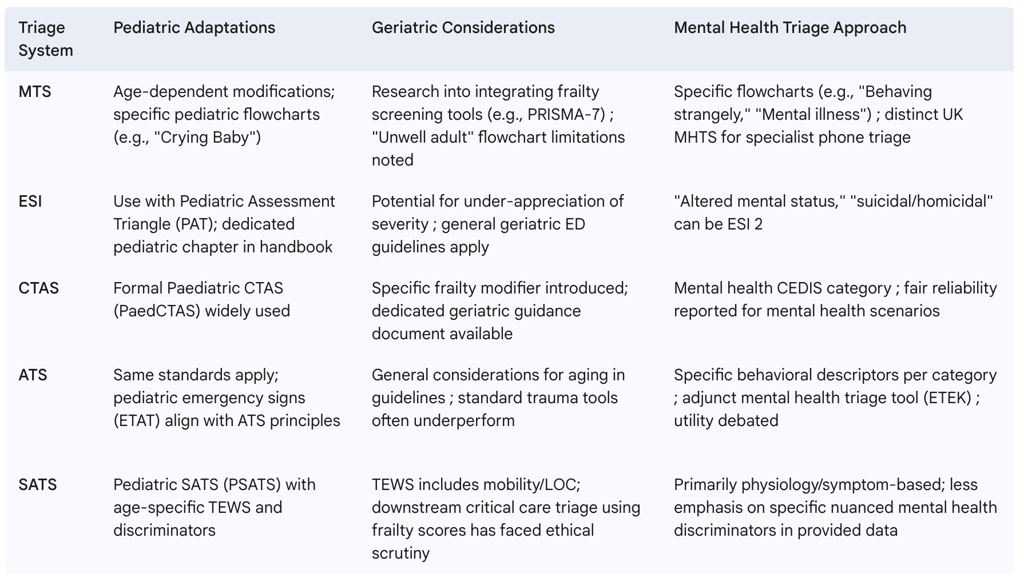
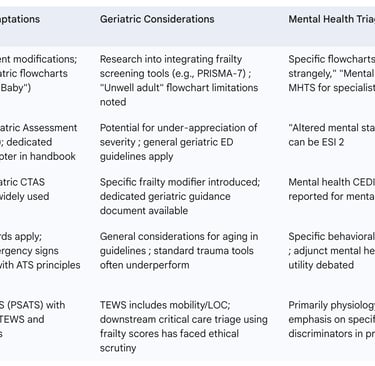
The following table (Table 3) summarizes the approaches of each system to these special populations.
Table 3: Comparative Overview of Special Population Adaptations
D. Ease of Use, Training Requirements, and Implementation Challenges
Ease of Use: Subjective ease of use can influence adoption and consistent application. ESI is often noted for its ease of use , and MTS is described as straightforward to understand. The ATS assessment aims for brevity (2-5 minutes). SATS was designed with LMIC contexts in mind, implying an aim for relative simplicity in application.
Training Requirements: All systems necessitate adequately trained personnel, typically experienced ED nurses.
MTS: Training is available through ALSG and associated course centers.
ESI: Recommendations include at least one year of ED experience plus completion of a comprehensive ESI training program (often 2-4 hours internally with annual refreshers). Lack of adequate education is linked to reduced precision.
CTAS: NENA provides courses and educational materials.
ATS: The Emergency Triage Education Kit (ETEK) serves as a key training resource.
SATS: Standardized training materials are available, often through EMSSA.
Implementation Challenges: Successful implementation is often hampered by systemic and human factors.
ED Overcrowding: This pervasive issue affects the ability of any triage system to achieve its goals of timely care.
Human Factors: Human error and cognitive biases can lead to inconsistencies in MTS and other systems.
Under/Over-triage: This remains a common problem across all systems, impacting patient safety and resource allocation.
Resource Constraints: Limited staff, equipment, or downstream capacity (e.g., inpatient beds) can negate the benefits of even accurate triage.
Achieving Time Targets: Meeting the prescribed waiting time targets is a consistent challenge, as seen with ATS and SATS.
System-Specific Challenges: These include consistent application of complex rules like CTAS modifiers , or correct use of TEWS and discriminators in SATS, particularly in high-pressure or low-resource settings.
Data and Technology: For emerging digital and AI-based triage tools, challenges include ensuring data quality, algorithm reliability and fairness, and effective integration into clinical workflows.
The choice between these systems often involves a trade-off. Systems like ATS, with their primary focus on urgency and a rapid assessment timeframe of 2-5 minutes , offer speed and a clear, universally understandable framework. This simplicity can be an advantage for rapid initial sorting. Conversely, systems that incorporate more complex decision trees or extensive sets of modifiers, such as MTS with its 52-53 flowcharts , CTAS with its first and second-order modifiers , or ESI with its multi-step algorithm including resource prediction , may offer a more nuanced and potentially more comprehensive assessment. However, this increased complexity can also demand more cognitive effort from the triage clinician, necessitate more intensive and ongoing training, and potentially impact inter-rater reliability if not consistently applied or well-supported by decision aids. SATS attempts to strike a balance by combining an objective physiological score (TEWS) with a list of clear clinical discriminators, designed for usability in LMICs , yet even its application can be challenging as noted.
Ultimately, while five-level triage scales are generally considered superior to older, simpler systems , and individual systems like ATS are sometimes referred to as a "gold standard" within specific contexts or for particular aspects of triage , the consistent reporting of under-triage and over-triage across all reviewed systems is telling. Coupled with the evident need for local adaptations—such as the Extended MTS , the CTAS frailty modifier , or various pediatric-specific modifications—this suggests that no single triage system is universally perfect or a one-size-fits-all solution. The "best" system is likely one that is carefully chosen to match the specific ED's patient demographics, resource availability, staff experience levels, and the institution's capacity for ongoing quality improvement and training. The concept of a single, definitive "gold standard" triage system is challenged by the evidence of continuous refinement, context-specific performance issues, and the diverse philosophical approaches embodied by these established tools.
IV. The Evolving Landscape of Emergency Triage
A. Historical Milestones in Triage System Development
The practice of triage, though formalized in recent centuries, has ancient roots in prioritizing care during times of mass casualty. Its modern history is often traced back to military medicine during the Napoleonic Wars, with figures like Baron Dominique-Jean Larrey and Baron Pierre-François Percy developing systems for sorting and evacuating wounded soldiers. Larrey's concept of the "ambulance volante" (flying ambulance) emphasized rapid evacuation and organized care.
Triage systems continued to evolve through major conflicts of the 19th and 20th centuries. World War I saw the development of more structured approaches, and by World War II, tiered systems for evacuation and staged care were common. The Korean War was pivotal in establishing the tiered categories still fundamental to many systems today: immediate, delayed, minimal, and expectant. This era also saw medical advancements, like understanding shock, integrated earlier into the triage process, alongside the advent of MASH units and helicopter evacuation. The Vietnam War further refined prehospital care with the introduction of helicopter medics capable of providing interventions en route, significantly reducing time to definitive care.
These military-driven innovations gradually transitioned into civilian emergency medical services and hospital emergency departments from the mid-1960s onwards. Early civilian triage systems were often trauma-based, reflecting their battlefield origins. The contemporary challenge for triage has been to develop systems capable of managing the full spectrum of medical and traumatic conditions, across all age groups, from the critically ill to those with minor complaints. This led to the development and widespread adoption of standardized five-level triage scales, such as MTS, ESI, CTAS, and ATS, predominantly from the 1990s onwards, aiming for greater objectivity and consistency in ED prioritization.
B. Innovations in Pre-hospital Triage
The principles of triage are not confined to the hospital ED; effective pre-hospital triage is crucial for directing patients to the most appropriate level of care and preparing receiving facilities. Several of the reviewed hospital-based systems have adaptations or specific considerations for pre-hospital use:
Prehospital CTAS is well-established in Canada, with specific guidelines for paramedics that include assigning both an "Arrival CTAS" and a "Departure CTAS" to track changes in patient condition and guide transport decisions.
SATS was explicitly designed for dual use in both hospital Emergency Centres and pre-hospital settings in South Africa and other LMICs, acknowledging the need for a robust tool in environments where pre-hospital resources may be limited.
Beyond these general systems, specialized pre-hospital triage tools have emerged for specific time-sensitive conditions. For acute stroke, scales such as FAST (Face-Arm-Speech-Time), RACE (Rapid Arterial oCclusion Evaluation), and G-FAST (Gaze-FAST) are used by EMS personnel to identify potential large vessel occlusion (LVO) strokes and expedite transport to stroke centers capable of endovascular therapy (EVT). Mobile Stroke Units (MSUs), ambulances equipped with CT scanning capabilities, represent a more advanced pre-hospital triage and treatment innovation, allowing for earlier diagnosis and initiation of thrombolysis in the field.
Internationally, collaborative efforts have also produced tools like the Interagency Integrated Triage Tool (IITT), developed by the WHO, ICRC, and Médecins Sans Frontières (MSF). The IITT provides integrated protocols for routine facility-based triage of adults and children using a simplified three-color system (Red: high acuity, Yellow: moderate acuity, Green: low acuity) and is intended for use in emergency units, including those in humanitarian or low-resource settings. While primarily for facilities, its interagency nature and design for diverse contexts suggest broad applicability.
C. The Role of Digital Health Tools and Artificial Intelligence in Modern Triage
The landscape of emergency triage is being reshaped by the advent of digital health technologies and Artificial Intelligence (AI). These innovations aim to enhance efficiency, consistency, and accuracy in the complex triage process.
Digital Health Tools: Various digital tools are being implemented to support and streamline triage:
Digital Check-in Kiosks: These systems allow patients to self-register demographic information, presenting complaints, and medical history upon arrival at the ED. The goal is to automate initial intake processes, potentially reducing administrative workload, shortening wait times, and improving patient flow. Some kiosks also incorporate preliminary triage assistance functions.
Symptom Checkers and Virtual Triage Platforms: Online tools and mobile applications (e.g., Infermedica) are increasingly available to patients for self-assessment of symptoms prior to seeking care. These platforms use algorithms to analyze patient-inputted data, provide a list of possible conditions, suggest an appropriate level of care (e.g., self-care, telehealth, ED visit), and navigate them to relevant services. Some are designed to integrate with healthcare provider systems.
Clinical Decision Support and Process Analysis Tools: Software like Codimg enables video recording and analysis of the triage process. This can be used for quality assurance, training, and research to assess consistency in triage decisions across different staff and shifts, identify areas for improvement, and provide objective feedback to triage personnel.
Artificial Intelligence (AI) in Triage: AI holds significant promise for transforming ED triage by leveraging machine learning algorithms to analyze vast amounts of real-time patient data, including vital signs, medical history, and presenting symptoms.
Enhanced Prioritization and Efficiency: AI-driven triage systems aim to automate and standardize aspects of the triage process, potentially improving consistency and reducing reliance on purely subjective assessments. By rapidly processing multiple data points and recognizing complex patterns, AI can assist in more precise risk stratification, identifying patients at higher risk of deterioration (e.g., in sepsis, stroke, cardiac events) and prioritizing their care accordingly. Studies have suggested that AI-informed triage can lead to improved patient flow, decreased ED length of stay, and more rapid identification of both high-risk and low-risk patients.
Clinical Decision Support: AI tools can reduce the cognitive burden on triage clinicians by pre-processing information and highlighting key risk factors, allowing healthcare professionals to focus their expertise on the most complex cases or on the human aspects of patient interaction. The goal is often to augment, not replace, human judgment.
The evolution of triage from its origins in simple manual sorting during mass casualty events on the battlefield to the sophisticated, data-driven algorithms now being embedded in digital platforms represents a fundamental paradigm shift. The trajectory points towards increasingly advanced AI-powered decision support systems. These systems have the potential to offer greater precision in risk stratification and improved operational efficiency. However, this technological advancement also introduces new and complex challenges, particularly concerning data governance, the potential for algorithmic bias, ensuring transparency in decision-making, and defining the optimal interaction between human clinicians and AI tools.
Despite the considerable potential of AI in triage, it is crucial to recognize that current research and expert consensus emphasize the continued, indispensable role of human decision-making and clinical judgment. AI is predominantly positioned as a powerful clinical decision support tool, designed to augment the capabilities of healthcare professionals rather than to replace them entirely. This perspective suggests that the most effective and safest future triage models will likely be synergistic, combining the analytical power and speed of AI with the nuanced understanding, ethical reasoning, and empathic communication skills of human experts. This "human-in-the-loop" approach will be critical for handling situations involving high degrees of uncertainty, atypical presentations, or complex ethical considerations that current algorithms may struggle to address adequately.
Challenges for Digital/AI Implementation: The widespread adoption of these advanced tools is not without hurdles. Key challenges include:
Data Quality and Algorithm Reliability: AI models are highly dependent on large, high-quality datasets for training and validation. Ensuring the accuracy, completeness, and representativeness of this data is paramount.
Bias Mitigation: Algorithms can inadvertently perpetuate or even amplify existing biases present in historical data, potentially leading to disparities in care if not carefully designed and audited.
Transparency and Trust: The "black box" nature of some AI algorithms can be a barrier to clinician trust. Ensuring transparency in how AI tools arrive at their recommendations is important for acceptance and accountability.
Integration and Training: Seamless integration of new digital tools into existing ED workflows and electronic health record systems is a technical and logistical challenge. Adequate training for clinical staff on how to use these tools effectively and understand their limitations is also essential.
Ethical Governance: Establishing clear ethical guidelines and governance frameworks for the use of AI in healthcare decision-making is crucial.
V. Conclusion and Strategic Insights
A. Synthesizing Key Differences and Strengths
This comprehensive analysis of the Manchester Triage System (MTS), Emergency Severity Index (ESI), Canadian Triage and Acuity Scale (CTAS), Australasian Triage Scale (ATS), and South African Triage Scale (SATS) underscores the global effort to standardize and optimize patient prioritization in emergency care. While all five systems primarily utilize a five-level acuity structure and aim to ensure timely care for the most critical patients, they achieve this through distinct methodologies.
MTS employs a highly structured, symptom-driven approach using an extensive set of presentational flowcharts and clinical discriminators, primarily in the UK and Europe. Its strength lies in its detailed, protocolized nature.
ESI, predominant in the US, uniquely combines acuity assessment with the prediction of anticipated resource utilization for lower-acuity patients, directly linking triage to operational capacity.
CTAS, the Canadian standard, offers a nuanced assessment through its use of chief complaints refined by a comprehensive list of first and second-order clinical and physiological modifiers, and notably features strong prehospital integration.
ATS, originating from Australia and New Zealand, focuses sharply on clinical urgency defined by physiological predictors and explicit maximum waiting times, providing a clear, time-centric framework.
SATS, developed for South Africa and other LMICs, balances physiological assessment via the Triage Early Warning Score (TEWS) with key clinical discriminators, designed for applicability in resource-constrained settings.
Each system has demonstrated strengths: MTS in its systematic guidance, ESI in its operational linkage through resource prediction, CTAS in its capacity for nuanced clinical modification and prehospital utility, ATS in its unambiguous focus on urgency, and SATS in its tailored design for LMICs.
B. Considerations for System Selection and Implementation
The selection and implementation of a triage system is a critical decision for any emergency department and should be guided by a careful assessment of the local context. Factors to consider include:
Patient Demographics: The prevalence of pediatric, geriatric, or mental health presentations may favor systems with more robust or specific adaptations for these groups.
Resource Availability: Systems like ESI that explicitly consider resources may align well with highly managed environments, while SATS is designed for settings where resources are scarce.
Staff Experience and Training Capacity: More complex systems with numerous rules or modifiers (e.g., CTAS, MTS) may require more intensive and ongoing training compared to systems with a simpler core logic if high reliability is to be achieved.
Digital Infrastructure: The capacity to support digital versions of triage systems or integrate AI-driven tools will influence future adaptability.
Regardless of the system chosen, successful implementation hinges on robust initial and ongoing training programs, continuous quality assurance monitoring to identify and mitigate under- and over-triage, and a culture of regular review and feedback. Local adaptation and validation may be necessary to optimize performance, but this should be done cautiously to maintain the core integrity and evidence base of the chosen system. Strong clinical leadership and multidisciplinary team involvement are paramount throughout the selection, implementation, and quality improvement cycle.
C. Future Research and Development Imperatives
The field of emergency triage is continuously evolving, and several areas warrant further research and development:
Enhanced Reliability and Validity Studies: Continued investigation into the reliability and validity of all triage systems across diverse international settings, patient populations (especially vulnerable groups), and by different cadres of healthcare workers is needed.
Improved Adaptations for Special Populations: Further development and rigorous validation of more nuanced and integrated approaches for geriatric patients (e.g., standardized frailty assessment within triage) and those with acute mental health conditions are essential.
Addressing "Mid-Acuity Congestion": For systems like ESI where a large, undifferentiated group of mid-acuity patients (e.g., ESI Level 3) emerges, research into sub-stratification methods or care pathways for this cohort could improve flow and resource allocation.
Ethical AI and Digital Tool Development: The advancement of AI and digital triage tools must prioritize ethical considerations, including algorithmic transparency, bias detection and mitigation, data security, and ensuring that these tools genuinely support, rather than supplant, clinical judgment. Validation in real-world clinical workflows is critical.
Patient-Centered Outcomes: Research should expand beyond ED operational metrics (like waiting times or length of stay) to evaluate the impact of different triage systems and processes on longer-term, patient-centered outcomes, such as functional status, health-related quality of life, and patient experience.
Optimizing Training and Decision Support: Investigating the most effective training methodologies and forms of decision support (e.g., embedded digital aids, real-time feedback) to improve triage accuracy, reduce cognitive load, and enhance consistency is crucial.
The comprehensive review of these five major triage systems reveals a critical truth: while all aim to optimize the initial stages of emergency care, none represent a flawless or universally applicable solution. Each system possesses inherent strengths tailored to certain priorities—be it structured symptomatology (MTS), resource awareness (ESI), clinical nuance (CTAS), temporal urgency (ATS), or LMIC applicability (SATS)—but also exhibits weaknesses or faces challenges in specific contexts or with particular patient groups. The persistent issues of under-triage and over-triage, the documented need for local adaptations and specialized guidelines for populations like children or the elderly, and the ongoing exploration of new technologies such as AI, all underscore that emergency triage is not a static, perfected science.
Rather, it is a dynamic and evolving process. The imperfections inherent in current systems, however, do not diminish the essential and indispensable role of standardized triage in managing the complex, high-stakes environment of emergency care. In the absence of such systems, patient prioritization would be ad-hoc, inconsistent, and likely inequitable. Therefore, the continuous pursuit of refinement—through research, education, technological innovation, and thoughtful adaptation—remains the imperative. The ultimate goal is to make these vital systems as safe, efficient, and equitable as possible, ensuring that all patients receive the right care, at the right time, according to their clinical need.
Conclusion
As emergency departments worldwide continue to face increasing patient volumes, resource constraints, and complex healthcare needs, the selection and implementation of an appropriate triage methodology remains a critical determinant of clinical outcomes and operational efficiency. Our comparative analysis of the five major triage systems—MTS, ESI, CTAS, ATS, and SATS—reveals that each offers distinct advantages that may prove decisive in specific healthcare contexts. The Manchester Triage System provides unparalleled standardization and reproducibility, making it ideal for large healthcare networks seeking consistency across multiple sites. The Emergency Severity Index uniquely balances clinical urgency with resource utilization predictions, offering particular value in cost-conscious healthcare environments. The Canadian Triage and Acuity Scale delivers the most comprehensive clinical assessment framework, benefiting settings where detailed evaluation and frequent reassessment can be supported. The Australasian Triage Scale achieves an effective balance between simplicity and clinical accuracy, particularly when backed by robust quality assurance mechanisms. The South African Triage Scale demonstrates that effective triage is possible even in resource-limited environments, providing a model for healthcare systems developing their emergency care capabilities. As technology continues to enhance implementation possibilities and adaptation to specific healthcare contexts progresses, the future of emergency triage lies not in the dominance of any single methodology but in thoughtful integration of principles from each system, guided by local realities and emerging evidence. The optimal approach ultimately depends not on which system is "best" in absolute terms, but on which best aligns with specific organizational needs, patient populations, and resource environments. By applying the insights from this comparative analysis, healthcare leaders can make informed decisions that enhance their emergency departments' ability to deliver the right care to the right patients at the right time—the fundamental purpose that unites all triage systems regardless of their methodological differences.
FAQ Section
Which triage system is most widely used globally in 2025? The Manchester Triage System (MTS) remains the most widely implemented system globally, with particular dominance in Europe, parts of South America, and numerous Asian countries. The ESI follows closely behind, with strong adoption throughout North America and increasing implementation in Middle Eastern healthcare systems.
How long does it take to train staff in each triage methodology? Training requirements vary significantly: SATS requires approximately 8-16 hours of basic instruction, ATS and ESI typically require 16-24 hours plus supervised practice, MTS demands 24-32 hours with certification, and CTAS is the most intensive with 40+ hours of training plus competency assessment.
Which triage system performs best for pediatric patients? CTAS has demonstrated the highest accuracy rates for pediatric presentations due to its comprehensive age-specific modifiers and specialized pediatric protocols. The 2023 update to MTS has significantly improved its pediatric performance, bringing it close to CTAS in recent comparative studies.
Can different triage systems be used within the same healthcare network? Yes, some healthcare networks implement different systems based on specific facility needs. For example, a major trauma center might utilize CTAS or MTS while affiliated urgent care centers implement the simpler ESI or adapted SATS protocols for lower-acuity presentations.
How do the five triage systems compare in identifying sepsis? Recent studies show CTAS and MTS achieve the highest sensitivity for early sepsis detection (88% and 86% respectively), followed by ESI (82%), ATS (80%), and SATS (75%). However, when technology-enhanced versions are implemented, these differences narrow significantly.
What is the average cost to implement each triage system? Implementation costs vary dramatically based on facility size and approach: basic paper-based SATS implementation can cost under $5,000 for a small facility, while comprehensive electronic MTS or CTAS systems with full EHR integration typically range from $100,000 to $750,000 for large emergency departments.
Which system performs best in mass casualty incidents? Modified versions of SATS have demonstrated superior performance in mass casualty incidents due to the system's emphasis on rapid assessment and minimal resource requirements. Specialized mass casualty adaptations of ESI have also shown effectiveness when implemented with proper training.
How do these triage systems address language barriers? MTS and CTAS have the most developed multilingual resources, with official translations in 25+ languages. Technological solutions including AI-powered translation tools are increasingly integrated with all five systems to address language barriers in diverse patient populations.
Which system has the highest inter-rater reliability? Current data shows that properly implemented MTS achieves the highest inter-rater reliability (84-87%), followed closely by CTAS (82-85%), ATS (80-83%), ESI (78-81%), and SATS (75-79%), though performance varies based on staff experience and training quality.
How are these triage systems adapting to telemedicine? MTS and ESI have developed the most robust telehealth adaptations, with structured assessment protocols designed specifically for virtual patient evaluation. CTAS introduced its comprehensive telehealth module in late 2024, while ATS and SATS are in earlier stages of telehealth integration.
Additional Resources
World Health Organization Emergency Triage Assessment and Treatment (ETAT) Guidelines, 2024 Edition
Journal of Emergency Nursing Special Issue: Global Triage Methodologies in the Post-Pandemic Era (March 2025)
International Federation for Emergency Medicine: Comparative Analysis of Triage Systems Implementation Guide (2024)
Emergency Nurses Association Triage Qualification Program: Multi-System Approach (Online Resource, Updated January 2025)
Robertson-Steel I, Edwards S, et al. "The Evolution of Modern Triage: From Battlefield to Emergency Department." Oxford University Press, 2023.
