The Portuguese Triage System
The Portuguese Triage System (PTS) is fundamentally and legally anchored in the Manchester Triage System (MTS), a five-level, color-coded protocol that is one of the most widely used in Europe. The system's implementation in Portugal was a strategic and progressive evolution, beginning with a voluntary initiative.


The Portuguese Triage System (PTS) is fundamentally and legally anchored in the Manchester Triage System (MTS), a five-level, color-coded protocol that is one of the most widely used in Europe. The system's implementation in Portugal was a strategic and progressive evolution, beginning with a voluntary initiative by pioneering hospitals in 2000 and culminating in a national mandate from the Ministry of Health in 2005. The Grupo Português de Triagem (GPT), a non-profit association, is the entity responsible for the protocol’s management, implementation, training, and auditing.
The analysis indicates that the MTS is a validated and effective tool, with a demonstrated ability to predict crucial patient outcomes such as hospital admission and short-term mortality. However, the system's operational success is contingent on a complex, multi-layered ecosystem that extends beyond the hospital emergency department (ED). This includes the pre-hospital telephone triage service SNS 24, which acts as a primary filtering mechanism, and new digital models like the SINACC for managing specialty consultation waiting lists.
Despite its strengths, the system faces significant challenges. Chief among these is the human element: the immense pressure, cognitive burden, and undervalued role of the triage nurse, who must often make complex, high-stakes decisions that transcend the protocol's rigid framework. Systemic inefficiencies, such as the persistent overcrowding of EDs by non-urgent patients, also strain resources and can compromise care.
Based on these findings, the future of the PTS requires strategic investment to address these limitations. Recommendations include enhancing professional training for triage nurses, integrating advanced technological solutions like AI-assisted decision support, and strengthening the coordinated link between primary care, pre-hospital services, and hospital EDs to optimize patient flow and ensure clinical excellence.
Foundational Framework and Official Mandate
The Genesis of the Portuguese Triage System (PTS)
The adoption of a standardized triage system in Portugal was a direct response to a critical need for organized patient flow in emergency services. Prior to the implementation of the MTS, emergency departments were often overwhelmed by non-urgent cases, which led to significant delays in the observation of patients who required immediate medical attention. This "first-come, first-served" model compromised care quality and patient safety, highlighting the urgent need for a method to prioritize care based on clinical severity.
The MTS was created in Manchester, UK, in 1994, with the explicit goal of establishing a consensus among emergency physicians and nurses to create triage standards based on clinical risk determination. This methodology provided the blueprint for a solution in Portugal. The initial implementation was not a top-down mandate but a pioneering grassroots effort. In October 2000, two major hospitals—Hospital Fernando Fonseca in Amadora and Hospital de Santo António in Porto—voluntarily adopted the Manchester Triage Protocol (PTM). This represented a radical change in their operational structure, as it reorganized emergency services based on clinical priority rather than patient arrival time. The success of this pilot initiative led to the formation of the Grupo Português de Triagem (GPT) in 2001, in partnership with the Ministry of Health, to consolidate the methodology and expand its implementation to other hospitals.
Legal and Governmental Adoption
The success of these pioneering efforts served as the evidence base for a decisive policy shift at the national level. In 2005, the Ministry of Health formally recognized the importance of a structured triage system for the management of hospital emergency care. The Despacho n.º 19124/2005 officially mandated that all hospitals in the National Health Service (SNS) that had not yet implemented a priority triage protocol must do so by December 31 of that year. This decree recognized the Manchester Triage Protocol as a proven instrument for clinical decision support and patient management, effectively transforming a successful local initiative into a mandatory national standard.
The GPT was formally entrusted with the responsibility of disseminating the protocol and ensuring its uniform implementation across the national network of urgency and emergency services. This legal framework provided the necessary authority and accountability, ensuring that the system would be consistently applied and monitored.
Methodological Principles of the Manchester Triage System (MTS)
The MTS is a structured, algorithmic approach that provides a clinical priority to patients based on their presenting signs and symptoms, rather than a definitive diagnosis. The system is built upon a list of 52 flowcharts that cover a comprehensive range of patient complaints, such as “Headache,” “Shortness of breath,” and “Wounds”. The triage process is a focused clinical encounter where a trained nurse selects the most specific flowchart for the patient's complaint and then follows a series of clinical discriminators to determine the appropriate priority level.
The system uses a five-level, color-coded scale to classify patients and determines the maximum time they should wait before being seen by a physician.
Table 1: Manchester Triage System Priority Levels and Target Times
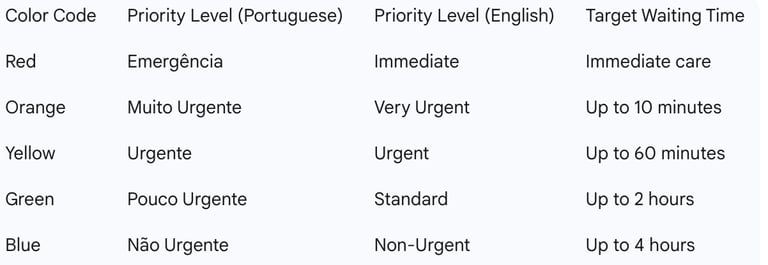
A key element of the MTS is the use of discriminators, which are the factors that allow for the patient’s inclusion in one of the five clinical priorities. These discriminators can be either general, such as "acute pain" or "level of consciousness," which apply to all flowcharts, or specific, such as "precordial pain" or "pleuritic pain," which are tied to individual clinical presentations. The methodology is designed to be rigorous, ensuring that a patient's priority level is determined by the first positive discriminator that leads to the highest clinical priority.
A notable adaptation to the MTS in Portugal is the implementation of a "White" code. This sixth classification is used to identify and monitor patients who use the emergency service for non-urgent administrative reasons, such as elective procedures, follow-up appointments, or unscheduled therapies. This specific addition reflects an attempt to address a recurring issue of ED misuse that is specific to the Portuguese healthcare context.
The Ecosystem of Triage in Portugal
The Role of Pre-Hospital and Community Triage (SNS 24)
The Portuguese Triage System is not a single, isolated protocol but a multi-modal ecosystem designed to manage patient flow across the entire healthcare continuum. A critical component of this ecosystem is the SNS 24 telephone line, a 24/7 service staffed by a multidisciplinary team of health professionals, including nurses, doctors, and pharmacists. The primary function of SNS 24 is to provide telephone triage, counseling, and referral for citizens with non-emergency acute health problems, with the goal of guiding them to the most appropriate level of care, such as self-care, a health center, or a hospital ED.
The “Ligue Antes, Salve Vidas” (Call First, Save Lives) pilot project, launched in 2023, represents a formalization and strategic enhancement of this pre-hospital triage system. This initiative aims to alleviate pressure on hospital EDs by encouraging citizens to call SNS 24 first, thereby optimizing healthcare resources. The project also introduced a "reverse referral" system, which directs non-urgent ED walk-in cases to primary care services. This strategic approach demonstrates a clear policy objective: to prevent unnecessary ED visits and protect hospital resources for true emergencies.
However, the efficacy of this pre-hospital filtering mechanism has faced challenges. Data from a recent period shows that nearly half of the individuals (44%) who called SNS 24 were still directed to hospital EDs, while only 11% were able to manage their condition with self-care at home. This indicates a persistent struggle to effectively divert non-urgent cases and highlights the ongoing systemic pressure on emergency services. The high referral rate may also reflect a lack of available primary care services, particularly on weekends, which a study on pediatric triage found to be a key reason for a high number of ED visits. This suggests that while the system of pre-hospital triage exists, its full potential is limited by a lack of coordinated, accessible primary care alternatives.
Hospital-Based Triage and Systemic Integration
In the hospital setting, the MTS is typically implemented using computerized protocols. Some hospitals have adopted sophisticated software solutions that integrate the Manchester Triage Protocol with their clinical systems and offer AI-assisted decision support. This technology helps triage nurses by asking additional questions based on a vast database of audited triages, which can enhance the accuracy and efficiency of the decision-making process.
The management of patient flow in Portugal extends beyond the emergency department through new models like the Sistema Nacional de Acesso a Cuidados de Saúde (SINACC). This new model replaces the previous one (SIGIC) and introduces a triage process for patients referred for specialty consultations. The objective of the SINACC is to prevent patients from being "forgotten on waiting lists" and to ensure timely access to specialist care. This system requires a triage consultation to be performed within two business days for priority patients and within five business days for all others, with all patient information registered digitally. This development demonstrates a holistic approach to patient management that views triage not as a process exclusive to the ED, but as an essential mechanism for managing patient flow across the entire hospital system, from emergency entry to specialized outpatient care.
Clinical Effectiveness and Performance Metrics
Validation and Predictive Power of the MTS
The Manchester Triage System's credibility in Portugal is not based solely on its structured methodology but on its proven clinical effectiveness. A significant study conducted at Hospital Fernando Fonseca in Lisbon, involving a large dataset of over 321,000 patients triaged between 2004 and 2007, provided robust evidence for the system's validity. The study's primary finding was a clear and strong association between the priority group assigned by the MTS and key indirect triage outcomes, namely hospital admission and short-term mortality.
The analysis revealed that patients classified in higher priority groups (Red and Orange) had a significantly greater number of short-term deaths and were more likely to be admitted to the hospital. Conversely, patients in lower priority groups (Yellow, Green, and Blue) had lower rates of death and were less likely to be admitted. The study concluded that the MTS is a powerful tool for distinguishing between patients with high and low unadjusted risks of death and hospital admission, providing valuable information that extends beyond its immediate use as a prioritization mechanism. This validation confirms the system's role as a vital risk management tool and a cornerstone of patient safety.
Quality Assurance and Auditing
The effectiveness and reproducibility of the MTS in Portugal are maintained through a rigorous and systematic auditing process. The Ministry of Health and the GPT have established a framework for quality assurance that includes both internal and external audits. Hospitals are required to conduct monthly internal audits of the triage system to ensure that the methodology and its results align with established criteria. The GPT, in its capacity as the governing body, is responsible for conducting external audits to ensure national-level consistency and quality.
These audits are guided by specific performance metrics. An accuracy rate of 80% in triage classifications is considered "good," a rate above 90% is deemed "very good," and a rate exceeding 95% is considered "excellent". This quantitative approach provides a clear standard for performance and allows for continuous monitoring and improvement. To support this system, the GPT also provides specialized training for instructors and auditors, enabling hospitals to gain greater autonomy in their internal quality control processes and the ongoing professional development of their staff.
Critical Analysis and Challenges in Practice
The Triage Nurse: A Complex and Undervalued Role
While the Manchester Triage System provides a structured protocol, its application is ultimately dependent on the professional judgment of the triage nurse. This role is fraught with complexity and significant pressure, and it involves far more than simply following a flowchart. Nurses must make rapid, high-stakes decisions with limited information and under immense pressure, which can lead to human error in classification.
A significant challenge arises from the tension between the system's rigid, algorithmic nature and the complex, nuanced reality of clinical practice. The nurse's responsibilities extend beyond assigning a priority level; they must also decide the order of patient care, identify critical situations that may not be immediately obvious, and even initiate diagnostic tests or therapies for conditions like stroke or sepsis before a physician's evaluation. This is particularly challenging when patients or their companions provide insufficient or unreliable information, or when the patient's condition is subtle or changes while they are waiting.
Despite the critical nature of this role, which requires broad clinical knowledge and the ability to make rapid, accurate decisions, triage nurses are often undervalued and undercompensated compared to their colleagues in other hospital departments. This lack of professional recognition and the constant pressure from a high volume of patients, limited resources, and aggressive patient interactions can unduly influence a nurse's decisions and lead to significant professional stress and dissatisfaction.
Systemic Limitations and the Need for Refinement
Despite its proven utility, the MTS is not without its limitations. The system can be susceptible to errors such as undertriage (classifying a serious condition as less urgent) and overtriage (overestimating the urgency of a case). A review of the literature notes that while the system’s overall sensitivity is moderate to good, it can fail to detect patients who deteriorate after the initial triage assessment.
Furthermore, the system’s design and discriminators have been identified as needing refinement in specific contexts. A study at Hospital Fernando Fonseca noted a "puzzling" inconsistency where the MTS was less effective at discriminating admissions between medical and surgical specialties. This suggests a potential bias or gap in the protocol's design that requires further investigation. A study on the pediatric application of the system also found that some professionals felt the discriminators for children needed improvement and revision to be more specific for that age group.
A Comparative Perspective
The Manchester Triage System is one of several prominent and validated triage scales used globally, alongside the Emergency Severity Index (ESI), the Australian Triage Scale (ATS), and the Canadian Triage and Acuity Scale (CTAS). These systems share the common objective of distinguishing between patients who require immediate medical attention and those who can safely wait for care.
A comparative analysis of these systems reveals both similarities and differences. One study suggests that the ESI may be more effective at distinguishing between low and high urgency levels and may have a reduced risk of undertriage compared to the MTS. However, another analysis found that the MTS was a more "inclusive" system and was more effective at predicting admission and death in the short term. The Portuguese Triage Group's work to implement the MTS in other Portuguese-speaking countries, such as Angola, Cape Verde, and Mozambique, positions Portugal not just as an adopter but as a developer and exporter of this clinical methodology.
Strategic Recommendations and the Future of Triage in Portugal
Strategic Recommendations
The analysis of the Portuguese Triage System reveals that while the Manchester Triage Protocol provides a robust and validated foundation for emergency care, its long-term success is contingent on a commitment to continuous evolution. The following strategic recommendations are proposed to address the identified challenges and enhance the system's effectiveness:
Enhance Training and Professional Development for Triage Nurses: The complex, high-stakes nature of the triage role necessitates advanced training that goes beyond basic protocol adherence. Training programs should be expanded to focus on developing clinical judgment, managing cognitive load, and building resilience to the psychological pressures of the job. The GPT should continue its crucial role in this area, focusing on protocol refinements for specific populations, such as pediatrics, where improvements have been identified as necessary.
Integrate Technological Innovations for Decision Support: The widespread use of computerized protocols presents a significant opportunity to integrate advanced technologies. The adoption of AI-assisted triage software could provide real-time decision support, ask targeted questions to improve accuracy, and serve as a valuable tool for supporting less experienced staff. This could help to mitigate the risk of human error and ensure greater consistency in classification.
Strengthen Systemic Integration and Patient Flow Management: The persistent issue of non-urgent patients overwhelming EDs requires a more robust, system-wide solution. This involves strengthening the link between the SNS 24 telephone triage line and primary care services. Policymakers should focus on improving access to primary care, particularly during weekends and non-business hours, to provide a viable and attractive alternative to the ED for non-urgent health issues. The "reverse referral" mechanism of the "Call First, Save Lives" project should be refined to ensure smooth and efficient patient transitions, reducing complexity and administrative friction.
Conclusion
The Manchester Triage System has been a cornerstone of emergency care in Portugal for over two decades, successfully shifting the paradigm from a "first-come" to a "first-needed" approach. Its legal mandate, combined with the continuous oversight and auditing by the GPT, has established a framework of quality and accountability. A large-scale study has provided empirical validation of its effectiveness, demonstrating a strong correlation between triage classification and key patient outcomes.
However, the system's future success depends on its capacity to evolve in response to contemporary challenges. The most critical area for development is the support and professionalization of the triage nurse's role. By investing in advanced training, leveraging technological innovations, and creating more seamless patient pathways between pre-hospital, primary, and hospital care, Portugal can not only maintain but enhance the effectiveness and safety of its triage system. This forward-looking approach will ensure that the Portuguese Triage System remains a model of clinical excellence in the 21st century.
