Triage Methodologies in Mass Casualty Events: START, SALT, and RAMP
This report provides a comprehensive analysis of three prominent triage methodologies: Simple Triage And Rapid Treatment (START), Sort-Assess-Lifesaving Interventions-Treatment/Transport (SALT), and Rapid Assessment of Mental Status and Pulse (RAMP).


Mass casualty incidents (MCIs) present unique challenges to emergency medical services, often overwhelming available resources and necessitating a shift from individual-focused care to maximizing overall survival. Triage, the process of rapidly categorizing patients based on injury severity and resource needs, is a critical component of effective MCI response. This report provides a comprehensive analysis of three prominent triage methodologies: Simple Triage And Rapid Treatment (START), Sort-Assess-Lifesaving Interventions-Treatment/Transport (SALT), and Rapid Assessment of Mental Status and Pulse (RAMP).
The analysis reveals that each system offers distinct advantages and inherent limitations. START is widely recognized for its speed and simplicity, making it ideal for initial rapid assessment by first responders. However, its broad physiological thresholds can lead to significant over-triage and may not adequately differentiate among critically injured patients. SALT, developed as a more standardized and comprehensive approach, integrates early life-saving interventions and introduces a resource-based expectant category, enhancing accuracy and ethical resource allocation but potentially adding complexity. RAMP, an even more streamlined system, prioritizes extreme speed in high-threat environments by focusing on only two critical physiological parameters, though this simplification can result in higher rates of misclassification.
A fundamental challenge across all MCI triage systems is the tension between the need for rapid assessment in chaotic environments and the desire for precise patient categorization. While military experience informs civilian protocols, direct transferability and efficacy in civilian contexts remain unproven, highlighting the continuous need for adaptation, robust validation studies, and ongoing training to optimize outcomes in real-world disaster scenarios.
What us Mass Casualty Triage?
Definition and Purpose
Triage, a term originating from the French word for "sorting," is the systematic process of categorizing patients based on the severity of their injuries and their immediate need for medical intervention and transportation during a mass casualty incident (MCI). The primary objectives of triage in such events are to quickly ascertain the number of casualties, classify them according to injury severity, prioritize their treatment and transportation, and provide initial stabilization for life-threatening conditions until more extensive resources become available. In situations where medical resources are limited or overwhelmed by the sheer volume of injured individuals, the overarching goal of triage shifts from providing optimal care for each individual patient to achieving "the greatest good for the greatest number" of people. This utilitarian approach is a cornerstone of MCI management, guiding the allocation of scarce resources to maximize overall survival.
Historical Context and Evolution
The foundational strategies of modern triage emerged from military medicine, with its roots tracing back to battlefield practices. Baron Dominique-Jean Larrey, a French military surgeon, is widely credited with developing one of the earliest battlefield triage systems during the Napoleonic Wars. His novel approach in 1812 advocated for the immediate treatment of the most severely wounded, rather than deferring care until the cessation of hostilities, which was the prevailing custom at the time. As military conflicts evolved, so did triage principles. In 1846, British surgeon John Wilson proposed a different philosophy, suggesting that treatment should prioritize patients most likely to benefit from immediate intervention, deferring care for both minor injuries and those with severe, likely fatal wounds. During World War I, the United States adopted a triage strategy aimed at maximizing the number of soldiers who could swiftly return to combat, prioritizing those who could be treated quickly to maintain fighting force strength. Later conflicts, such as the Korean and Vietnam Wars, saw a shift from extensive on-scene treatment to rapid evacuation of wounded soldiers to well-equipped medical facilities, facilitated by advancements in ground and air transport.
The Need for Standardized Systems in Civilian MCIs
Despite the valuable lessons learned from military medicine, recent catastrophic global disasters have exposed significant deficiencies in civilian emergency preparedness and the application of triage protocols. A notable disparity exists between military and civilian operational expertise in disaster triage. Military forces often engage in frequent, rigorous drill training, fostering a high level of proficiency and standardized responses. In contrast, civilian society typically lacks this consistent, high-frequency training, which impacts the seamless execution of disaster triage.
A critical challenge arises from the inherent difficulty in conducting randomized clinical trials in disaster medicine, making it practically impossible to rigorously test and compare the efficacy of various triage protocols in real-world MCI settings. Consequently, the optimal application of military-derived triage protocols to civilian populations remains unproven. This situation highlights a crucial gap: while military experience provides a valuable foundation, direct transferability and confirmed efficacy of these protocols in civilian contexts are not fully established. This necessitates that civilian triage systems be meticulously adapted and validated within their unique operational environments, which often differ significantly from military theaters and lack the structured, high-frequency training of military forces. The absence of a unified national standard for mass casualty triage in the United States further complicates multi-agency responses, as incidents frequently cross jurisdictional lines involving diverse responders. This underscores the pressing need for consistent, evidence-based guidelines tailored for civilian emergency management
Simple Triage And Rapid Treatment (START)
Core Principles and Protocol (RPM)
The Simple Triage And Rapid Treatment (START) system is a widely adopted, fast, and efficient methodology for categorizing victims during mass casualty incidents. Developed in 1983 by the Newport Beach Fire Department and Hoag Hospital in California, START enables first responders to triage multiple patients in 30 seconds or less. The system's core is built upon three primary physiological observations: Respiration, Perfusion, and Mental Status (RPM). This rapid assessment aims to quickly identify the most seriously injured patients who require immediate attention, prioritizing their stabilization and transportation.
Detailed Steps of the Algorithm
The application of the START algorithm follows a systematic progression:
Initial Scene Assessment: Upon arrival at the incident scene, the first responder's priority is to remain calm, survey the environment, and gather an overview of the situation. A concise verbal report is then communicated to the dispatch center, detailing the incident's location, type, any immediate hazards, and an estimated number of victims. This initial report sets the operational stage for the entire response.
Step 1: "Walking Wounded" (Green/Minor): The first action in START triage is to instruct all individuals who are able to get up and walk to move to a designated safe area, often referred to as a Casualty Collection Point. These patients are initially categorized as "green" or "minor" because their ability to ambulate suggests they are not at immediate risk of death. It is understood that these individuals will require re-triage later as more medical resources become available.
Step 2: Assess Non-Ambulatory Patients (RPM): Following the initial sorting of ambulatory patients, responders systematically move through the remaining victims, conducting a quick assessment of each individual. This assessment should ideally take no more than one minute per patient. The assessment focuses on the RPM parameters:
Respirations (R): The first physiological parameter assessed is breathing. If a patient is not breathing, their airway is repositioned (e.g., via head tilt/chin lift). If spontaneous breathing does not resume after this intervention, the patient is classified as "deceased" (black tag). The protocol explicitly states that there is no time for cardiopulmonary resuscitation (CPR) in an MCI setting. If the patient is breathing, their respiratory rate is determined. A respiratory rate exceeding 30 breaths per minute immediately classifies the patient as "Immediate" (red tag). If the respiratory rate is less than 30 breaths per minute, the assessment proceeds to Perfusion.
Perfusion (P): The next step involves assessing the patient's circulatory status. This can be done by checking for a radial pulse or evaluating capillary refill time. The presence of a radial pulse is generally preferred over capillary refill due to the latter's susceptibility to environmental factors, such as cold temperatures, which can lead to inaccurate readings. If a radial pulse is absent or capillary refill is greater than 2 seconds, the patient is tagged "Immediate" (red). If a radial pulse is present (or capillary refill is less than 2 seconds), the assessment moves to Mental Status.
Mental Status (M): The final assessment criterion is the patient's neurological status, determined by their ability to follow simple commands. If the patient is unable to follow simple commands or exhibits confusion or an altered mental status, they are classified as "Immediate" (red), as these signs may indicate a head injury or another critical condition. If the patient is able to follow simple commands and demonstrates a normal mental status, they are categorized as "Delayed" (yellow).
Immediate Life-Saving Interventions (LSIs): While primarily a rapid assessment and sorting tool, START permits limited, critical interventions at the point of initial assessment. These include opening the airway and applying tourniquets for uncontrolled extremity bleeding, after which the responder must move on to the next patient.
Patient Categories (Color-coded): Patients are assigned to one of four color-coded categories:
Black (Deceased/Expectant): Patients who do not resume breathing after airway repositioning, or those with injuries deemed incompatible with life.
Red (Immediate): Patients with severe, life-threatening injuries who require rapid intervention and transport to survive.
Yellow (Delayed): Patients with serious injuries that are not immediately life-threatening; they can tolerate a delay of 1-3 hours before transport.
Green (Walking Wounded/Minor): Patients with minor injuries who can wait more than 3 hours for transport or may not require it.
Re-triage: The START system emphasizes that patient conditions are dynamic and can worsen over time. Therefore, re-triage is crucial and should occur as additional rescue personnel arrive and as time and resources permit.
Advantages
START triage is widely praised for its speed and simplicity. Its design allows for rapid assessment, typically within 30 seconds per patient, which is crucial in chaotic, high-volume MCI environments. This straightforward approach makes it particularly effective for initial assessment by first responders with basic medical training.
The system's widespread adoption is another significant advantage. It is one of the most commonly used triage methods in the United States and has been utilized by various military forces, including NATO armies. This broad acceptance facilitates interoperability and coordinated response among different agencies during large-scale incidents.
Furthermore, START's ease of training and recall contributes to its rapid deployment capabilities in disaster scenarios. Its simple algorithm can be quickly taught and remembered, enabling a larger number of personnel to participate effectively in the initial triage phase. The system's primary objective is the
prioritization of critical patients, ensuring that those with the most serious, life-threatening injuries are identified quickly for immediate attention, stabilization, and transportation.
Limitations and Criticisms
Despite its advantages, START faces several notable limitations and criticisms. A significant and frequently cited issue is its propensity for over-triage. This occurs when patients with less critical injuries are categorized as needing immediate attention. Often, non-acute factors such as emotional or psychological reactions to the incident can cause physiological responses like tachypnea (respiratory rate >30 per minute), leading to an "Immediate" (red) tag even if the underlying injury is not immediately life-threatening. While some degree of over-triage is considered acceptable to avoid missing serious conditions, excessive over-triage can lead to inefficient allocation and waste of limited resources, potentially diverting them from truly critical patients.
The respiratory rate thresholds in the START algorithm also draw criticism. It defines only an upper limit (respiratory rate >30 per minute) for critical conditions, failing to account for bradypnea (respiratory rate <10 per minute), which is also a life-threatening situation indicative of hypoxemia and should warrant an "Immediate" tag. Furthermore, the algorithm does not consider the depth of respiration, which is an essential measure of breathing quality. This narrow focus on rate alone can lead to misclassification.
Another limitation is the lack of a direct trauma severity index. START primarily relies on basic physiological parameters (RPM) and does not incorporate a comprehensive assessment of the severity of specific traumatic injuries. This can make it difficult to prioritize among multiple patients who have all been tagged "red" but may have vastly different injury severities, potentially delaying definitive care for the most severely injured within that category.
Environmental factors can also affect the accuracy of perfusion assessment. While modifications have been made to START (e.g., substituting radial pulse for capillary refill), environmental conditions like cold temperatures can still impact the reliability of perfusion checks.
A pervasive concern across disaster triage literature is the limited real-world validation of START. Despite its widespread use, there is a surprising lack of rigorous scientific review or comprehensive outcomes assessment from actual disaster scenarios to fully support its classification accuracy and effectiveness. Much of the supporting evidence is derived from simulated tests rather than real-world incidents.
Finally, START is considered a static system in that it is not explicitly designed to directly incorporate resource limitations or dynamic changes in patient condition or available resources into its core algorithm. This can be a significant drawback in evolving MCI situations where resource availability and patient needs are constantly changing.
The inherent simplicity of START, while a primary advantage for speed and rapid deployment, directly contributes to these limitations. The reliance on broad physiological thresholds without accounting for nuances like respiratory depth or lower rate limits can lead to misclassification of patients who are physiologically reactive but not critically injured. Moreover, the absence of a trauma severity index means that while START effectively identifies patients requiring immediate attention, it does not provide a mechanism to prioritize among those "immediate" patients. This creates a fundamental tension in MCI triage: the trade-off between the imperative for extremely rapid assessment in chaotic environments and the desire for precise and nuanced patient categorization that optimizes resource allocation.
Sort-Assess-Lifesaving Interventions-Treatment/Transport (SALT)
Core Principles and Protocol
SALT (Sort-Assess-Lifesaving Interventions-Treatment/Transport) represents a significant evolution in mass casualty triage, developed by a CDC-sponsored working group to propose a standardized, all-hazards initial triage method. This system is designed for applicability across all patient populations, including adults, children, and individuals with special needs. SALT incorporates best practices from existing triage systems, building upon the available scientific evidence and consensus opinion from a broad panel of experts. Its robust development has led to endorsements from prominent professional organizations, including the American College of Emergency Physicians (ACEP), the American College of Surgeons Committee on Trauma (ACSCOT), and the National Association of EMS Physicians (NAEMSP).
Detailed Steps of the Algorithm
The SALT algorithm is structured in distinct, sequential steps to guide responders through the triage process:
STEP 1: Sort (Global Sorting): SALT begins with a rapid, global sorting of patients into initial manageable groups, which then dictates the priority for individual assessment. This initial sorting phase involves:
Priority 1: Still/Obvious Life Threat: Individuals who are not moving or exhibit clear, immediate life-threatening conditions (e.g., severe uncontrolled bleeding, obvious respiratory distress) are identified first and prioritized for immediate individual assessment.
Priority 2: Wave/Purposeful Movement: Patients who are unable to walk but can follow a simple command (e.g., "wave your hand") or demonstrate other purposeful movement are assessed second.
Priority 3: Walk: Patients who are able to ambulate to a designated safe area are assigned the lowest priority for individual assessment. These "walking wounded" can also be engaged to assist in the initial sorting and care of other patients, leveraging available human resources.
STEP 2: Assess (Individual Assessment) and Life-Saving Interventions (LSIs): The individual assessment phase is unique in SALT for its immediate integration of limited, rapid life-saving interventions. These interventions are performed only within the responder's scope of practice and if the necessary equipment is immediately available. Key LSIs include:
Control Major Hemorrhage: This is a critical distinction from other systems, as SALT prioritizes the application of tourniquets or direct pressure to control significant bleeding early in the assessment process. This addresses the leading preventable cause of death in trauma, which can occur within minutes.
Open Airway: Through simple positioning (e.g., head tilt/chin lift) or basic airway adjuncts. Advanced airway devices are not used at this initial stage. For pediatric patients, considering two rescue breaths is an important part of this step.
Chest Decompression: For tension pneumothorax.
Auto-injector Antidotes: For specific chemical or biological exposures.
Categorization for Treatment/Transport: After assessment and the performance of LSIs, patients are assigned to one of five categories, typically indicated by color-coded tags :
Black (Dead): Patients who are not breathing even after life-saving interventions have been attempted.
Gray (Expectant): This is a defining and ethically significant category in SALT. It is designated for patients who are still breathing but are deemed unlikely to survive given the currently available resources. This category is explicitly resource-based, allowing providers to ethically focus limited resources on potentially salvageable patients with a higher probability of survival.
Red (Immediate): Patients who do not obey commands, lack a peripheral pulse, are in respiratory distress, or have uncontrolled major hemorrhage.
Yellow (Delayed): Patients with serious injuries that are not immediately life-threatening but require definitive care; they can tolerate a delay in treatment without increasing their risk of mortality.
Green (Minimal): Patients with mild, self-limited injuries who can tolerate a significant delay in care without increased mortality risk.
Dynamic Prioritization and Reassessment: SALT emphasizes that the prioritization process is dynamic and adaptable. It can be altered by changing patient conditions, the availability of resources, and evolving scene safety. Reassessment of all patient categories is crucial and should occur as soon as possible when higher-trained responders or additional resources arrive, recognizing that patient status can improve or decompensate over time.
Advantages
SALT's primary strength lies in its standardized and comprehensive approach, aiming to unify triage practices across the United States. This standardization is crucial for effective multi-agency responses, ensuring consistent patient categorization regardless of jurisdiction. Its design as an "all-hazards" system, applicable to diverse patient populations including adults, children, and those with special needs, further enhances its versatility in various MCI scenarios.
A significant improvement over earlier systems is the early integration of limited rapid life-saving interventions (LSIs) directly into the assessment phase. This direct action, particularly for hemorrhage control, addresses immediate life threats that can cause death in minutes, a critical advancement over protocols that might delay such interventions until after initial sorting. This demonstrates a shift towards immediate point-of-injury care, which can dramatically impact patient outcomes.
The inclusion of a resource-based expectant category (Gray) is a key differentiator for SALT. This category explicitly accounts for the grim reality of resource scarcity in overwhelming MCIs, allowing providers to ethically and practically allocate limited resources by focusing on patients with a higher probability of survival. This reflects a profound ethical consideration, shifting the focus from individual beneficence to the utilitarian principle of achieving the greatest good for the greatest number. This decision, while challenging for providers, provides a structured framework for managing resource-constrained environments. It also underscores the dynamic nature of MCI response, as expectant patients may receive care if resources later become available, emphasizing that the "expectant" status is conditional on resource availability.
Furthermore, studies indicate that SALT generally achieves higher accuracy rates and lower undertriage rates compared to START, particularly in classifying "delayed" and "immediate" patients. Modifications to the SALT system have shown further reductions in triage errors, improving its diagnostic power. Its design also promotes consistency with traditional medical care principles, which can enhance its acceptance and application by a wider range of medical professionals.
Limitations and Criticisms
Despite its advancements, SALT is not without its limitations. One concern is its perceived complexity compared to the simpler START system. While designed to be straightforward, its more detailed assessment steps and additional categories may lead some responders to find it more challenging to learn and apply, especially under high-stress conditions.
Similar to START, SALT utilizes color-coded categories, which are criticized for not always accurately reflecting survival probability or providing strong predictive validity. This can result in a wide range of patient acuities being grouped under a single color (e.g., "red"), potentially leading to subjective and inconsistent prioritization
within those categories. This broad categorization can hinder precise resource allocation at later stages of care.
The subjectivity in differentiating certain categories, such as "green" (minimal) from "yellow" (delayed), has also been noted as a potential issue, which may contribute to undertriage in some instances. This highlights the ongoing challenge of creating objective criteria for nuanced patient conditions in a rapid assessment environment.
Another criticism is that, like START, SALT does not explicitly incorporate patient deterioration over time into its core algorithm, implicitly assuming a static condition once triaged. While re-triage is emphasized, the initial classification doesn't inherently account for the progressive nature of certain injuries.
Similar to other triage systems, robust real-world validation data for SALT remains limited. Much of the supporting evidence is derived from simulations rather than actual incidents, making it difficult to definitively assess its performance in the unpredictable and complex environment of a true MCI.
Finally, while improving undertriage, some studies indicate that SALT may result in higher overtriage rates compared to START. This could still lead to the consumption of limited medical resources by less critical patients, impacting overall efficiency.
The integration of early life-saving interventions (LSIs) in SALT, while critical for patient outcomes, introduces a subtle but important trade-off: it inherently adds a slight increase in assessment time per patient compared to the purely rapid assessment of START. This means that while SALT aims for more comprehensive initial care, the operational challenge lies in performing these vital LSIs quickly and efficiently without significantly compromising the overall flow and speed of triage in a high-volume MCI. This balance between immediate intervention and overall triage throughput is a key consideration for responders.
Rapid Assessment of Mental Status and Pulse (RAMP)
Core Principles and Protocol
RAMP (Rapid Assessment of Mental Status and Pulse) is a triage system specifically designed for extremely rapid assessment in mass casualty incidents, particularly recommended when the number of immediate patients significantly exceeds available resources. It simplifies patient categorization into typically three broad groups: Expectant/Deceased, Urgent, and Delayed. The core of RAMP's assessment relies on just two primary physiological indicators: the patient's Mentation (specifically, their ability to follow simple commands) and the presence of a palpable Radial Pulse. These indicators are chosen due to their strong scientific correlation with patient survival, with studies showing that the ability to follow basic commands is a key predictor of trauma survival, and an absent radial pulse correlates with significantly higher mortality.
Detailed Steps of the Algorithm (Inferred from principles and examples)
While the provided research material does not contain a comprehensive, explicit flow chart for the medical RAMP algorithm , its operational logic can be inferred from the stated principles and illustrative examples:
Primary Assessment: Responders rapidly assess two key parameters for each patient:
Mentation: The primary question is whether the patient can follow simple commands. The ability to follow basic commands is considered the best overall indicator of survival from trauma.
Pulse: The second assessment is the presence of a palpable radial pulse. The absence of a radial pulse is associated with a significantly higher mortality rate.
Categorization: Based on these two rapid assessments, patients are categorized into one of three groups:
Expectant/Deceased (Black): If the patient is not following commands AND has no palpable radial pulse. This combination is strongly associated with a very high mortality rate (92%).
Urgent (Red): If the patient is not following commands BUT does have a palpable radial pulse.
Delayed (Green): If the patient is following commands AND does have a palpable radial pulse. This combination is associated with a high survival rate (95%).
Note on "Yellow" Category: Some RAMP models explicitly exclude the "yellow" (delayed) category, citing it as the most inaccurately triaged category by EMS providers. However, other sources indicate "Delayed" as a RAMP category, often color-coded green. This suggests some variation in RAMP implementation or interpretation across different agencies.
Life-Saving Interventions: RAMP protocols instruct responders to provide life-saving emergency medical care as needed, such as placing tourniquets, during the triage process.
Reporting: Once triage is complete, the Triage Sector Officer provides a "Triage Report" to Command. This report includes the number of immediate and delayed patients, along with other pertinent information such as pediatric/adult status, burns, or chemical exposure.
Advantages
RAMP's most compelling advantage is its extreme simplicity and speed. By focusing on just two critical physiological parameters (mentation and pulse), it is designed for maximum ease of use, recall, and rapid application, even under significant stress and in highly chaotic environments. This minimalist approach eliminates reliance on complex numbers or extensive critical thinking, making it highly accessible for first responders.
This simplicity facilitates the rapid identification of the most severely wounded. By quickly assessing mentation and pulse, RAMP allows for very swift identification of patients at high risk of mortality, enabling immediate resource allocation to those most critical.
RAMP also benefits from a strong scientific evidence base for its core indicators. The chosen physiological parameters (Glasgow Coma Scale/mentation and radial pulse) are well-established as correlating strongly with patient survival and hospital discharge in trauma, providing a robust foundation for its criteria.
Its simplified nature makes it potentially more suitable for high-threat, dynamic, or resource-limited environments where rapid, decisive actions are paramount and prolonged assessment is not feasible.
Limitations and Criticisms
The primary limitation of RAMP stems from its very simplicity: limited categorization. The reduction to typically three categories (Expectant/Deceased, Urgent, Delayed) can oversimplify patient acuity, potentially grouping patients with significantly different needs or prognoses into the same category. This lack of granularity might hinder more nuanced resource allocation at later stages of care.
Studies suggest that RAMP may exhibit lower sensitivity in identifying Priority 1 patients (those requiring time-critical, life-saving interventions) compared to some more detailed triage tools. One comparative analysis reported RAMP's sensitivity as 43.8%. This indicates a substantial risk of undertriage, where patients who genuinely require urgent life-saving interventions are not accurately identified as such.
Despite its simplified approach, RAMP can still lead to high overtriage rates (e.g., 26.8% in one study). This can result in the unnecessary consumption of limited medical resources by less critical patients, impacting overall efficiency.
The explicit exclusion of a "yellow" (intermediate delayed) category in some RAMP models, while aiming to reduce mis-triage in that specific category, might remove a useful intermediate classification that could facilitate more nuanced resource allocation and patient flow management in certain MCI scenarios.
A practical limitation, based on the provided material, is the absence of a comprehensive, explicit flow chart or detailed step-by-step algorithm for the medical RAMP triage system. This makes a full, detailed analysis of its internal decision-making process challenging without further external information.
The extreme simplification inherent in RAMP, while enabling remarkable speed and ease of use, carries an inherent trade-off: it sacrifices diagnostic granularity. By reducing the number of assessment points and triage categories, RAMP runs a higher statistical risk of undertriage. This means that some patients who, while not immediately "red," still require urgent attention that a more detailed assessment might reveal, could be misclassified. This highlights a strategic decision in triage system design: to prioritize rapid decision-making and ease of application in highly chaotic or resource-depleted environments, even if it means accepting a higher statistical risk of misclassification compared to more complex systems.
Comparative Analysis of START, SALT, and RAMP
The choice of triage system in a mass casualty incident is a critical decision, influencing patient outcomes and resource allocation. While START, SALT, and RAMP all aim to sort patients effectively, they differ significantly in their methodology, complexity, and performance characteristics.
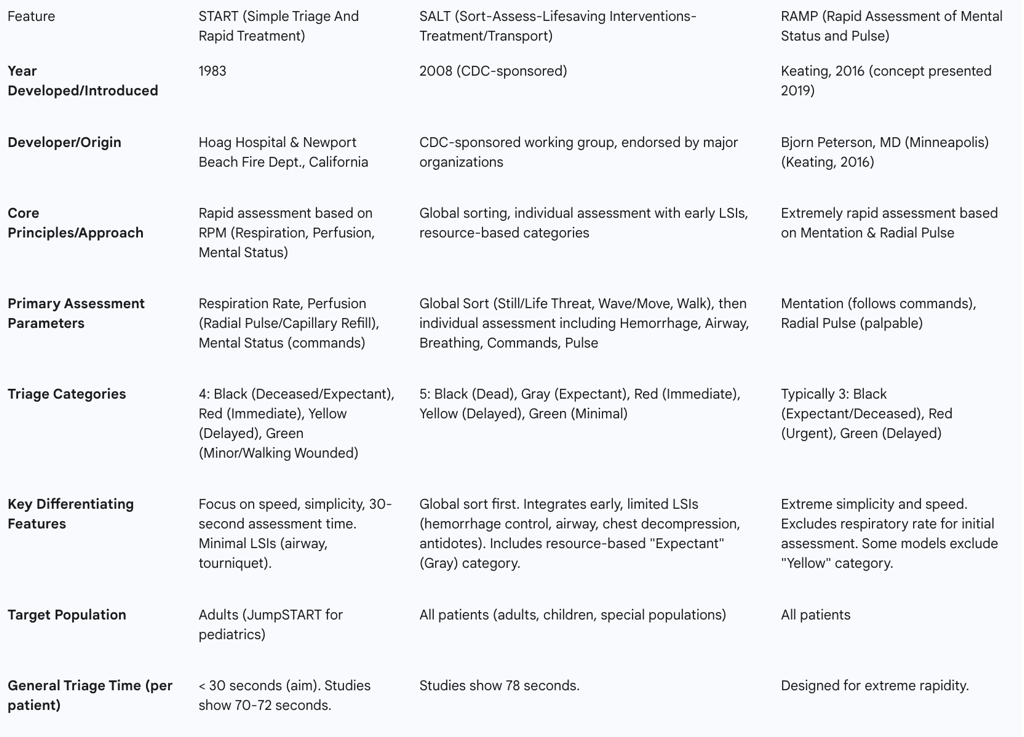
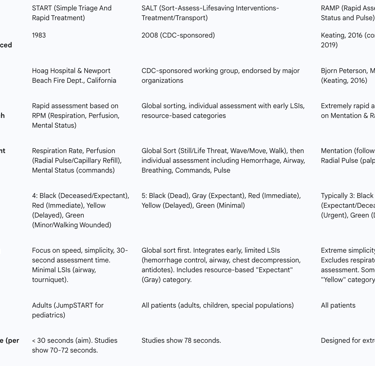
Table 1: Comparative Overview of START, SALT, and RAMP Triage Systems
Discussion of Comparative Performance
Quantitative analysis comparing these triage systems in real-world mass casualty incidents is limited, with much of the evidence derived from simulated scenarios. However, available studies offer valuable insights into their relative performance.
Accuracy and Misclassification: SALT generally demonstrates higher accuracy rates and lower undertriage rates compared to START. For instance, one study found SALT to have a 52% accuracy rate compared to START's 36% in an emergency department setting, and SALT had a significantly lower undertriage rate (26% vs. 57%). Another systematic review reported SALT's accuracy between 70% and 83%, while START's ranged widely from 44% to 94.2%. This suggests SALT provides more consistent and reliable categorization. However, SALT may also exhibit higher overtriage rates in some studies compared to START. RAMP, while designed for speed, has shown lower sensitivity in identifying Priority 1 patients (43.8%) and higher undertriage rates (56.2%) compared to some other tools in pediatric populations, indicating a risk of missing critical patients.
Speed and Simplicity: START is widely praised for its simplicity and rapid application, aiming for 30 seconds per patient. A systematic review found START to be faster (70-72 seconds per patient) than SALT (78 seconds per patient). RAMP is designed for even greater speed and ease of use, relying on just two parameters to eliminate complex decision-making under stress. This makes START and RAMP particularly advantageous in the initial, chaotic phases of an MCI where speed is paramount.
Life-Saving Interventions: A key distinction lies in the integration of immediate life-saving interventions (LSIs). START permits minimal LSIs like airway opening and tourniquet application. SALT, however, explicitly integrates a broader range of rapid LSIs, including hemorrhage control, airway management (with rescue breaths for children), chest decompression, and auto-injector antidotes, directly into the assessment phase. This proactive approach to immediate life threats is a significant advancement for SALT, addressing conditions that can be fatal within minutes. RAMP also allows for LSIs like tourniquet placement.
Categorization and Resource Allocation: START uses four categories, while SALT introduces a fifth, "Gray" (Expectant), which is explicitly resource-based. This "Expectant" category allows for ethical resource allocation when demand far exceeds supply, focusing efforts on salvageable patients. RAMP simplifies further, typically using only three categories, and some versions omit the "Yellow" (Delayed) category to reduce mis-triage, though this can also reduce granularity in patient classification. The static nature of START's categories, which do not inherently account for dynamic changes in patient condition or resource availability, is a recognized limitation. SALT's framework, conversely, emphasizes dynamic prioritization based on evolving conditions and resources.
Training and Implementation: START is known for its ease of training and widespread adoption, making it a common choice for initial responder training. SALT is perceived by some as more challenging to learn than START due to its increased complexity, though studies suggest healthcare students often prefer SALT for its logic and comprehensibility. RAMP is lauded for its extreme simplicity and ease of recall, making it highly teachable for rapid deployment.
Conclusions
The analysis of START, SALT, and RAMP triage methodologies in mass casualty events reveals that no single system is universally superior; each presents a unique balance of speed, accuracy, and comprehensiveness.
START excels in its simplicity and speed, making it an invaluable tool for initial, rapid assessment by first responders in chaotic environments. Its ease of training and widespread adoption facilitate broad application. However, its reliance on broad physiological thresholds can lead to significant over-triage, potentially misallocating limited resources. Furthermore, its lack of granularity in assessing trauma severity and its static nature can be drawbacks in evolving MCI scenarios.
SALT represents a more comprehensive and standardized approach, integrating crucial early life-saving interventions directly into the assessment process. The inclusion of a resource-based "Expectant" category is a significant ethical and practical advancement, enabling more judicious resource allocation in overwhelmed situations. Studies suggest SALT generally offers higher accuracy and lower undertriage rates than START. However, its increased complexity may pose a greater training burden compared to START.
RAMP prioritizes extreme speed and simplicity, focusing on just two highly predictive physiological parameters: mentation and radial pulse. This design makes it exceptionally easy to learn and apply, particularly in high-threat or severely resource-constrained environments. The trade-off for this extreme simplification, however, is a reduction in diagnostic granularity, which can lead to higher rates of undertriage and overtriage compared to more detailed systems.
The ongoing challenge in MCI triage lies in the fundamental tension between the need for extremely rapid decision-making in the initial chaotic phase and the desire for precise and nuanced patient categorization that optimizes resource allocation and long-term outcomes. While military experiences inform civilian protocols, the direct transferability and confirmed efficacy of these systems in civilian contexts remain areas requiring further rigorous, real-world validation. Future advancements in MCI triage will likely involve continued refinement of existing protocols, potentially incorporating technology-assisted assessments, and a persistent focus on robust training and exercises to enhance responders' ability to apply these critical skills effectively under immense pressure. Ultimately, the most effective triage strategy may involve a flexible, adaptive approach, utilizing the simplest, fastest methods for initial sorting, followed by more refined, intervention-focused assessments as resources become available and the scene stabilizes.
