The Power of Remote Triaging in HealthCare
Explore the transformative impact of remote triaging in modern healthcare. Discover how this innovative approach enhances patient care, optimizes resources, and improves healthcare accessibility.


Remote triage, defined as technology-enabled clinical decision-making in the absence of a face-to-face encounter, has emerged as a pivotal component of modern healthcare delivery. Its primary objective is to direct patients to the appropriate level of care, leveraging digital tools and telecommunications for remote assessment and prioritization. This approach offers substantial benefits, including enhanced accessibility to healthcare services, optimized resource allocation within facilities, improved patient convenience, and streamlined clinical workflows.
However, the implementation and scaling of remote triage are not without complexities. Critical considerations encompass ensuring diagnostic accuracy and mitigating misdiagnosis risks, navigating intricate interoperability and data management challenges, addressing the multifaceted needs of staffing, training, and workflow integration, and meticulously handling ethical, legal, and privacy concerns. Patient perception, digital literacy, and managing expectations also present significant hurdles.
Despite these challenges, remote triage holds strategic importance in managing patient flow, alleviating the burden on emergency services, and fostering a more patient-centered, efficient, and resilient healthcare system. The future trajectory of remote triage is poised for transformative advancements, particularly with the increasing integration of artificial intelligence (AI) and predictive analytics, which promise to reshape patient evaluations and care pathways. Realizing the full potential of remote triage necessitates a holistic and integrated approach that strategically harnesses technological innovations while steadfastly prioritizing patient safety, data integrity, and equitable access to care.
Defining Remote Triage in Healthcare
1.1. What is Remote Triage?
Remote triage is formally defined as the process of making clinical decisions and assessing or prioritizing health concerns from a distance, without the necessity of a physical, face-to-face encounter. This innovative approach relies heavily on digital tools and telecommunications to gather essential patient information and subsequently determine the most appropriate level of care required. Essentially, it involves screening patients remotely to ascertain their condition and the necessary medical intervention. The modalities through which remote triage can be delivered are diverse, encompassing traditional telephone-based services, video consultations, web-based platforms, and dedicated mobile applications. This flexibility allows for broad applicability across various healthcare scenarios and patient needs.
1.2. Evolution and Context in Modern Healthcare
Remote clinical triage centers are becoming an increasingly common feature of healthcare delivery, particularly within large healthcare organizations. The widespread adoption and rapid expansion of remote patient care solutions were significantly propelled by the COVID-19 pandemic. This period saw severe resource shortages and a critical need for social distancing, compelling healthcare systems to embrace virtual care as both a standalone solution and in combination with traditional in-person care.
Beyond crisis response, remote triage addresses the evolving needs of a rapidly aging global population, offering a scalable solution to improve access to care, facilitate interprofessional team collaboration, and ensure the appropriate utilization of finite healthcare resources. This evolution signifies a strategic shift in how healthcare services are conceptualized and delivered, moving towards more flexible and accessible models.
1.3. Core Principles and Objectives
The foundational principles guiding remote triage are centered on patient welfare and systemic efficiency. The primary goal is to deliver safe, quality-oriented remote triage, with the health, safety, and well-being of the patient serving as the paramount concern in every interaction. This involves a meticulous process of assessing a patient's current signs and symptoms, concurrently evaluating their past medical history and current medications, and subsequently determining the proper triage disposition. The aim is to direct care to the safest and most cost-effective medical facility available at that specific time. This comprehensive assessment includes understanding the urgency of medical needs and providing appropriate interventions.
An important objective for remote clinical triage centers is to achieve case resolution during the first contact. This means that a telephone call or virtual interaction is managed effectively without requiring further triage for other services, or that the caller is connected with the appropriate individual with only a single transfer. Furthermore, remote triage modalities are designed to significantly improve access to on-demand healthcare, reducing barriers that might otherwise delay or prevent care. A key aim is also to achieve better resource allocation and shorter wait times across the healthcare spectrum.
The initial definitions of remote triage highlight its immediate application in clinical decision-making and enhancing access to care. However, a deeper examination of its role reveals a progression from simply reacting to acute symptoms to proactively guiding patients and preventing more severe conditions. This is evident in the emphasis on engaging patients earlier in their care journey and identifying health risks and exacerbations upstream. This development suggests that remote triage is not merely a logistical tool for managing current demand but a strategic enabler for preventative care and early intervention. By acting as a "digital front door" , it encourages earlier patient engagement, potentially reducing the overall burden of illness and improving long-term population health outcomes.
There exists a subtle yet significant distinction in the concept of "resolution" within remote triage. One perspective suggests that a primary goal is to manage cases without requiring further in-person services. However, a critical question arises: should the ultimate objective be to completely resolve cases remotely, or to accurately determine the most appropriate triage destination for the patient, which may still involve an in-person visit? This underlying tension indicates that the true strength of remote triage lies not necessarily in avoiding in-person care entirely, but in optimizing the pathway to the most suitable care, whether that involves self-care instructions, a scheduled primary care appointment, or an urgent emergency department visit. An overemphasis on strictly avoiding in-person visits could lead to inadequate assessment or patient dissatisfaction if their expectations for care are not met. The genuine value of remote triage, therefore, resides in its capacity for intelligent navigation within the complex healthcare ecosystem.
2. Transformative Benefits of Remote Triaging
Remote triaging has proven to be a transformative force in healthcare, delivering a multitude of benefits that enhance patient experience, optimize operational efficiency, and contribute to improved health outcomes.
2.1. Enhanced Accessibility and Patient Convenience
Remote triaging significantly improves access to healthcare services, particularly for individuals residing in remote or underserved areas, by effectively dismantling geographical barriers. Patients gain the ability to access medical advice and assistance from the comfort of their homes, thereby eliminating the need for travel or enduring prolonged waits in crowded waiting rooms. This inherent convenience and comfort are widely appreciated by patients. Virtual triage (VT) systems specifically enable health systems to extend access to information and services beyond conventional workday and daytime physician office hours, or for situations that would otherwise entail challenging travel logistics. By offering prompt access to medical specialists for preliminary evaluations and actions, remote triage plays a crucial role in reducing patient frustration and delays in receiving necessary care.
2.2. Optimized Resource Allocation and Cost-Efficiency
Remote triage empowers healthcare providers to allocate resources with greater effectiveness by pre-assessing patients before they arrive at a facility. This pre-assessment process helps to reduce the number of unnecessary tests, procedures, and consultations, leading to significant time and resource savings for both patients and healthcare organizations. It contributes to lowering overall healthcare expenditures by minimizing needless emergency room (ER) visits, hospital stays, and in-person consultations. Healthcare providers also benefit from accelerated workflows and reduced administrative costs associated with in-person visits , while patients save money on transportation and time away from work or other obligations.
Remote Patient Monitoring (RPM), a closely related concept, further amplifies cost savings. Hospital at Home (H@H) programs, for instance, have demonstrated a remarkable 30% cost reduction, primarily attributable to decreased overhead and lower readmission rates. RPM has been shown to reduce 30-day hospital readmission rates by up to 83%, preventing costly and often unnecessary hospital stays. Virtual triage can also diminish the need for additional staff, equipment, and resources, thereby lowering operational costs and enhancing overall financial performance for healthcare organizations.
While numerous sources highlight the substantial cost savings, it is important to acknowledge a nuanced perspective from some research. One study found "no difference in overall cost of care" when comparing in-person primary care to GP-led or nurse-led telephone triage. This suggests that the extent of cost-efficiency may vary, potentially being more pronounced in specific contexts such as avoiding high-acuity ED visits or managing chronic diseases through RPM, rather than being a universal outcome across all remote triage modalities.
A common observation is that remote triage leads to "reduced wait times" and "reduces overcrowding". However, several systematic reviews indicate that remote triage has not consistently demonstrated a decrease in primary care or ED utilization, with some studies even reporting a significant increase. This apparent discrepancy suggests that the true strength of remote triage may not lie in reducing the absolute number of patient encounters or visits to traditional facilities, but rather in optimizing the management and flow of these interactions. It ensures that patients are directed to the most appropriate level of care, preventing unnecessary high-acuity visits and improving the efficiency of existing services, even if overall demand remains high or increases due to improved access. The focus thus shifts from simply "fewer visits" to "the right visits, at the right time, in the right place." This also implies that remote triage might increase overall patient engagement with the healthcare system due to lower barriers to entry, leading to more, but potentially lower-acuity, interactions.
The financial advantages of remote triage extend beyond immediate transactional cost reductions. The discussion surrounding RPM introduces concepts like "Hospital at Home" programs and significant reductions in 30-day readmission rates. This indicates that the financial power of remote triage enables systemic shifts in care delivery, such as the move towards home-based care, which can lead to deeper, long-term savings by preventing costly hospitalizations and readmissions. This strategic value proposition is a crucial consideration for healthcare systems contemplating large-scale investments in remote triage solutions.
2.3. Improved Patient Outcomes and Safety
Virtual pre-assessment tools are instrumental in enhancing patient safety by helping to identify individuals who require immediate attention and ensuring resources are assigned accordingly. This proactive approach can prevent medical errors and reduce the risk of adverse outcomes. The timely identification of severe symptoms through remote triage allows for quicker interventions, which directly translates into enhanced health outcomes for patients. Furthermore, by enabling patients to receive medical attention without physically visiting a facility, remote triage significantly decreases the risk of infection transmission, thereby protecting both patients and front-line healthcare staff, a critical benefit particularly during public health crises. Frequent patient data capture facilitated by virtual triage (VT) further supports robust clinical decision-making and holds the potential to reduce medical errors. Remote Patient Monitoring (RPM) interventions are widely recognized for their capacity to improve patient care and overall well-being.
While the benefits are substantial, it is important to consider the nuances regarding patient safety outcomes. A systematic review indicated "no statistically significant differences indicating increased risk for these patient safety outcomes" (mortality, hospitalizations, ED visits). Another review found "low or very low confidence in the evidence that remote triage has no effect on reducing patient deaths". This suggests that while remote triage does not appear to increase risk, direct evidence of its ability to significantly improve mortality rates or reduce adverse events across the board is limited. This implies that remote triage primarily maintains safety standards rather than dramatically enhancing them in all aspects of patient outcomes.
2.4. Streamlined Clinical Workflows and Provider Productivity
Virtual triage contributes significantly to reducing the workload for healthcare providers by automating various aspects of the triage process. This automation allows clinicians to dedicate more time to providing direct care to patients who need it most, rather than being consumed by administrative tasks. AI-powered triage assistants are particularly effective in streamlining remote patient triaging through automated workflows, which in turn improves clinical efficiency and patient prioritization. Telemedicine, encompassing remote triage, enhances overall operational efficiency by facilitating faster decision-making and more effective resource allocation to manage patient flow. Advanced AI-driven chatbots can handle initial patient interactions, collect symptoms, and triage queries even before patients arrive at a facility, substantially reducing physician workload without compromising the quality of care. Ultimately, virtual triage optimizes patient flow towards the most appropriate treatment pathway, saving valuable time for both patients and treatment facilities.
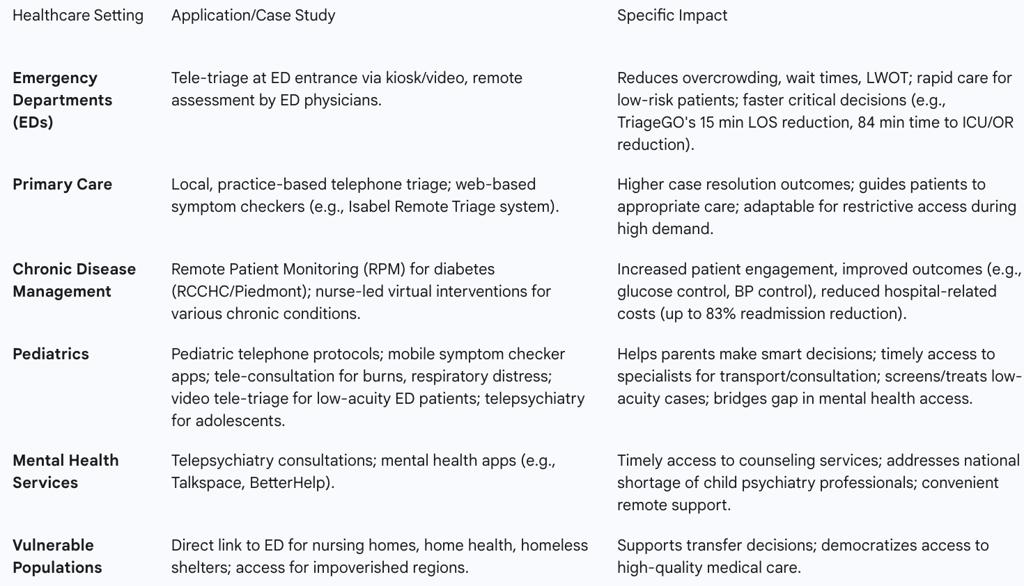
Table 1: Quantifiable Benefits of Remote Triage
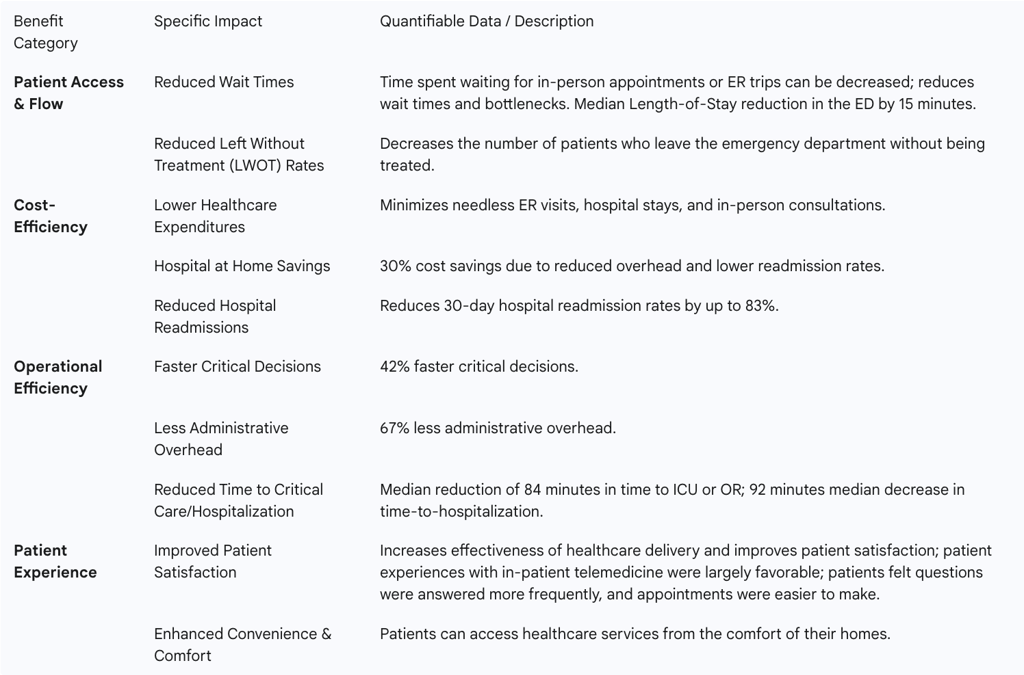
Note: While many studies report improved patient satisfaction, some evidence suggests heterogeneity and that satisfaction may be influenced by patient expectations. Additionally, some studies indicate remote triage does not consistently decrease primary care or ED utilization, and may even increase it, suggesting its primary benefit is in optimizing patient flow rather than reducing overall visits.
Key Technologies Powering Remote Triage
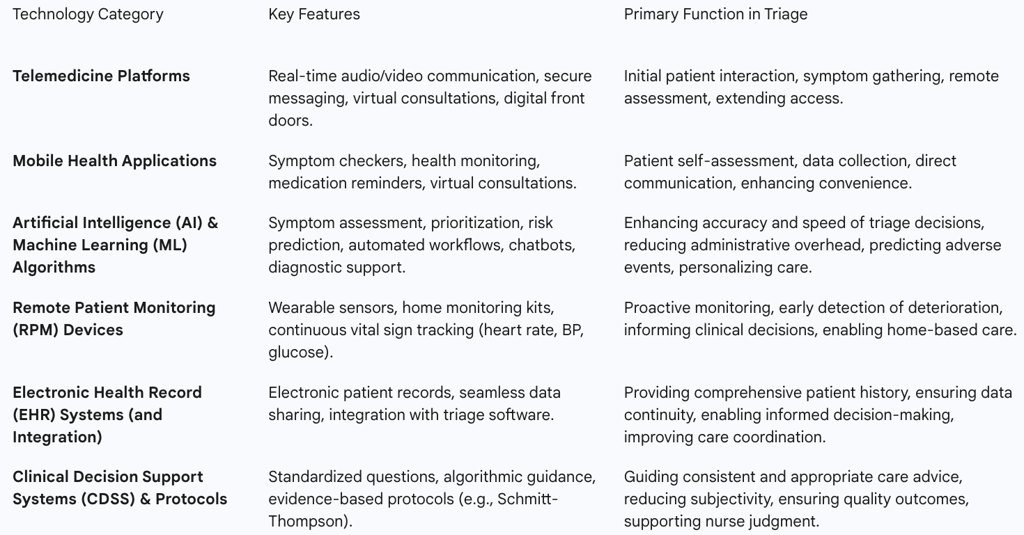
The efficacy and transformative power of remote triage are intrinsically linked to the sophisticated technological ecosystem that supports it. A combination of platforms, algorithms, and integrated systems enables the seamless assessment and management of patient needs from a distance.
3.1. Telemedicine Platforms and Mobile Health Applications
Telemedicine platforms form the backbone of remote triage, enabling real-time audio and video communication between patients and healthcare providers. These platforms often incorporate features such as secure messaging and file-sharing capabilities, facilitating comprehensive remote consultations and assessments. Video conferencing, for instance, is a widely utilized modality within these platforms. Complementing these platforms are mobile health applications, which empower patients to monitor their health status, track symptoms, and communicate with providers directly from their smartphones or tablets. These apps frequently include symptom checkers, medication reminders, and virtual consultation features, making healthcare more accessible and convenient for patients. Collectively, these technologies serve as crucial "digital front doors" to health systems, significantly improving accessibility and enabling patients to interact with care teams, schedule appointments, and conduct virtual visits with unprecedented ease.
3.2. Artificial Intelligence and Machine Learning Algorithms
Artificial Intelligence (AI) and Machine Learning (ML) algorithms are rapidly becoming indispensable tools in remote triage. AI-powered triage tools are designed to assess patient symptoms and prioritize care based on severity, utilizing advanced algorithms to analyze patient data and generate informed recommendations. AI enhances traditional Remote Patient Monitoring (RPM) by enabling closer monitoring, earlier problem detection, and quicker intervention. Some cutting-edge solutions embed AI directly into RPM devices, allowing for autonomous diagnostic capabilities.
Studies from institutions like Johns Hopkins University and Stanford indicate that AI-powered triage systems can identify high-risk patients more rapidly and with fewer errors compared to conventional methods. A notable example is TriageGO, which employs machine learning algorithms to provide acuity-level recommendations to nurses based on the risk of various clinical outcomes. This has demonstrated tangible benefits, including reductions in Emergency Department (ED) length-of-stay and decreased time to critical care interventions like ICU or OR transfers. AI's capacity to analyze vast amounts of patient data, detect anomalies, and alert providers to potential issues before they escalate to critical levels is a significant advantage. Furthermore, AI-driven chatbots are increasingly being deployed to handle initial patient interactions, collect symptoms, and triage queries, thereby reducing the administrative workload for physicians without compromising care quality. These systems leverage natural language understanding to interpret patient needs effectively. AI models also possess the capability to predict disease severity and the likely length of hospitalization during viral outbreaks, which is crucial for optimizing resource allocation in times of high demand.
The effectiveness of AI in remote triage is profoundly influenced by the quality, completeness, and accessibility of the data it processes. AI's capabilities are repeatedly linked to its ability to "analyze vast amounts of patient data" and "learn from large sets of clinical data". This highlights that robust Electronic Health Record (EHR) integration is not merely beneficial but essential for providing the necessary data foundation. Without seamless EHR integration and secure data exchange mechanisms, the full potential of AI in remote triage remains significantly constrained. This underscores the critical need for interoperability as a foundational requirement for the successful adoption of advanced AI technologies.
The role of AI is evolving beyond simple automation of routine tasks to a more sophisticated augmentation of clinical decision-making. While some AI tools are described as having "autonomous diagnostic capabilities" or handling "initial patient interactions" and "triage queries without needing staff" , other descriptions emphasize AI's function in "alerting healthcare providers" , "providing guidance to home caregivers" , "generating a preliminary care plan for review, edit, and approval" , or offering "acuity-level recommendation to the nurse". This duality indicates that AI's strength lies not in completely replacing clinicians, but in empowering them with faster, more accurate insights and significantly reducing administrative burdens. This allows clinicians to dedicate their expertise to complex cases and deliver more personalized care. This shift has considerable implications for workforce training and adaptation, necessitating a focus on collaborative human-AI workflows.
3.3. Remote Patient Monitoring (RPM) and Electronic Health Record (EHR) Integration
Remote Patient Monitoring (RPM) systems utilize digital devices such as wearable sensors, blood pressure monitors, scales, and pulse oximeters to continuously track patient health outside traditional clinical settings. This continuous data flow enables proactive interventions and allows clinicians to adjust care plans based on real-time, remotely gathered data.
The seamless integration of RPM data with Electronic Health Record (EHR) systems is paramount. EHR systems facilitate the electronic access and management of patients' medical records, enabling the smooth sharing of patient information across different healthcare settings. This ensures that providers have immediate access to relevant clinical data during remote consultations, leading to more informed decision-making. Integrating triage software directly with EHRs ensures that triage notes are automatically linked to the correct patient record, making them immediately visible to the entire care team and supporting more accurate reporting and follow-up. Enhanced interoperability between various EHR systems further streamlines data sharing, eliminating data silos and ultimately optimizing patient outcomes.
3.4. Clinical Decision Support Systems (CDSS) and Protocols
Clinical Decision Support Systems (CDSS) are integral to the remote triage process. These systems, often incorporating decision-support algorithms, are deployed to assess self-reported patient concerns and guide the appropriate sequencing of care. Standardized protocols, such as the widely adopted Schmitt-Thompson protocols, serve as algorithmic guides for nurses conducting remote assessments. These protocols ensure consistent care advice and help direct patients to the appropriate level of care based on the severity of their symptoms, rather than aiming for a definitive diagnosis. These protocols are not merely rigid rules but are described as decision support tools that nurses apply with their enhanced assessment skills, superior judgment, and extensive experience, leading to safe and quality outcomes.
Table 2: Core Technologies Enabling Remote Triage
Diverse Applications Across Healthcare Settings
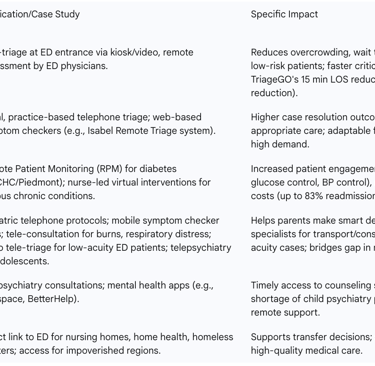
The versatility of remote triage allows its effective application across a broad spectrum of healthcare settings, each benefiting from its capacity to optimize patient flow and resource utilization.
4.1. Emergency Departments (EDs)
Tele-triage plays a crucial role in emergency departments by screening patients remotely to determine their condition and care needs even before or upon their arrival. The benefits in this high-pressure environment are substantial: it significantly reduces overcrowding, wait times, and bottlenecks by processing patients more quickly. This rapid assessment capability ensures that low-risk patient populations with low-risk health conditions receive prompt care, which in turn reduces the number of patients who leave the emergency department without being treated (LWOT). Implementation can range from patients using web or app-based tools at home to on-site kiosks or video interactions upon ED entry. Telemedicine further empowers ED physicians to assess patients remotely, prioritize critical cases, and streamline the admission process. The impact is evident in reduced patient congestion, quicker treatment initiation, faster consultations, and enhanced patient throughput. Advanced AI tools like TriageGO have demonstrated measurable improvements, including a median Length-of-Stay reduction of 15 minutes in EDs and an 84-minute median reduction in time to ICU or OR for critical patients.
4.2. Primary Care and Chronic Disease Management
In primary care, remote triage assists patients in accessing appropriate levels of care, often through technology-based systems. Evidence suggests that local, practice-based telephone triage services tend to achieve higher case resolution outcomes and refer fewer patients to emergency or primary care services compared to more regional or national telephone-based remote triage models. This indicates that integrating remote triage deeply within existing practice workflows can yield more effective results.
For chronic disease management, telemedicine facilitates continuous monitoring and regular check-ins, which can significantly reduce complications and the need for repeat ED visits. Remote Patient Monitoring (RPM) is particularly valuable here, enabling clinicians to proactively adjust care plans based on remotely gathered data for patients with chronic conditions. A compelling illustration is the Patient Provider Telehealth Network case study involving RCCHC and Piedmont, where the implementation of post-discharge remote monitoring and chronic care management for diabetes patients led to dramatically increased patient engagement, improved outcomes, and reductions in hospital-related costs. Virtual care interventions, especially those led by nurses, have demonstrated benefits in enhancing symptom management, promoting self-care behaviors, and improving various clinical controls such as weight, glucose, and blood pressure for individuals with chronic diseases.
While remote triage is broadly recognized for its benefits, its impact on reducing ED and primary care utilization has been observed to be mixed. However, local, practice-based services consistently show higher case resolution rates. This observation suggests that the effectiveness of remote triage is not uniform but is highly dependent on its specific implementation context, organizational structure (e.g., local versus regional/national), and how seamlessly it integrates within existing care pathways. This implies that for optimal results, healthcare systems should prioritize localized, integrated remote triage solutions that are deeply embedded within specific practice workflows, rather than adopting generic, centralized models. Furthermore, this highlights the necessity for tailored metrics to evaluate success based on the specific application, such as ED decongestion versus chronic disease management, rather than relying on a one-size-fits-all assessment.
4.3. Pediatrics and Mental Health Services
Remote triage extends its reach to specialized populations, offering critical support in pediatrics and mental health. In pediatric care, structured telephone protocols guide nurses and other medical providers in making timely decisions about whether a child requires immediate attention. Mobile applications, such as the ChildrensMD Symptom Checker, provide parents with essential care guidelines, empowering them to make informed decisions about when to seek professional medical advice or manage care at home.
Specific case examples in pediatrics underscore the versatility of telehealth: it facilitates crucial prehospital transport decisions, such as assessing burn severity via securely transmitted pictures from paramedics. Video tele-triage systems can efficiently screen and treat low-acuity patients in EDs, particularly valuable during surges in respiratory viral illnesses. Tele-consultation further aids in diagnosing conditions like skin rashes and respiratory illnesses, and in determining the need for interventions such as laceration repair.
For mental health services, telepsychiatry effectively bridges the significant gaps in timely access to child psychiatry professionals, offering an efficient and cost-effective means for consultations, especially for critical screenings like suicidality. Various mental health applications provide online therapy and support, making psychological care more accessible and convenient.
The inclusion of mental health services and specific case studies like telepsychiatry for suicidal ideation demonstrates that the utility of remote triage extends far beyond addressing traditional physical symptoms. This expansion signifies that the capabilities of remote triage are amplified by its ability to meet the growing demand for mental and behavioral health services. This is particularly relevant in underserved areas or for sensitive issues where the necessity of an in-person visit might pose a significant barrier to seeking help. This broader application enhances its strategic value as a comprehensive tool for healthcare access, addressing a wider array of patient needs.
4.4. Support for Vulnerable Populations
Remote triage serves as a vital tool in supporting vulnerable populations by providing a direct link to healthcare services. It assists patients in nursing homes, home health settings, and homeless shelters by connecting them directly to the emergency department, facilitating decisions on whether and when a patient needs to be transferred. This mechanism ensures that medical care services are available and accessible to patients living in impoverished regions globally, by accelerating case evaluation and alleviating the burden of delays. Remote Patient Monitoring (RPM) is particularly impactful in this context, viewed as a "great equalizer" in healthcare due to its capacity to democratize access to high-quality medical care for all, regardless of their socioeconomic or geographic circumstances.
Table 3: Remote Triage Applications and Case Studies by Healthcare Setting
Challenges and Critical Considerations for Implementation
Despite its numerous advantages, the widespread and effective implementation of remote triage systems encounters several significant challenges that require careful consideration and strategic mitigation.
5.1. Ensuring Accuracy, Patient Safety, and Mitigating Misdiagnosis Risks
A primary challenge in remote triage stems from the inherent difficulty of conducting a thorough physical examination from a distance. This limitation can impede the capacity to make an appropriate diagnosis and treatment decisions. Remote triage staff, such as nurses, are confined to gathering information through detailed questioning and attentive listening, lacking the ability to visualize physical signs, detect odors, palpate, or use a stethoscope. This constraint contributes to the potential for adverse events linked to remote triage. Safety incidents are often characterized by the use of inappropriate modalities, poor rapport building, inadequate information gathering, limited clinical assessment, and adherence to inappropriate pathways or algorithms. These issues can culminate in missed, inaccurate, or delayed diagnoses, underestimation of symptom severity or urgency, delayed referrals, incorrect or delayed treatment, insufficient safety netting, and inadequate follow-up care. Studies indicate that triage accuracy can vary widely, ranging from 48.8% to 90.1%, with some studies reporting up to 15% under-triage. Furthermore, the introduction of digital health technologies, while beneficial, also introduces new risks for medical error and potential malpractice liability.
5.2. Interoperability and Data Management Complexities
A significant hurdle to the seamless operation of remote triage is the pervasive challenge of interoperability and data-sharing limitations within healthcare systems. When different healthcare systems, staff, and software platforms cannot effectively communicate and exchange data, vital patient information can become siloed, rendering it unavailable to other systems that depend on it. This issue is compounded by the use of disparate data standards across various Electronic Health Record (EHR) platforms, security protocols that may block third-party data access, and a lack of prioritization for integration within health systems' triage workflows. Consequently, manual processes for transferring triage notes to EHRs become necessary, which are time-consuming and prone to error. This can lead to delayed or lost notes, increased call and patient wait times, redundant data entry, and critical communication breakdowns between nurses and providers.
5.3. Staffing, Training, and Workflow Integration
Successful implementation of remote triage necessitates careful consideration of staffing, training, and integration into existing workflows. Adequate initial and ongoing training for individuals serving as remote triage staff is crucial, alongside fostering a work environment that supports their physical and emotional well-being. Challenges frequently reported include a lack of necessary training for nurses, insufficient support for triage personnel, and the burden of heavy workloads. Given that implementing a remote triage service is a multifactorial process, purposeful planning both prior to and throughout its implementation is paramount to ensuring its success. This planning must account for how remote triage influences existing clinic workflows, appointment scheduling and availability, and the workload distribution among both clinical and non-clinical call handlers. Furthermore, staff require a thorough understanding of AI advice and automation to foster trust and ensure effective utilization.
Many of the challenges in remote triage stem from the intricate interaction between human operators and technology. Issues such as miscommunication , difficulties in ensuring patient comprehension of advice , the necessity for comprehensive staff training , and addressing patient digital literacy gaps are recurrent themes. The inherent limitations of remote physical assessment directly impact the accuracy of diagnoses. This indicates that the effectiveness of remote triage is ultimately constrained by the weakest link in this human-technology interface. Therefore, investment in technology must be complemented by equally robust investment in user-centric design, comprehensive staff training, patient education regarding the purpose and limitations of the service , and proactive efforts to bridge digital literacy divides. This comprehensive approach is essential to maximize safety and overall effectiveness, advocating for a socio-technical systems perspective in implementation.
5.4. Ethical, Legal, and Privacy Concerns
Protecting patient privacy constitutes a significant ethical challenge within telemedicine, demanding strict adherence to privacy laws such as the Health Insurance Portability and Accountability Act (HIPAA). Concerns regarding patient security, confidentiality, and privacy issues are frequently cited as obstacles to successful implementation. Difficulties in obtaining truly informed consent from patients for telehealth services are also noted. Legal barriers further encompass concerns related to forensic medicine, including potential medical negligence and malpractice claims arising from remote interactions. To navigate these complexities, clear guidelines are necessary regarding how to obtain appropriate consent for telemedicine, establish data security rules aligned with new technologies, clarify licensing regulations for providers operating across state lines, and assign responsibility for AI mistakes and automation problems. Physicians are also ethically obligated to disclose any financial interests in telehealth applications and ensure the objectivity and accuracy of any health information attributed to them.
The rapid advancement of remote triage technologies, particularly AI, appears to be progressing faster than the development of comprehensive ethical and legal frameworks to govern their use. Concerns about AI accountability , data security , informed consent for telemedicine , and potential malpractice liability are fundamental ethical and legal principles that become increasingly complex in a remote, AI-driven care environment. This suggests that the full capabilities of these technologies cannot be safely or responsibly realized without clear, universally accepted guidelines concerning responsibility, data governance, and patient rights within a virtual setting. This situation necessitates proactive and collaborative efforts among healthcare organizations, policymakers, and legal experts to establish robust frameworks.
5.5. Patient Perception, Digital Literacy, and Expectations
The impact of remote triage on patient satisfaction is often heterogeneous and significantly influenced by the degree to which patients perceive the received triage service to align with their expectations of care at the time of contact. A key challenge lies in ensuring that patients fully understand the advice provided remotely, as miscommunication can lead to detrimental outcomes due to delayed self-care or treatment. Barriers to access also include a lack of electronic devices, unreliable internet access, and a general reluctance among some patients to adopt telehealth solutions. Digital health literacy levels represent a significant barrier, particularly in low-income countries. While many patients express broad acceptance and appreciate the convenience of remote care, some still articulate a preference for in-person consultations. It is also noteworthy that a substantial proportion of older patients may require assistance to effectively utilize virtual triage platforms
Future Outlook: Innovations and Strategic Imperatives
The trajectory of remote triage is marked by continuous innovation, driven by technological advancements and evolving healthcare demands. Its future impact will be shaped by the strategic integration of emerging technologies and responsive policy frameworks.
6.1. Advancements in AI, Predictive Analytics, and Autonomous Capabilities
Artificial intelligence is poised to enable increasingly precise and personalized patient monitoring. AI-powered diagnostics will analyze complex medical images, such as CT scans and X-rays, with a speed and accuracy that rivals human interpretation, facilitating earlier disease detection and more tailored treatment plans. Predictive analytics, leveraging vast historical patient data, will become instrumental in forecasting demand, identifying potential peak periods for healthcare services, and optimizing resource allocation accordingly. AI-powered triage platforms will advance to predict patient disease severity and the likely length of hospitalization, which will be crucial for efficient resource optimization, especially during public health crises and viral outbreaks. Furthermore, machine learning algorithms are expected to enable survival prediction and remote triage via wearable devices, significantly reducing the time required for initial assessment. AI will continue to transform patient evaluations, enhance risk assessment, and automate routine administrative tasks, thereby improving overall efficiency.
The future of remote triage is characterized by a fundamental shift towards proactive, personalized, and predictive healthcare. The emphasis on AI's role in "earlier disease detection and personalized treatment plans" , "proactive interventions" , "predicting patient management needs" , and "forecasting demand" signals a profound transformation in healthcare delivery. This progression means that the capabilities of remote triage in the future will be less about merely reacting to symptoms and more about enabling a healthcare system that is truly anticipatory, tailored to individual needs, and capable of predicting health trajectories. This will evolve patient engagement from episodic interactions to continuous monitoring and management, potentially leading to significantly better health outcomes and a more sustainable healthcare model. This future also implies an increased reliance on data analytics and a higher level of AI literacy across the entire healthcare workforce.
6.2. Evolution of Multi-modal and Integrated Care Models
Future interventions in remote triage are expected to expand beyond traditional telephone-based services to encompass a wider array of modalities, including video, web, and mobile applications. The healthcare landscape will increasingly feature hybrid telehealth and in-person care models, strategically blending digital and face-to-face consultations to provide seamless and comprehensive patient experiences. Innovative solutions are emerging that will extend care further upstream, enabling providers to engage patients at the earliest onset of symptoms, thereby facilitating earlier identification of health risks and exacerbations. Enhanced interoperability between Electronic Health Record (EHR) systems will be critical in this evolution, facilitating smoother data sharing, eliminating data silos, and ultimately optimizing patient outcomes across the care continuum. Virtual care platforms are also expanding their scope to include a broader range of healthcare professionals, such as nurse practitioners, pharmacists, dietitians, and care coordinators, moving beyond urgent care to encompass preventive health and chronic disease management.
Remote triage, while initially focused on screening and prioritization, is increasingly becoming a gateway to a broader, integrated virtual care continuum. The future vision includes "remote patient monitoring expansion" , the proliferation of "Hospital at Home" programs , and the adoption of "hybrid telehealth and in-person care models". This indicates that remote triage is not an isolated function but a critical entry point and an ongoing component of a comprehensive virtual care strategy. Its future strength lies in its seamless integration into a full "tele-continuum" that spans prevention, acute care, chronic disease management, and post-acute follow-up. This integration will blur the traditional lines between care settings, necessitating strategic planning for end-to-end digital patient journeys that are cohesive and patient-centered.
6.3. Policy and Regulatory Landscape Evolution
The evolving policy and regulatory landscape will play a crucial role in shaping the future of remote triage. The easing of regulations and changes to encourage reimbursements for Remote Patient Monitoring (RPM) interventions, as observed with CMS approving Hospital at Home programs, highlight the importance of supportive policy in driving adoption and innovation. Future developments will likely involve the establishment of clear ethical guidelines for the growth and integration of telemedicine, necessitating proactive collaboration among healthcare organizations, policymakers, and nursing associations. Addressing existing legal barriers, such as concerns around patient security, confidentiality, and potential malpractice, will require the adoption of robust international standards (e.g., ISO/IEC 27001, HIPAA-like standards) to ensure data protection and accountability. Policymakers' recognition of RPM's potential to reduce costs and improve patient outcomes will continue to drive supportive legislative and regulatory changes.
Maximizing the Potential of Remote Triage
Remote triage stands as a powerful and indispensable component of modern healthcare, demonstrating a profound capacity to enhance accessibility, optimize efficiency, and improve patient outcomes. Its utility extends beyond immediate symptom management, enabling a strategic shift towards proactive health management and integrated care delivery. The strength of remote triage manifests in its ability to streamline patient flow, alleviate the burden on traditional healthcare facilities, and facilitate intelligent navigation to the most appropriate level of care, whether that involves self-management, a primary care visit, or urgent intervention. Furthermore, its capacity to enable systemic shifts, such as home-based care models, unlocks deeper, long-term cost savings by preventing costly hospitalizations and readmissions.
While the implementation of remote triage systems presents various challenges—including ensuring diagnostic accuracy, managing complex interoperability, addressing staffing and training needs, and navigating intricate ethical and privacy concerns—these obstacles are largely surmountable. Overcoming them requires strategic planning, targeted technological investment, and a steadfast focus on the human element, encompassing comprehensive staff training, clear patient education, and the development of robust ethical frameworks. The future of remote triage is characterized by transformative advancements in AI and predictive analytics, which promise to usher in a new era of proactive, personalized, and predictive healthcare. Realizing the full potential of remote triage demands a holistic and integrated approach that judiciously leverages these technological innovations while prioritizing patient safety, data integrity, and equitable access for all.
Recommendations for Healthcare Leaders and Policymakers
To fully harness the transformative capabilities of remote triage and ensure its sustainable integration into the healthcare ecosystem, the following recommendations are put forth for healthcare leaders and policymakers:
Invest in Integrated Technology Infrastructure: Prioritize investment in interoperable Electronic Health Record (EHR) systems and integrated remote triage platforms. These systems must seamlessly share data across the entire care continuum to ensure comprehensive patient information is available for informed decision-making.
Embrace AI Ethically and Strategically: Develop clear policies and guidelines for the ethical integration of AI in remote triage. The focus should be on AI's role in augmenting, rather than fully automating, clinical decision-making, ensuring continuous clinician oversight, and proactively addressing issues of accountability and algorithmic bias. Strategic investment in AI tools for predictive analytics and risk stratification should be pursued to enhance early intervention capabilities.
Prioritize Comprehensive Workforce Training and Support: Implement robust and ongoing training programs for all healthcare staff involved in remote triage, encompassing both clinical protocols and technological proficiency. Foster a supportive work environment that addresses the physical and emotional well-being of remote staff to mitigate burnout and ensure sustained quality of care.
Develop Patient-Centric Engagement Strategies: Educate patients and their families comprehensively on the purpose, benefits, and limitations of remote triage services. Actively manage patient expectations regarding care delivery and provide accessible, user-friendly interfaces for all remote platforms. Proactive measures should be taken to address digital literacy disparities to ensure equitable access to these services across all demographics.
Advocate for Supportive Policy and Reimbursement Models: Collaborate actively with policymakers to establish clear, consistent regulatory frameworks, licensing guidelines, and reimbursement policies that incentivize the widespread adoption and scaling of remote triage and broader virtual care models. This regulatory clarity is vital for fostering innovation and investment.
Establish Robust Data Governance and Cybersecurity Measures: Implement and continuously update stringent security protocols to protect patient privacy and ensure the integrity of health data. Adherence to established standards like HIPAA is non-negotiable, and continuous monitoring for evolving cyber threats is essential.
Foster Continuous Evaluation and Quality Improvement: Implement rigorous metrics to assess the effectiveness and efficiency of remote triage systems on an ongoing basis. Evaluation should focus on key outcomes such as patient safety, clinical outcomes, resource utilization, and patient satisfaction. Data derived from these evaluations should be used to identify areas for improvement and adapt strategies dynamically.
Explore Hybrid Care Models: Design and implement care pathways that strategically blend remote and in-person care components. This approach leverages the distinct strengths of each modality to provide optimal patient experience and achieve superior health outcomes, creating a truly integrated and flexible healthcare delivery system.
FAQ Section
Q: What is remote triaging?
A: Remote triaging is the process of evaluating and prioritizing patient needs and conditions remotely, using various technologies to facilitate effective communication and assessment1.
Q: What are the benefits of remote triaging?
A: Benefits include expanded access to care, early intervention, resource utilization, improved patient safety, and convenience for patients3412.
Q: What tools are essential for effective remote triaging?
A: Key tools include telehealth platforms, AI and machine learning, and electronic health records (EHRs)42.
Q: What challenges are associated with remote triaging?
A: Challenges include technology barriers, communication issues, privacy concerns, and the need for adequate staff training5.
Q: How can the challenges of remote triaging be addressed?
A: Addressing challenges involves bridging the digital divide, enhancing communication, ensuring data security, and providing comprehensive training for healthcare staff5.
Q: What is the future of remote triaging?
A: The future of remote triaging includes AI-incorporated assessments, expanded telemedicine access, better self-service options, and real-time data analytics2.
Q: How does remote triaging improve patient outcomes?
A: Remote triaging improves patient outcomes by facilitating timely consultations, enabling prompt interventions, and enhancing recovery rates5.
Q: Can remote triaging reduce healthcare costs?
A: Yes, remote triaging can reduce healthcare costs by minimizing unnecessary in-person visits and decreasing overhead costs for healthcare organizations6.
Q: Is remote triaging suitable for managing chronic conditions?
A: Yes, remote triaging is suitable for managing chronic conditions through regular virtual check-ins, symptom monitoring, and treatment adjustments2.
Q: How does remote triaging enhance patient safety?
A: Remote triaging enhances patient safety by enabling timely identification of severe symptoms and quicker interventions, translating into enhanced health outcomes2.
