The Spanish Triage Model (MAT): Its History, Methodology, and Role in Modern Emergency Care
The MAT is a structured, five-level prioritization model, a format it shares with other widely adopted international systems. The system's central feature is its integration into a computer-assisted program, the PAT, which guides the professional through the classification process.


The concept of triage, derived from the French word trier—meaning "to sort" or "to classify"—has evolved from its military origins into a fundamental component of modern healthcare systems. While the term originally described the sorting of agricultural products, its application in medicine is now almost exclusive to contexts involving the allocation of scarce resources. The historical practice of triage arose from the necessities of warfare, with early, documented systems dating back to the 18th century. Most scholars attribute the first formal battlefield triage system to Baron Dominique-Jean Larrey, chief surgeon of Napoleon's Imperial Army. Larrey's system represented a radical departure from previous practices, which often involved waiting until a battle concluded to treat the wounded. Instead, his "flying ambulances" were designed to rapidly transport and treat soldiers based on the urgency of their wounds, an early form of patient prioritization.
This military principle of sorting casualties based on need stands in stark contrast to the "first come, first served" method that was prevalent in early civilian and military medical settings, as described by poet Walt Whitman during the American Civil War. Whitman's observations of wounded soldiers waiting patiently for their turn highlighted a system that did not account for the severity of injuries, a fundamental flaw that modern triage was developed to correct.
Today, triage is a critical clinical and administrative process for safely managing patient flow in emergency departments (EDs), especially when patient demand exceeds available resources. The primary objectives of a structured triage system are to identify patients with life-threatening conditions quickly and to classify them according to a priority level. The system is designed not only to prioritize care but also to determine the most appropriate treatment area, mitigate congestion, and provide a framework for continuous patient re-evaluation. By providing a uniform and structured approach, modern triage systems aim to reduce the variability in clinical decision-making and provide a predictable, auditable process for managing a fundamentally chaotic environment.
1.2 The Canadian Influence: The MAT’s Conceptual Lineage
The Modelo Andorrano de Triaje (MAT) is not an isolated development but rather a direct "conceptual adaptation" of the Canadian Emergency Department Triage and Acuity Scale (CTAS). This lineage is crucial as it grounds the MAT in an internationally recognized, evidence-based framework that has been a national standard in Canada since 2002. The MAT was developed by Josep Gómez Jiménez and a commission from the Andorran Health Service in 2000, with its origins tracing back to the Australian-Canadian school of triage.
A pivotal element of the MAT's design was the integration of a computerized decision-support tool known as the Programa de Ayuda al Triaje (PAT). This decision was driven by the recognition that the highly structured nature of the original CTAS presented a significant challenge for creating an electronic version. By building the system from the ground up to be digitally native, the MAT became more than just a clinical protocol; it was conceived as a comprehensive socio-technical system. The software is not an optional accessory but the central mechanism for the system's function, guiding professional decision-making and ensuring consistency.
A key, non-clinical driver for the MAT's success was its ability to provide professional support. Multiple sources highlight that one of the PAT's primary objectives is to provide a "protocolized medico-legal support element" for healthcare professionals, particularly nurses. Historically, concerns about legal liability were a significant barrier to nurses performing triage. The formalization of the process through a validated, computer-assisted protocol served to mitigate this risk, making the practice more acceptable to the nursing profession. The importance of this legal formalization is underscored by a firm court ruling in Spain in February 2007, which affirmed the nursing role in structured triage using the SET. This transformation of triage from a clinical task to a legally supported professional practice was a critical factor in its widespread adoption.
The Modelo Andorrano de Triaje (MAT): Core Methodology and Structure
2.1 Architectural Framework: The PAT System
The MAT is a structured, five-level prioritization model, a format it shares with other widely adopted international systems such as the Australian Triage Scale (ATS), the CTAS, the Manchester Triage System (MTS), and the Emergency Severity Index (ESI). The system's central feature is its integration into a computer-assisted program, the PAT, which guides the professional through the classification process. The software is designed to integrate with hospital electronic health records, enabling a seamless flow of information. The PAT program is not a simple checklist; it uses a complex algorithmic approach based on a series of questions that, when answered, yield a final triage level.
2.2 Building Blocks of Classification: A Multi-Factorial Approach
The MAT’s methodology is symptom-based, rather than diagnosis-based, which allows for initial classification without a definitive medical diagnosis. The original PAT v3 recognized 32 symptomatic categories and 14 subcategories, which encompassed 578 distinct clinical reasons for consultation. This extensive list provides a high degree of granularity for patient classification, which has since been expanded to include 617 reasons in later versions.
The system uses specific "discriminants" to differentiate the degree of urgency between triage levels within the same symptomatic category. These discriminants include:
Vital Signs: Objective physiological measurements such as temperature, systolic blood pressure, heart rate, oxygen saturation (SpO2), capillary glycemia, and the Glasgow Coma Scale. These are used to differentiate patients with similar symptoms, for example, between Level II and Level III.
Abnormal Vital Signs: A qualitative assessment of a patient's condition, including skin condition, radial pulse, respiratory rate and depth, and the presence of drowsiness or confusion.
Pain Assessment: The MAT includes a dedicated clinical guide to objectify the patient's self-reported pain levels. This allows the professional to incorporate pain as a measurable discriminant for classification.
The system also integrates various, pre-existing, validated severity scales, such as the Glasgow Coma Scale, and scales for non-traumatic coma, dehydration, clinical dyspnea, or asthma. The computerization of the model makes these tools readily available to the professional during the triage process.
The design of the MAT extends beyond pure clinical classification to serve a dual function. The system's objectives include providing information for hospital management to "optimize resources and improve management". The collection of a "minimum set of emergency care data (CMBDU)" is used for "benchmarking" and to analyze the patient "casuística" or "case-mix". This allows administrators to move from anecdotal observations to data-driven analysis for resource allocation and demonstrating efficiency, positioning the MAT as a powerful administrative tool in addition to a clinical one.
2.3 Triage Levels, Colors, and Timeframes: A Nuanced and Critical Analysis
The five-level structure of the SET-MAT provides a clear framework for patient prioritization, but a review of the literature reveals a notable lack of uniformity in the specific colors and timeframes associated with each level. This variability is not necessarily an error but a reflection of the system's dynamic evolution and its adaptation to different regional and institutional contexts.
The following table provides a consolidated view of the most commonly cited data, while also explicitly addressing the discrepancies found in the research material.

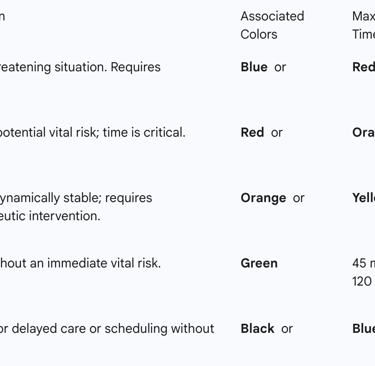
The variations in these standards are a critical observation. While a standardized model is meant to provide a universal language for triage, the observed discrepancies in colors and wait times suggest that the system is not static. Instead, it appears to be a dynamic framework that has been adapted by different health systems or evolved through subsequent software versions (e.g., PAT v4) to better align with local resources, patient demographics, and clinical preferences. This flexibility, while potentially compromising absolute standardization, may be a necessary component of its widespread adoption in a decentralized healthcare system like Spain's.
The Spanish Adaptation: From MAT to the Sistema Español de Triaje (SET)
3.1 Institutionalization and Professional Standards
The official adoption of the MAT as the national standard for triage in Spain, known as the Sistema Español de Triaje (SET), was orchestrated by the Sociedad Española de Medicina de Urgencias y Emergencias (SEMES) in 2003. This institutional endorsement provided a critical foundation for its dissemination and acceptance across the country.
To ensure the system's effectiveness and safety, SEMES has established specific requirements for professionals, primarily nurses, who perform triage. These requirements mandate that individuals have specific training in emergencies and critical patients, as well as dedicated theoretical and practical training in the SET model itself. Additionally, professionals are required to have a minimum of one year of experience in a hospital emergency department and at least six months of experience in the specific hospital where they will perform triage to ensure familiarity with local protocols and care circuits. These stringent requirements demonstrate that the system's efficacy is contingent upon a highly skilled and well-prepared workforce, highlighting the interdependence of the clinical protocol and the professionals who use it.
3.2 Regional Implementation: A Gradual Process
The implementation of the SET in various autonomous communities in Spain began in 2003 and has been described as a "gradual process". A key case study on the implementation of the SET in 29 public hospitals in Andalusia provides a clear illustration of this multi-phase process. Over the course of three semesters, the study found a progressive increase in SET usage.
This phased implementation underscores that the adoption of a new triage system is not merely a technical or administrative switch but a complex socio-technical challenge. The process requires an "adaptation period for professionals" to avoid a negative impact on quality indicators. The success of the implementation is dependent on the seamless integration of a well-trained workforce, a supportive institutional environment, and a robust IT infrastructure that can handle the triage software and its data. The "gradual process" is therefore not a flaw but a necessary period of adaptation for both the system and the people who use it.
Clinical Performance and Validation of the SET
4.1 Scientific Validation: Reliability and Validity
The SET-MAT has undergone rigorous clinical validation, demonstrating high reliability and a strong correlation between its assigned priority levels and patient outcomes. A key measure of a system's safety and reproducibility is its interobserver concordance—the degree to which different professionals classify the same patient at the same level. A clinical study on the web_e-PAT v3 version of the software found a weighted kappa (k) index of 0.90, indicating excellent reliability and agreement. The exact modal concordance was 93%, with agreement within one triage level reaching 99%. This high degree of consistency confirms that the SET is a valid, useful, and reproducible tool for clinical practice.
The system's validity has also been confirmed by its ability to correlate the assigned triage level with patient outcomes, which are used as "surrogates for severity". A study on neonates, for instance, found a positive correlation between higher priority levels and an increased need for hospital admission and resource consumption.
4.2 Impact on Key Performance Indicators
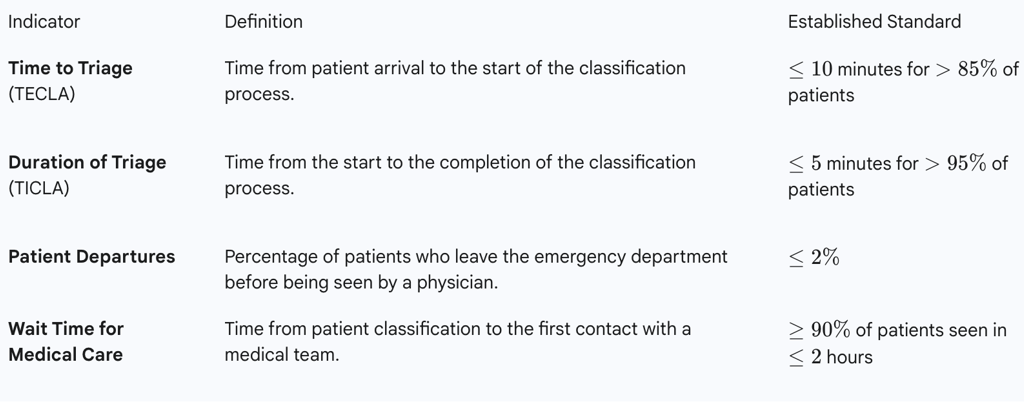
The implementation of the SET has been shown to positively impact key administrative and clinical performance indicators, reflecting its dual purpose as a clinical and managerial tool. The system aims to improve patient flow and reduce congestion. A study on its implementation in Andalusia found a significant decrease in the mean wait time before triage (TECLA), and a corresponding increase in the proportion of patients who waited less than 10 minutes. The SET sets a standard that over 85% of patients should be triaged within 10 minutes of arrival, with the classification itself taking less than 5 minutes for over 95% of patients.
The study on the Andalusian implementation also provides a nuanced view of the system's impact. While it noted a statistically significant increase in the proportion of patients who left before being seen, the authors concluded that the clinical impact was minimal due to the small magnitude of the change. Furthermore, the ED mortality rate did not change significantly during the implementation period, indirectly confirming that the system did not negatively impact patient safety. This demonstrates the importance of a multi-metric approach to evaluating a system's performance, as a single, negative statistic might not reflect the overall positive impact on core outcomes.
The SET also provides a framework for financial and managerial accountability. It allows for the analysis of patient "case-mix" and complexity based on their final destination (e.g., admission, discharge) and age. The ability to collect and analyze this data enables hospital administrators to conduct benchmarking, optimize resource allocation, and improve management decisions, thereby linking clinical practice directly to administrative oversight.
Table 2: Key Quality Indicators for SET Performance
A Comparative Perspective: SET vs. Manchester Triage System (MTS)
5.1 Methodological Differences
The triage landscape in Spain is a dynamic one, with two dominant systems co-existing: the SET and the Manchester Triage System (MTS). While both are five-level priority systems, their underlying methodologies differ significantly.
The SET, rooted in the MAT, is a symptom-based model that relies on a computerized application (e-PAT) to guide the professional through a series of questions. It uses an extensive list of 32 symptomatic categories and various discriminants and severity scales to reach a classification. This multi-factor approach allows for a granular and nuanced patient assessment.
In contrast, the Manchester Triage System, developed in the UK in 1994, is a flowchart-driven model based on 52 clinical presentations. The professional follows a series of "yes/no" questions (discriminators) to navigate a flowchart and arrive at a priority level. The methodological divergence between these two systems is a critical distinction. A study comparing different triage methods for mass casualty incidents found differences in how each system classified patients by severity, suggesting that the chosen methodology can have a direct impact on the identification of the most critically ill patients.
5.2 Implementation Landscape and Regional Distribution
The SET and MTS are the two most widely established triage systems in Spanish hospitals. The MTS is used in autonomous communities such as Asturias, Madrid, Galicia, Andalusia, Extremadura, and the Valencian Community, and in at least 78 hospitals across Spain. The SET, having been officially endorsed by SEMES, is used in the remaining communities and in over half of the hospitals surveyed by the Sociedad Española de Urgencias de Pediatría (SEUP).
The co-existence of these two systems highlights a decentralized, "best-fit" model of adoption in Spain, where regions or hospitals select or adapt a system based on their specific needs, resources, and historical preferences. An example of this is the hospital network in Navarra, which has a system adapted from both the SET and the MTS. This approach, while fostering local control and flexibility, may also present challenges in achieving national-level data standardization and comparability.
Challenges, Criticisms, and Areas for Improvement
6.1 Implementation Hurdles and Professional Adaptation
The implementation of any structured triage system, including the SET, is a complex process with inherent challenges. The research repeatedly emphasizes the need for a gradual implementation and an "adaptation period" for professionals. While the SET provides a structured protocol, its effective application requires significant professional training and experience. A lack of specific training can lead to a lack of professional confidence and an inability to handle the complex psychological aspects of patient interaction. The system also faces the challenge of patient resistance, as many patients may expect fast, simple solutions and are unprepared for the comprehensive, multi-dimensional approach of structured triage.
6.2 Systemic Discrepancies and Inconsistencies
Despite the SET's goal of standardization, the literature reveals inconsistencies, particularly regarding the specific timeframes and colors associated with each triage level. While these variations may be due to regional adaptations or software updates, they can undermine the system's intended function as a universal, uniform protocol across all of Spain.
A further challenge is the lack of universal access to the triage software itself. A survey of Spanish hospitals found that a significant percentage of those using a triage system did not have a dedicated software application. Since the SET's core benefits—such as medico-legal support for nurses, robust data collection, and decision support—are tied to its digital nature, the absence of this software compromises the system's full potential. The broader digital transformation landscape in Spain provides a useful analogy; as seen in other digital initiatives, the implementation of new technology is often fraught with issues such as a lack of transparency, low-quality services, and inadequate support, which can hinder even a well-designed system.
The Future of the SET: Innovation and Strategic Trajectory
7.1 European and International Recognition
A significant strategic development for the SET occurred in May 2025, when it was registered as a European trademark by the European Union Intellectual Property Office (EUIPO). This formal legal protection is a critical step that reinforces the authorship and commercial rights surrounding the model. The trademark covers not only the software but also associated printed materials, educational services, and medical services. This elevates the SET from a clinical protocol to a formal piece of intellectual property with significant commercial value. This strategic move positions the SET for further international expansion beyond Spain and its existing presence in Latin America.
7.2 The Role of Technology: From Software to AI
The SET is built on a foundation of continuous improvement, with a modular, multi-platform, and multi-language design that facilitates easy updates and integration. The future of triage is likely to be shaped by advancements in technology, and the SET's digital-first design makes it well-suited for this evolution. The potential for AI to act as a "democratizing tool" in healthcare, enabling professionals to utilize complex systems without becoming experts, is a concept that is directly applicable to triage. AI-powered agents could potentially perform routine triage tasks, freeing up human professionals to focus on more complex cases. Research has also explored the use of computational models and simulations for crisis management and disaster response, a domain where dynamic triage and resource allocation are paramount.
Conclusion and Strategic Recommendations
The Sistema Español de Triaje (SET), a sophisticated adaptation of the Canadian Triage and Acuity Scale (CTAS), has established itself as a cornerstone of emergency medicine in Spain. Its strength lies in its meticulous, software-driven methodology, which provides a data-rich framework for patient classification. The system has been clinically validated, demonstrating a high degree of reliability and a positive impact on key performance indicators such as patient wait times and flow dynamics. Its ability to serve as a tool for administrative oversight, patient case-mix analysis, and medico-legal protection for professionals further solidifies its value.
However, the analysis also reveals that the SET's implementation is a nuanced process. The existence of competing systems like the Manchester Triage System (MTS) and the regional variations in its protocols highlight a "best-fit" approach rather than a truly uniform national standard. The system's full potential is also constrained by logistical hurdles, including the need for continuous professional training and the lack of universal access to its integrated software.
Based on this comprehensive analysis, the following strategic recommendations are proposed:
For Administrators and Policy Makers: A unified national strategy should be pursued to standardize the SET's protocols, including colors and timeframes, to eliminate regional discrepancies. Full investment in the digital integration of the e-PAT software is essential to maximize its benefits for data collection, benchmarking, and medico-legal protection.
For Healthcare Professionals: The importance of standardized and continuous training programs for the SET cannot be overstated. Addressing the confidence gaps reported by professionals will ensure high interobserver concordance and a safe, efficient triage process.
For Innovators and Researchers: Further research and development should focus on leveraging emerging technologies. The integration of AI-powered agents and simulation models into the SET could enhance its efficiency, improve predictive accuracy in patient outcomes, and optimize real-time resource allocation, particularly in high-stakes scenarios like mass casualty incidents or public health crises. The SET's recent formalization as intellectual property positions it for continued innovation and international leadership in the field of structured emergency triage.
