The Manchester Triage System vs Other Triage Systems
Explore the Manchester Triage System (MTS) and its comparison with other triage systems like ESI, CTAS, ATS, SATS, and RETTS. Understand their features, sensitivity, specificity, and real-world applications.

The Manchester Triage System (MTS) represents a paradigm shift in the initial assessment of patients in unscheduled care settings. It is not merely a sorting mechanism but a comprehensive and structured clinical risk management tool designed to bring objectivity, consistency, and safety to the chaotic environment of the emergency department (ED). Its global adoption is a testament to the fundamental need for a standardized approach to patient prioritization when clinical demand exceeds the capacity for immediate care. This section details the system's foundational principles, tracing its evolution from subjective, experience-based practices to a standardized, evidence-informed methodology that underpins modern emergency nursing practice.
1.1 Genesis and Philosophy: The Imperative for a Standardized Approach
The development of the MTS was a direct response to the inherent risks and inconsistencies of traditional triage methods. Before its inception, the process of prioritizing patients in the ED was often intuitive, relying heavily on the individual practitioner's clinical experience and subjective judgment. This approach, while often performed by skilled clinicians, suffered from critical flaws: it lacked consistency from one nurse to another, was not reproducible, and, crucially, was not auditable. This absence of a standardized framework created an environment where patient safety could be compromised, as queuing was often determined by the order of arrival rather than by clinical urgency.
Recognizing these deficiencies, a group of senior emergency nurses and physicians convened in Manchester, United Kingdom, in the 1990s. Their primary objective was to engineer a system that could minimize the variability in triage decisions. The goal was to ensure that patients presenting with similar conditions would be assessed and prioritized in a uniform manner, regardless of which trained professional was conducting the assessment. This effort was driven by the universal challenge faced by EDs worldwide: managing unpredictable and often overwhelming patient volumes with finite resources, including staff, space, and equipment.
The core purpose that emerged was the establishment of a robust system for clinical risk management. The MTS was designed to provide a safe, logical, and consistent method for managing patient flow, ensuring that the most critically ill or injured individuals receive immediate attention while others are seen in an order dictated by their clinical priority. By providing a structured and consistent assessment process, the system aims to minimize clinical risk and enhance overall patient safety. This structured approach has profound implications beyond the immediate clinical encounter. The shift from a non-auditable process, which is difficult to defend in cases of adverse events or litigation, to a standardized system with documented flowcharts and discriminators creates a clear, auditable trail of the decision-making process. The implementation of MTS is therefore as much an act of organizational risk management as it is of clinical risk management. It provides a defensible framework for triage decisions, shifting the focus in a potential dispute from "what did the nurse think?" to "did the nurse correctly apply the established, evidence-informed protocol?"
1.2 The Reductive Methodology: A "Safety First" Algorithm
At the heart of the MTS philosophy is its "reductive" methodology, a defining feature that hardwires a risk-averse, "safety first" principle into the triage algorithm. This approach fundamentally assumes that every patient presenting to the ED is potentially in a life-threatening condition, corresponding to the highest priority level (Priority 1 - Red). The task of the triage nurse is not to build a case for urgency but rather to systematically search for evidence that allows for the safe reduction of this assumed high priority.
The process requires the nurse to methodically rule out a series of high-priority signs and symptoms, known as discriminators, in a hierarchical fashion. Only after confirming the absence of immediate life threats and other high-risk indicators can the nurse "reduce" the patient's assigned priority to a lower level, such as Orange, Yellow, Green, or Blue. This design is explicitly risk-averse, architected to ensure that serious conditions are not inadvertently missed or down-triaged. This reductive methodology is a deliberate design choice that has significant downstream consequences. The system's inherent bias towards safety is a direct and predictable cause of one of its most frequently cited limitations: a high rate of overtriage, where patients are classified as more urgent than their condition ultimately warrants. This leads to the "unnecessarily high use of resources" noted in critical reviews. Therefore, the system's greatest strength—ensuring patient safety through a cautious, reductive approach—is inextricably linked to one of its most significant practical weaknesses: a potential for inefficient resource allocation. This is not a simple flaw to be engineered out of the system, but rather a core trade-off inherent in the MTS philosophy, prioritizing clinical safety over operational efficiency.
A second crucial aspect of the methodology is its strict focus on presentation, not diagnosis. Triage decisions are based on the patient's chief complaint, reported symptoms, and the nurse's objective observations—in short, "what the patient says is happening". The system does not require, nor does it permit, the triage nurse to make any assumptions about the underlying diagnosis. This principle ensures that the process remains a standardized assessment of symptoms and risk factors, rather than a premature and potentially inaccurate diagnostic exercise.
1.3 The Role of the Triage Practitioner: An Expert System
The MTS is explicitly designed as a professional, expert system, and its safe and effective use is contingent on the clinical acumen of the practitioner. The Manchester Triage Group (MTG), the governing body of the system, states unequivocally that the MTS was developed solely for use by registered Health Care Professionals (HCPs), such as nurses qualified to UK Band 5 or its international equivalent. This requirement is rooted in the recognition that a valid triage assessment demands a sophisticated level of clinical skill, knowledge of pathophysiology, and practiced judgment that non-HCPs do not possess.
Further emphasizing this point, the MTG recommends that the most, rather than the least, experienced clinical personnel in an emergency department should be assigned to the triage role. This guidance underscores the complexity of the task, which involves more than simply following a script. It requires the ability to elicit a relevant history, accurately interpret both verbal and non-verbal cues, and navigate the system's algorithms with clinical wisdom. Empirical research supports this position, with studies demonstrating that the reliability of MTS assessments is positively correlated with the nurse's years of professional experience in emergency care and risk classification.
The MTG's stance on this matter is not merely a recommendation but a cornerstone of its approach to patient safety and legal accountability. The group has made its position clear that it will not support organizations that permit non-HCPs to use the MTS. In the event of medical negligence proceedings, the MTG will provide a formal letter to the court to this effect, reinforcing the system's status as a tool for qualified professionals. This establishes a clear standard of care and places the responsibility for correct implementation firmly on the healthcare organization.
The Architectural Core: Priority Levels and Discriminators
The architectural core of the Manchester Triage System is built upon two fundamental components: a five-tiered urgency classification scale and a structured set of clinical "discriminators." Together, these elements form the engine of the triage process, providing a standardized, logical pathway that translates a patient's presenting symptoms into a clear clinical priority. This section dissects these building blocks to explain how the MTS decision-making algorithm functions.
2.1 The Five-Tiered Urgency Classification
The MTS framework allocates every patient to one of five distinct priority categories. This classification provides a common language for communicating clinical urgency throughout the hospital. Each category is consistently identified by a number, a descriptive name, and a color, and is critically linked to a maximum target time within which the patient should have their first contact with a treating physician or advanced practice provider.
The five priority levels are as follows:
Level 1: Red (Immediate): This category is reserved for patients with immediately life-threatening conditions that require instantaneous medical intervention. Upon assignment of a Red priority, all other ongoing, subordinate activities are expected to be interrupted to facilitate immediate care. The target time to physician contact is
0 minutes. Clinical examples include cardiac arrest, major trauma with hemodynamic instability, and active, prolonged seizures.
Level 2: Orange (Very Urgent): This level is for patients with serious, high-risk conditions that, while not immediately life-threatening, have the potential for rapid deterioration and require urgent assessment. The target time for physician contact is 10 minutes. Examples include patients with suspected stroke, sepsis, severe respiratory distress, or chest pain of suspected cardiac origin.
Level 3: Yellow (Urgent): This category includes patients with serious conditions that are not life-threatening but require prompt evaluation and could become more serious if delayed. There is a noted discrepancy in the literature regarding the target time for this level. Some sources, particularly from specific hospital implementations, cite 30 minutes , while the official handbooks and other widespread guidance specify
60 minutes. The 60-minute standard is the most commonly accepted target. Clinical examples include moderate abdominal pain, possible limb fractures without neurovascular compromise, and moderate chest pain not meeting Orange criteria.
Level 4: Green (Standard): This level is for patients with non-life-threatening conditions that still require assessment and treatment in a timely manner. As with the Yellow category, target times vary in the literature, with some sources citing 90 minutes and others specifying
120 minutes (2 hours). The 120-minute standard is more common. Examples include minor burns, simple, uncomplicated fractures, and mild asthma attacks.
Level 5: Blue (Non-Urgent): This is the lowest priority level, reserved for patients with minor complaints or injuries that can safely wait for an extended period before being seen. Again, target times vary between 120 minutes and the more widely accepted standard of
240 minutes (4 hours). Examples include minor cuts and abrasions, mild skin rashes, and symptoms of a mild upper respiratory infection.
It is critical to recognize that these discrepancies in target times for the lower-acuity levels are not necessarily errors in the literature but reflect a key feature of the system's implementation. As noted in the preface to the official MTS handbook, while the clinical priority level (the color) is an absolute clinical indicator derived from the patient's presentation, the associated waiting time targets are often set locally. These targets can be influenced by regional health policy, departmental resources, and even political pressures. This distinction is crucial: the clinical assessment is standardized by the MTS, but the operational performance targets are adaptable. This explains the variations seen across different reports and highlights the fact that comparing hospital performance based solely on waiting times can be misleading without first understanding their locally defined targets.
Additionally, some healthcare systems have adapted the MTS framework to meet specific local needs. For instance, the Portuguese Triage Group implemented a supplementary "White" category to identify and track individuals presenting for purely administrative reasons, such as scheduled follow-up appointments or elective procedures, thereby separating them from the stream of unscheduled emergency patients.
2.2 The Logic of Discriminators: The Engine of Triage
Discriminators are the core components of the MTS algorithm; they are the specific signs, symptoms, or historical factors embedded within each presentational flowchart that drive the triage decision. They are operationalized as a series of structured questions or observations that the triage nurse must consider. The presence of a single positive discriminator is sufficient to assign the patient to the corresponding priority level.
There are two main types of discriminators:
General Discriminators: These are six overarching key discriminators that represent fundamental principles of clinical risk and appear across numerous flowcharts. Their consistent application ensures that core threats are assessed for a wide variety of presentations. The six general discriminators are: Life Threat, Pain, Haemorrhage, Level of Consciousness, Temperature, and Acuteness of Onset.
Specific Discriminators: These are discriminators tailored to the specific context of a particular presentational flowchart. They provide the clinical granularity needed to stratify risk within a given complaint. For example, 'Increased work of breathing' is a specific discriminator found in the 'Shortness of breath in children' flowchart, while 'Persistent vomiting' is a specific discriminator within the 'Abdominal pain' flowcharts.
A foundational rule of the MTS, critical to its consistency and reliability, is that a given discriminator will always lead to the same urgency level, regardless of the presentational flowchart in which it is identified. For example, the discriminator 'Severe pain' will always triage a patient to the Orange (very urgent) category, whether the presenting complaint is a headache, abdominal pain, or a limb injury. This design feature greatly simplifies the system, reduces ambiguity, and is a key factor in promoting inter-rater reliability among triage nurses.
2.3 Hierarchical Assessment: The ABCDE Framework
The arrangement of discriminators within each of the 53 flowcharts is not arbitrary. They are meticulously sorted by clinical urgency according to the internationally recognized ABCDE scheme of emergency assessment: Airway, Breathing, Circulation, Disability (neurological status), and Exposure/Environment. This is a critical structural element that mirrors the standard approach to evaluating critically ill patients (as taught in courses like Advanced Trauma Life Support) and reinforces the system's risk-averse, reductive methodology.
In practice, this means the triage nurse must first assess for and rule out any immediate airway threats (e.g., stridor, gurgling). If none are present, the nurse proceeds to assess for life-threatening breathing problems (e.g., severe respiratory distress, cyanosis). This continues sequentially through circulation (e.g., signs of shock), disability (e.g., altered level of consciousness), and finally to other signs, symptoms, and historical factors. The documentation process reflects this hierarchy; rather than noting the absence of every single discriminator, the nurse provides a "summary confirmation" that all discriminators at a given priority level have been considered and ruled out before moving to the next lower level.
The algorithmic logic of the MTS is that of a "first-match" system. The nurse proceeds down the hierarchical list of discriminators, and the triage process for that patient concludes as soon as the first positive discriminator is identified. The patient is then allocated to the priority level associated with that specific discriminator. While this creates a highly efficient and reproducible pathway, it also introduces a degree of clinical rigidity. The system, by design, cannot aggregate the risk of multiple lower-level findings. For instance, a patient may present with a constellation of concerning but not individually critical symptoms (e.g., several "Yellow" level discriminators). An experienced clinician might holistically view this pattern as indicative of a sicker patient who warrants a higher, "Orange" level of urgency. However, because the MTS algorithm locks in the priority at the very first match, it is structurally incapable of performing this kind of risk aggregation. This represents a potential systemic weakness, particularly for patients with complex, atypical, or multi-system complaints where the overall clinical picture is more concerning than any single symptom.
A Comprehensive Analysis of the 53 Flowcharts
The practical application of the Manchester Triage System is executed through its comprehensive library of presentational flowcharts. These 53 algorithmic tools are the specific instruments used by triage nurses to translate a patient's story into a standardized clinical priority. This section provides a definitive overview of this canon, beginning with a master list of all flowcharts and then proceeding to a detailed analysis of the clinical logic, performance, and evolution of key representative charts from medical, trauma, and specialty domains.
3.1 Overview of the Presentational Flowcharts
The MTS is built upon a foundation of 53 distinct, presentation-based flowcharts. It is worth noting that a significant portion of the academic literature cites a total of 52 charts. This minor discrepancy is likely attributable to different versions of the system being studied over time or the specific inclusion/exclusion criteria of various research projects. This report uses the figure of 53, as stated by the governing Manchester Triage Group on its official website, which reflects the most current iteration of the system.
These flowcharts are designed to cover the vast majority of reasons why a patient might seek emergency care. They are not based on diagnoses but on the initial presenting complaint. This library of charts can be broadly grouped into several categories: Adult Medical, Pediatric-Specific, Trauma-Related, and Non-Specific or Behavioral presentations. Reflecting the unique challenges of pediatric assessment, a large subset of 49 flowcharts is deemed suitable for use with children.
The following table provides a comprehensive master list of the 53 presentational flowcharts that constitute the core of the Emergency Triage tool. The list has been compiled and cross-referenced from numerous academic studies, patient safety documents, and the official MTS handbook index.
3.2 In-Depth Analysis of Key Medical Flowcharts
While the system contains 53 flowcharts, a few key presentations account for a large volume of ED visits and represent significant clinical challenges. Analyzing these in depth reveals the system's logic and performance characteristics.
Chest Pain
Purpose and Clinical Context: The 'Chest Pain' flowchart is one of the most critical in the entire system. Its primary purpose is to rapidly identify and prioritize patients with potentially life-threatening cardiac conditions, most notably Acute Coronary Syndrome (ACS), which includes ST-elevation myocardial infarction (STEMI), non-ST-elevation myocardial infarction (NSTEMI), and unstable angina.
Discriminators and Triage Logic: The logic of the flowchart is heavily weighted towards identifying high-risk features. The discriminator for 'Cardiac pain' is designed to route patients directly to a high-priority category, typically Orange (very urgent) or, in the presence of hemodynamic compromise, Red (immediate). Other high-priority discriminators are drawn from the ABCDE framework, such as signs of circulatory shock (a 'C' problem) or severe respiratory distress (a 'B' problem). Lower-priority discriminators, which would lead to a Yellow or Green classification, include features suggestive of a non-cardiac cause, such as pleuritic pain (pain with breathing) or pain of mild intensity.
Performance and Evidence: Studies demonstrate that the 'Chest Pain' flowchart is generally effective. It shows high sensitivity in identifying high-risk cardiac patients, with one study finding that over 82% of patients with a final diagnosis of AMI were correctly triaged to a category with a target time of 10 minutes or less. Furthermore, the use of this flowchart is associated with a lower short-term mortality rate for AMI patients, suggesting it successfully identifies those who benefit from rapid intervention. However, the system is not perfect. A substantial proportion of patients with confirmed ACS—over 40% in one study—are still triaged to the lower-priority Yellow category. This indicates that patients with atypical presentations may not trigger the high-priority discriminators. This finding has led to strong clinical recommendations that a 12-lead electrocardiogram (ECG) should be performed within 10 minutes of arrival for
all patients with a presentation suggestive of ACS, regardless of their initial MTS priority level, to avoid missing time-sensitive diagnoses like STEMI.
Abdominal Pain (Adult and Pediatric)
Purpose and Clinical Context: Abdominal pain is an exceedingly common ED presentation that spans a vast diagnostic spectrum, from benign gastroenteritis to life-threatening emergencies like a ruptured aortic aneurysm or appendicitis. The 'Abdominal Pain' flowcharts for adults and children are therefore designed to stratify this diagnostically challenging and heterogeneous patient group.
Discriminators and Triage Logic: The flowchart's logic prioritizes signs of systemic illness or catastrophic intra-abdominal events. High-priority discriminators include evidence of hemodynamic instability (e.g., hypotension, tachycardia, pallor), which points to a 'Circulation' problem like haemorrhage or sepsis, and severe, unrelenting pain, which is an Orange-level discriminator. The evolution of this flowchart, documented in the official update log, provides a clear window into efforts to enhance its safety. Crucial discriminators have been added at the Orange level to explicitly screen for high-risk conditions, including
'Possible Sepsis', 'Aortic pain' (which replaced the less specific 'Pain radiating into back' to better identify aortic dissection), and, for the pediatric version, 'Testicular pain' to ensure conditions like testicular torsion are not missed in young boys who may not articulate the source of their pain clearly. Lower-priority discriminators include 'moderate pain' (Yellow) or 'mild pain' (Green/Blue).
Performance and Evidence: Despite its frequent use, the 'Abdominal Pain' flowchart demonstrates only moderate validity. One large, multicenter study found that its sensitivity for identifying high-urgency patients was below 0.5, meaning it missed more than half of the truly urgent cases as defined by the study's reference standard. This suggests that the available discriminators struggle to reliably separate high-risk from low-risk patients in this diverse population, making it one of the more challenging presentations to triage accurately with the MTS.
"Unwell Adult"
Purpose and Clinical Context: This flowchart occupies a unique and problematic space within the MTS. It is intended as a "catch-all" pathway for adult patients who present with vague, non-specific complaints such as generalized weakness, fatigue, or simply "feeling unwell," where a clear, localizing symptom is absent.
Discriminators and Triage Logic: Lacking specific symptomatic clues, this flowchart relies almost exclusively on the general discriminators (pain, consciousness, temperature, etc.) and the measurement of vital signs to determine a priority level.
Performance and Critique: The performance of the "Unwell Adult" flowchart is a major point of criticism and a recognized system vulnerability. It is one of the most frequently used flowcharts in many EDs, particularly for older adult patients. However, a compelling body of research demonstrates that it performs significantly worse than more specific flowcharts. Studies using the Area Under the Curve (AUC) to measure predictive accuracy show that the "Unwell Adult" chart is substantially less accurate at predicting hospitalization, ICU admission, and in-hospital mortality compared to patients triaged with specific charts like 'Chest Pain' or 'Head Injury'. This systematic underperformance means that patients, especially the elderly, who present with non-specific complaints are often assigned a lower triage level than their underlying condition warrants, creating a clear and present risk of undertriage and subsequent adverse outcomes. This has led researchers to label the flowchart a potential "curse" of the system. This issue represents a fundamental clash between the MTS's symptom-based design and the reality of geriatric medicine, where non-specific complaints are often a harbinger of serious illness. The system is optimized for discrete, typical problems and struggles when the "presentation" is a lack of a clear presentation. This is not merely a flaw in one flowchart but a systemic vulnerability of the entire methodology when confronted with the growing demographic of elderly, multi-morbid patients.
3.3 Analysis of Key Trauma and Specialty Flowcharts
The MTS includes a dedicated suite of flowcharts for traumatic injuries and other specific clinical scenarios, which often demonstrate different performance characteristics than the general medical charts.
Head Injury
Purpose and Clinical Context: As a core trauma flowchart, 'Head Injury' is designed to stratify patients based on the mechanism of their injury and, most importantly, their neurological status, to identify those at risk of intracranial injury.
Discriminators and Triage Logic: The logic of this flowchart is centered on the 'Disability' component of the ABCDE assessment. High-priority (Red or Orange) discriminators include a reduced or fluctuating level of consciousness (assessed using the Glasgow Coma Scale (GCS) or the simpler AVPU—Alert, Voice, Pain, Unresponsive—scale), a history of high-impact injury, active seizures following the injury, or the presence of new focal neurological deficits (e.g., one-sided weakness).
Performance and Evidence: In general, the trauma-related flowcharts within the MTS perform better than the medical flowcharts. A large study in a pediatric population found that the likelihood ratio for identifying a high-urgency patient was 12.0 for trauma presentations, compared to just 2.3 for medical presentations. This suggests that the discriminators for trauma, which are often more objective and dramatic (e.g., level of consciousness, visible injury), are more effective at risk stratification than those for medical complaints, which can be more subtle and subjective.
Pediatric-Specific Flowcharts ('Worried Parents', 'Dyspnea in Children', 'Crying Baby')
Purpose and Clinical Context: This group of flowcharts was specifically created to address presentations that are unique to children or that manifest differently in pediatric patients. They acknowledge that assessing children can be challenging due to their inability to articulate symptoms and that parental concern is often a primary driver for seeking emergency care.
Frequency of Use: The 'Worried Parents' flowchart is a standout in pediatric emergency medicine, often being the single most-used chart. In one large study, it accounted for 22.4% of all pediatric ED visits triaged with MTS. This is typically followed in frequency by 'Dyspnea in children' and 'Diarrhea and vomiting'.
Discriminators and Triage Logic: These charts use a combination of objective clinical signs and more subjective or historical factors. Objective, high-priority discriminators include 'Low O2 saturation' and 'Increased work of breathing'. More subjective or historical discriminators include 'Not fed', 'Persistent vomiting', or simply a 'Recent event' (a low-priority discriminator indicating the problem is new but not otherwise alarming).
Performance and Evidence: The overall validity of the MTS in pediatric populations is generally considered moderate. Some studies have suggested that this moderate performance may be due to a relative lack of specific flowcharts tailored to the nuances of pediatric illness compared to the adult-focused charts. The extremely high usage of the 'Worried Parents' flowchart underscores a central challenge in pediatric triage: distinguishing legitimate parental concern about a sick child from parental anxiety about a well child.
3.4 The Dynamic Nature of the Flowcharts: An Evolving System
A critical feature of the Manchester Triage System is that it is not a static set of rules. It is a dynamic, "living" system that is subject to ongoing review and evidence-based updates managed by the International Reference Group. This commitment to continuous improvement ensures the system remains clinically relevant and incorporates new knowledge about patient safety risks.
The official MTS update log provides concrete evidence of this evolutionary process, serving as a historical record of emerging patient safety priorities in emergency medicine. Analysis of these updates reveals a clear pattern of reactive improvements designed to address known system weaknesses or changing epidemiological trends:
Improving Sepsis Recognition: In 2016, a major update involved adding the discriminator 'Possible Sepsis' to the Orange (very urgent) category across multiple relevant flowcharts, including 'Abdominal pain' (both adult and child) and 'Abscesses and local infections'. This change directly reflects the global clinical emphasis on early recognition and intervention for sepsis.
Targeting Aortic Dissection: In 2020, the 'Abdominal pain in adults' flowchart was updated to replace the vague discriminator 'Pain radiating into back' with the much more specific and high-risk discriminator 'Aortic pain'. This was a deliberate change to improve the early identification of patients with potential aortic dissection, a frequently missed and highly lethal diagnosis.
Enhancing Mental Health Triage: In 2021, a review of mental health presentations led to significant updates in the 'Abuse and neglect' and 'Apparently drunk' flowcharts. Vague discriminators were replaced with more precise language to better stratify the immediate risks of self-harm, violence towards others, and the need for restraint.
Expanding Applicability: The flowchart originally named 'Abused and neglected child' was renamed to the more inclusive 'Abuse and neglect'. This seemingly minor change had a significant practical impact, making the flowchart applicable to vulnerable adults as well as children, thereby expanding its utility.
This continuous evolution demonstrates that the flowcharts are not just static algorithms but a reflection of the emergency medicine community's growing understanding of clinical risk. Analyzing their changes over time provides a clear timeline of what have been identified as the most pressing areas of missed diagnoses or emerging patient safety threats.
Evidence in Practice: Validity, Reliability, and Performance
The theoretical elegance of a triage system is meaningless without empirical evidence of its performance in the complex and unpredictable environment of a real-world emergency department. The Manchester Triage System has been the subject of extensive academic research aimed at evaluating its core performance characteristics: reliability (consistency) and validity (accuracy). This section critically synthesizes this body of evidence, examining how the MTS performs overall, in vulnerable patient populations, and in the context of its inherent tendency towards overtriage and undertriage.
4.1 System Reliability: Is the Assessment Consistent?
Reliability, in the context of triage, refers to the consistency and reproducibility of the assessment. It addresses the question of whether the system yields the same result when applied to the same patient by different assessors (inter-rater reliability) or by the same assessor at different times (intra-rater reliability). A reliable system is crucial for ensuring that triage decisions are standardized and not dependent on the random chance of which nurse is on duty.
Overall, systematic reviews and meta-analyses conclude that the MTS demonstrates a moderate to substantial level of reliability. The most common statistical measure used is the kappa coefficient (k), which quantifies the level of agreement beyond what would be expected by chance. Pooled kappa coefficients for MTS are frequently reported in the range of 0.55 to 0.78, indicating a level of agreement that is clinically acceptable, though not perfect. One meta-analysis calculated a pooled coefficient of 0.751, which is considered "substantial" agreement.
However, this overall reliability is not uniform and is influenced by several key factors:
The Power of the Discriminator: A crucial finding for the system's internal logic is that the correct choice of the discriminator has a far greater impact on achieving the correct final priority level than the choice of the flowchart. This provides strong evidence for the safety of the system's design principle that a given discriminator leads to the same priority level regardless of the flowchart. It means that even if two nurses choose different but plausible flowcharts for a complex presentation, they are likely to arrive at the same, safe priority level if they identify the same critical sign or symptom.
The Influence of Nurse Experience: Reliability is not an inherent property of the tool alone but is significantly mediated by the user's expertise. Studies consistently show that reliability is higher among nurses with more years of professional experience, particularly in emergency care and risk classification settings. Nurses with one to ten years of experience tend to demonstrate the highest levels of agreement with both their peers and an established gold standard.
Geographic and Cultural Factors: Intriguingly, one meta-analysis discovered that inter-rater reliability was higher in studies conducted in the United Kingdom and countries in close geographic proximity. This suggests that factors such as the fidelity of the initial training, cultural adaptation of the tool, and ongoing educational support may play a significant role in maintaining high levels of consistency.
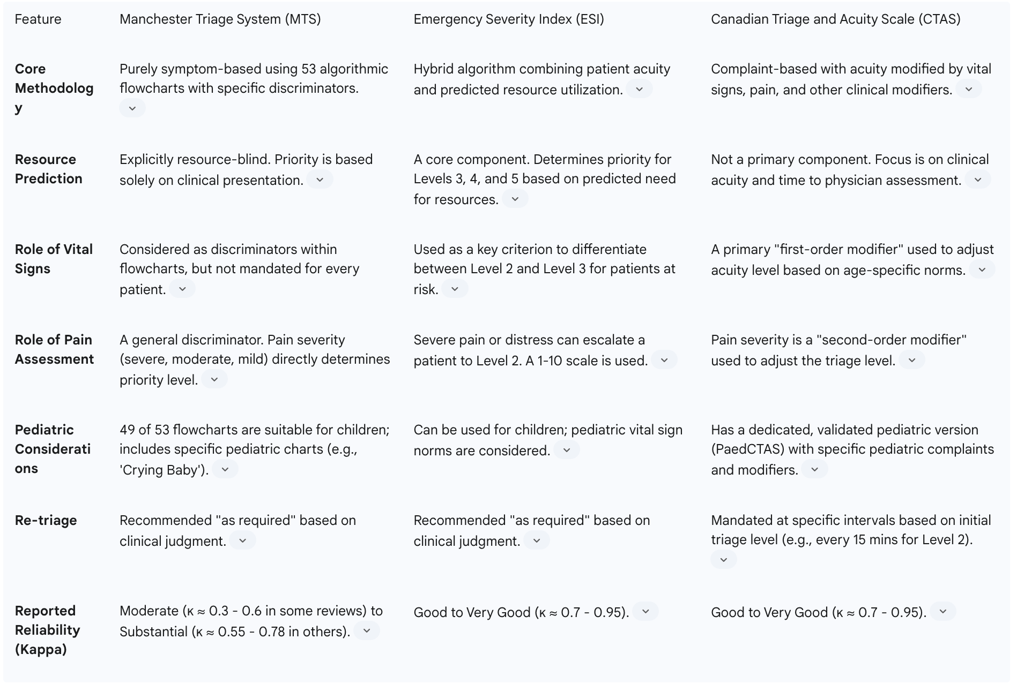
When compared to other major triage systems, the evidence on reliability is mixed. Some systematic reviews have concluded that the reliability of MTS (with reported kappa statistics in the range of 0.3 to 0.6) is only "moderate" and may be lower than the "good to very good" reliability (kappa > 0.7) reported for the Emergency Severity Index (ESI) and the Canadian Triage and Acuity Scale (CTAS).
4.2 System Validity: Is the Assessment Correct?
Validity addresses a more fundamental question: does the MTS accurately measure a patient's true clinical urgency and correctly stratify them according to risk?. Because there is no single, perfect "gold standard" for clinical urgency, validity is assessed by comparing the MTS priority level against a range of objective proxy outcomes, such as the need for hospital admission, admission to an Intensive Care Unit (ICU), and short-term mortality.
The consensus from a large body of research is that the MTS has moderate to good validity. It has been consistently shown to be a good predictor of key patient outcomes, with higher MTS priority levels strongly correlating with a higher likelihood of hospitalization and mortality.
However, this "moderate to good" rating masks a much more complex and variable performance profile. A closer look at the data reveals that the system's validity is not uniform across all patients, presentations, or settings. One of the most striking findings from a large, multicenter study was the "considerable variation" in performance between different hospitals. The Diagnostic Odds Ratio, a single metric of test performance, was found to vary by a factor of two to three between institutions, even within the same country. This suggests that local factors—such as patient population acuity, nurse training, and adherence to the protocol—have a profound impact on how well the system works in practice. This implies that a healthcare organization cannot simply implement the MTS and assume it will be valid; its performance must be actively and locally audited.
The system's performance in predicting the most severe outcomes is a key area of concern. While overall sensitivity for identifying high-urgency patients (defined by ICU admission or death) is moderate to good, ranging from 0.58 to 0.88 in adults, critical failures still occur. A landmark multicenter study found that the MTS still misclassified 14% to 20% of adults and 9% to 34% of children who ultimately required ICU admission into a low-urgency category, potentially delaying their care. This highlights that while the system is generally safe, it is not infallible.
When compared to other scoring systems, the MTS shows distinct strengths and weaknesses. For instance, studies comparing MTS to the National Early Warning Score (NEWS) found that MTS was a superior predictor of the need for hospitalization and ICU admission. However, NEWS, which is based purely on vital signs, was a better predictor of 30-day mortality. This suggests that MTS is better at capturing the immediate need for hospital-level intervention, while NEWS may be better at identifying underlying physiological derangement that predicts longer-term outcomes.
4.3 The Challenge of Overtriage and Undertriage
The concepts of overtriage and undertriage are central to any evaluation of a triage system's validity and safety. They represent the two types of classification error, each with different consequences.
Overtriage (A Failure of Efficiency): This occurs when a patient is assigned a higher priority level than their clinical condition warrants. The MTS has a well-documented and pronounced tendency towards overtriage. In some pediatric studies, overtriage rates have been reported to be as high as 40-54%. This is not an accidental flaw but a direct and predictable consequence of the system's risk-averse, reductive methodology, which is designed to be "inclusive" and err on the side of caution. While this protects patients from being missed, it comes at a significant operational cost, leading to the inefficient use of ED resources, as less urgent patients may be prioritized for beds and investigations over others.
Undertriage (A Failure of Safety): This occurs when a patient is assigned a lower priority level than is appropriate for their condition. Although less common than overtriage in the MTS, undertriage is a far more serious patient safety concern, as it can lead to dangerous delays in assessment and treatment. Some systematic reviews have cited the rate of undertriage as a key reason for describing the system's overall safety as "low," despite its other strengths. Undertriage is known to be more likely in specific high-risk groups, such as infants and any child triaged using the 'unwell child' flowchart.
The persistent dichotomy of high overtriage and low-but-significant undertriage represents a core philosophical and economic conflict in emergency care. These are not two separate metrics but two sides of the same coin, reflecting a fundamental trade-off. The MTS is explicitly designed to accept high overtriage (economic inefficiency) in order to minimize undertriage (clinical risk). Criticisms of its high overtriage rate are, in effect, criticisms of this foundational principle. This has major implications for healthcare systems under intense financial pressure, which must decide which type of error they are more willing to tolerate.
4.4 Performance in Vulnerable Populations: The Young and the Elderly
A powerful and consistent theme that emerges from the highest-quality, large-scale research is that the validity of the Manchester Triage System is systematically lower in the most vulnerable patient populations: young children and the elderly.
Elderly Patients (≥65 years): The system's ability to accurately predict adverse outcomes diminishes significantly in older adults. This is particularly true for elderly patients who present with the non-specific complaints that lead to the use of the "Unwell adult" flowchart. The atypical presentation of serious disease (e.g., "silent" heart attacks), the confounding effects of multiple comorbidities, and altered physiological responses in the elderly all challenge a triage system that is heavily reliant on typical symptom patterns.
Pediatric Patients: The validity of MTS in children is consistently rated as moderate. This is attributed in part to the inherent challenges of pediatric assessment, such as communication difficulties and the subjective nature of caregiver reports. The system demonstrates lower specificity in children compared to adults, contributing to high rates of overtriage. While some pediatric-specific flowcharts exist (e.g., 'Crying Baby', 'Worried Parent'), the evidence suggests that the overall framework may not be sufficiently nuanced to capture the full spectrum of pediatric emergency presentations, leading to classification errors.
Critical Appraisal and Systemic Limitations
While the Manchester Triage System provides a structured and largely reliable framework, it is not without significant limitations. A critical appraisal reveals challenges that stem from the interplay of human factors, the system's core philosophical choices, and its inherent structural constraints. Understanding these limitations is essential for any organization seeking to implement the MTS safely and effectively.
5.1 Human Factors and Implementation Fidelity
Despite its algorithmic design, the MTS is not an automated process; it is a tool wielded by a human practitioner, and its effectiveness is therefore subject to human factors.
Error Under Pressure: Triage is a high-stakes, time-pressured activity. Triage nurses must make rapid decisions in a distracting environment, which can increase the likelihood of cognitive errors and misclassification, even within a standardized system.
The Role of Cognitive Bias: The system's structure is intended to minimize subjectivity, but it cannot eliminate it entirely. Unconscious biases, personal judgments, and heuristics can still influence a nurse's decisions. For example, the MTS places a high value on pain as a discriminator, but pain assessment is notoriously subjective. A nurse's interpretation of a patient's pain score can lead to significant variability in the final triage category.
Training and Protocol Adherence: The fidelity of implementation is paramount. The system's performance degrades significantly if practitioners are not adequately trained or do not adhere to the protocol. For example, one study found that nurses often failed to perform pain assessments as required by the guidelines, sometimes because of a belief that doing so would automatically lead to overtriage. This demonstrates a breakdown in both education and adherence, where practitioners begin to "game" the system based on their own perceptions rather than following the prescribed methodology.
5.2 The Deliberate Omission of Resource Constraints
One of the most defining—and debated—features of the MTS is its philosophical purity in separating clinical priority from operational considerations.
An Absolute Clinical Priority: The Manchester Triage Group's philosophy is resolute: the triage priority (the color assigned) is an absolute clinical indicator based solely on the patient's presentation. It should never be altered or influenced by the current state of the department, such as how busy it is or what resources are available.
A Key Distinction from ESI: This stance creates a clear dividing line between MTS and other systems like the Emergency Severity Index (ESI). The ESI algorithm explicitly requires the triage nurse to predict the patient's anticipated resource needs (e.g., number of tests, procedures, consultations) to assign a priority level for less acute patients. MTS is, by design,
resource-blind.
The Practical Consequence: While this approach maintains the integrity of the clinical assessment, it creates a significant practical limitation. The MTS is excellent at identifying who is sickest, but it offers no inherent mechanism to help manage the subsequent patient flow or predict the overall departmental workload. This can lead to significant bottlenecks, as the system may generate a large queue of high-priority patients without providing the tools to manage that queue. This "resource-blind" philosophy places the entire burden of managing patient flow and departmental capacity on separate, downstream processes and personnel (e.g., a charge nurse or flow coordinator). It creates a potential disconnect in hospital operations, where the critical data gathered at triage is not fully translated into actionable information for managing departmental load.
5.3 The Inadequacy for Non-Specific and Atypical Complaints
The architectural design of the MTS, built upon specific presentational flowcharts, creates a systemic vulnerability when faced with patients who do not present with a "typical" complaint.
The "Unwell Adult" Weakness: As detailed previously, the system's performance falters significantly when dealing with the non-specific complaints funneled into the "Unwell Adult" flowchart. The system's reliance on "typical case presentation" is a major concern, as it leads to the under-prioritization of seriously ill older patients who often present with vague symptoms like generalized weakness or confusion.
Atypical Presentations of Serious Disease: The symptom-based nature of the flowcharts means that a patient with a life-threatening condition, such as an acute coronary syndrome or a pulmonary embolism, may be assigned a low priority if they present with atypical symptoms (e.g., epigastric pain or syncope instead of classic chest pain). The system is powerful and precise for its intended targets (typical presentations) but can be brittle and prone to failure when faced with unexpected or ambiguous clinical pictures. It is excellent at finding the "needle" in the haystack if the patient reports a sharp prick, but it struggles to identify risk when the patient just reports a general sense of being "in the haystack."
5.4 Stagnation and the Pace of Updates
A broad criticism that has been leveled against all major, established triage systems, including the MTS, is that they can be slow to evolve. Critics argue that these systems sometimes undergo only minimal substantial updates, causing them to lag behind the advancing body of scientific evidence in emergency medicine.
While this is a valid general concern for any standardized protocol, the evidence specific to the MTS suggests a more nuanced picture. The existence of a formal governance structure, the Manchester Triage Group, and its International Reference Group, provides a clear mechanism for continuous, evidence-based review and updates. The detailed update log, which shows specific changes made in response to emerging patient safety concerns like sepsis and aortic dissection, serves as counter-evidence to the idea that the system is entirely static. Therefore, the greater risk may not lie with a lack of updates from the governing body, but rather with individual healthcare organizations failing to implement the latest, safest version of the tool. A patient safety alert from the Royal College of Emergency Medicine highlighted this very issue, warning of the dangers posed by hospitals continuing to use outdated versions of the MTS with obsolete parameters for critical conditions.
The Global Context: MTS in Relation to Other Triage Systems
The Manchester Triage System does not exist in a vacuum. It is one of several major triage systems used in emergency departments around the world. Situating the MTS within this international landscape, particularly in comparison to its main counterparts—the Emergency Severity Index (ESI) and the Canadian Triage and Acuity Scale (CTAS)—is essential for understanding its unique methodological approach, philosophical underpinnings, and relative strengths and weaknesses.
6.1 The "Big Four" Five-Level Triage Systems
Over the past three decades, a global consensus has emerged that a five-level acuity scale is the most effective framework for emergency triage. These systems have demonstrated superior validity and reliability compared to older, simpler three-level systems. Within this five-level paradigm, four systems have achieved widespread international recognition and have been the subject of extensive study:
The Manchester Triage System (MTS): Developed in the UK and widely used across Europe, Brazil, and Australia.
The Emergency Severity Index (ESI): Developed in the USA and the predominant system used in North America.
The Canadian Triage and Acuity Scale (CTAS): Developed in Canada and the national standard there, with a strong evidence base.
The Australasian Triage Scale (ATS): Developed and used in Australia and New Zealand, and the progenitor of the CTAS.
6.2 Comparative Methodological Analysis
The core difference between these systems lies not in their five-level structure, but in the methodology and logic used to arrive at a priority level.
Manchester Triage System (MTS): The methodology of the MTS is purely symptom-based and highly algorithmic. The process begins with the nurse selecting one of 53 presentational flowcharts that best matches the patient's chief complaint. The nurse then follows a reductive, hierarchical process, checking for the presence of specific "discriminators" from the highest priority (Red) downwards. The first positive discriminator found determines the patient's triage category. The system's defining feature is its highly structured nature, designed to maximize consistency and minimize subjective interpretation. It is explicitly and philosophically resource-blind.
Emergency Severity Index (ESI): The ESI employs a unique hybrid algorithm that explicitly combines the assessment of patient acuity with a prediction of necessary resource utilization. The algorithm poses a series of four decision points. The first two quickly identify high-acuity patients (Level 1: Is the patient dying? Level 2: Is this a high-risk situation or is the patient confused/lethargic/disoriented, or in severe pain/distress?). If the patient does not meet Level 1 or 2 criteria, their final priority level (3, 4, or 5) is determined by the number of different resources (e.g., lab tests, ECG, imaging, IV fluids, specialty consultation) the triage nurse predicts the patient will require to reach a disposition decision.
Canadian Triage and Acuity Scale (CTAS): The CTAS, which evolved from the ATS, uses a comprehensive list of presenting complaints and symptoms, combined with physiological modifiers. The triage nurse considers the patient's primary complaint, but also modifies the acuity level based on vital signs, level of consciousness, pain severity, and mechanism of injury. A key feature of CTAS is its rigorously defined and research-validated time objectives for physician assessment and, critically, its mandatory
re-triage intervals for patients left waiting in the department. It also has a well-developed and validated pediatric version, PaedCTAS.
6.3 Performance Comparison: Reliability and Validity
Direct comparisons of the systems' performance reveal different strengths and weaknesses.
Reliability: Some systematic reviews have drawn a distinction in the reported reliability of the systems. These reviews often conclude that CTAS and ESI demonstrate "good to very good" reliability, with kappa coefficients frequently above 0.7. In contrast, these same reviews sometimes categorize MTS as having only "moderate" reliability, with kappa values reported in the 0.3 to 0.6 range. This could suggest that the more rigid, flowchart-driven nature of MTS does not eliminate inter-rater variability as much as intended, or that the other systems' frameworks lead to more consistent application in some research settings.
Validity: When it comes to validity, the picture is less clear, with performance often being highly variable and context-dependent.
High-Urgency Patients: In studies comparing the systems' ability to identify high-urgency patients (as defined by ICU admission), no single system emerges as clearly superior. MTS, ESI, and CTAS all demonstrate moderate to good sensitivity, but all exhibit wide variability in performance across different studies and settings.
Low-Urgency Patients: Similarly, when assessing the ability to correctly identify low-urgency patients (those ultimately discharged home), none of the systems shows a markedly better specificity than the others. Again, high variability within each system is the dominant finding.
A Practical Example in Trauma: A direct comparison of MTS and ESI in a trauma patient population offered a revealing practical insight. The study found that ESI triaged a significantly higher percentage of patients to Level 3 (70%) compared to MTS (34%). This was attributed to ESI's resource prediction component; many minor trauma patients who were stable (and thus a lower priority in MTS) required resources like X-rays, automatically escalating them to ESI Level 3. A key outcome was that the mean length of stay in the ED was significantly shorter for the group triaged with MTS. This suggests that ESI's focus on resources may lead to ED congestion by pulling less acute patients into higher-priority streams, whereas MTS's purely clinical focus may facilitate faster disposition for minor cases.
The choice between MTS and ESI, therefore, represents a strategic decision that reflects a hospital's core operational priority. An organization that prioritizes creating a highly standardized, auditable, and consistent clinical assessment may favor the rigid, flowchart-driven MTS. Conversely, an organization whose primary challenge is managing patient flow, predicting departmental load, and aligning clinical priority with operational throughput may find the integrated resource prediction of ESI more advantageous. The "better" system is not an absolute; it depends entirely on the specific problem the healthcare organization is trying to solve.
This divergence also reflects the different healthcare systems in which these tools were conceived. The MTS, born from the UK's National Health Service, mirrors a culture of standardized national protocols and clinical governance. The ESI, developed in the United States, reflects a system where hospital efficiency and resource management are critical financial and operational drivers. The CTAS, driven by Canadian national bodies, emphasizes national standards for training and continuous quality monitoring through re-triage. This suggests that the international triage landscape is unlikely to converge on a single "best" system. Instead, the choice of a triage tool will likely remain a process of finding the best philosophical and operational fit for a given local or national healthcare context.
Table 2: Comparative Analysis of Major Triage Systems (MTS, ESI, CTAS)
Governance, Evolution, and Recommendations
The Manchester Triage System is more than a static set of documents; it is a dynamic and governed clinical tool that continues to evolve. Its long-term safety and efficacy are contingent on a robust governance structure, a commitment to continuous improvement, and diligent implementation by healthcare organizations. This final section examines the governance framework of the MTS, its expansion into a wider ecosystem of related tools, and provides evidence-based recommendations for its quality assurance and safe application in practice.
7.1 The Manchester Triage Group and International Governance
Unlike some clinical tools that are developed and then left to be used as-is, the MTS is actively managed and maintained. This governance is a key feature that underpins its claim as a standardized system.
A Governed System: The MTS is overseen by the Manchester Triage Group (MTG) in the UK and a broader International Reference Group. This international body is composed of representatives from all countries that have officially adopted and translated the system, ensuring a global perspective on its application and development.
Continuous, Evidence-Based Improvement: This governance structure is not merely administrative; its primary function is to facilitate the continuous improvement of the system. The group convenes for annual international conferences where new research is presented and changes to the system are debated and agreed upon based on emerging clinical evidence and patient safety data. This process ensures that the MTS remains a living tool that adapts to the changing landscape of emergency medicine.
The Critical Importance of Version Control: The evolutionary nature of the MTS means that multiple versions exist. The 3rd Edition of the core handbook, for example, has been updated to Version 3.8 as of 2023. This makes it absolutely critical for healthcare organizations to ensure they are using the most current, supported version. The Royal College of Emergency Medicine has issued a formal patient safety alert regarding this very issue, highlighting that organizations using outdated versions of the MTS are operating with obsolete clinical parameters for time-sensitive conditions like sepsis, which could directly and negatively affect patient outcomes. This underscores that the MTS should not be viewed as a one-time purchase or implementation, but as an ongoing subscription to a clinical safety service. Its efficacy is contingent on an organization's engagement with the governance and update ecosystem.
7.2 The MTS Ecosystem: Beyond the Emergency Department
Recognizing that the need for standardized risk assessment extends beyond the hospital's front door, the core principles of the MTS have been systematically adapted into an integrated suite of tools for various clinical settings. This "MTS ecosystem" aims to create a common language and a consistent approach to triage across the entire urgent and emergency care pathway.
The key adaptations include:
Telephone Triage and Advice: This tool uses the same reductive methodology, flowchart structure, and discriminator definitions as the ED version but is adapted for remote assessment over the telephone. It is widely used by urgent care desks and ambulance service call centers.
Prehospital Pathfinder: This is a risk assessment tool specifically designed for paramedics and other ambulance clinicians to use during face-to-face patient contact in the prehospital environment.
Nursing and Residential Triage (NaRT): This is a simplified version of the MTS designed for staff working in nursing and residential homes. Recognizing the different scope of practice in this setting, the NaRT condenses the 53 ED flowcharts into just two overarching charts: 'Illness' and 'Injury'.
Community Triage Tool (CoTT) / SAFE pathways: These tools are designed for other community-based healthcare professionals, first responder organizations, and telecare providers, again using the core MTS principles to guide assessment and disposition decisions.
The development of this ecosystem represents a sophisticated strategy to standardize the language and logic of clinical risk assessment across multiple points of patient contact. When a telephone operator using Telephone Triage, a paramedic using Prehospital Pathfinder, and an ED nurse using Emergency Triage are all working from the same foundational principles, the potential for information to be "lost in translation" during patient handoffs is significantly reduced. This creates a powerful network effect, hardwiring consistency not just within the walls of the ED, but across the patient's entire unscheduled care journey.
7.3 Recommendations for Implementation and Quality Assurance
The evidence clearly indicates that the safe and effective use of the Manchester Triage System is dependent on diligent and systematic implementation and ongoing quality assurance. Based on the findings of numerous studies and the guidance of the MTG itself, the following recommendations are essential for any organization using or planning to use the MTS:
Ensure Version Control: Organizations must have a formal process to ensure they are always using the most current, officially supported version of the MTS and all its associated tools. Using outdated versions introduces known patient safety risks.
Mandate Robust Training and Credentialing: All practitioners assigned to triage must be registered HCPs. They must complete a comprehensive, standardized training program on MTS methodology before they begin triaging patients. This training must cover the reductive philosophy, the correct use of all relevant flowcharts, and the precise definitions in the discriminator dictionary. Competency should be assessed and periodically re-validated.
Implement a Structured Audit Program: The MTS is explicitly designed to be auditable, and this feature must be utilized. Organizations should implement a regular, structured audit program as defined by the MTG. This involves reviewing a set sample of triage records (e.g., 2% of all cases or a minimum of 10 per user) against the system's standards to identify deviations, provide feedback to staff, and monitor system performance.
Conduct Local Validity Monitoring: Given the well-documented variability in MTS performance across different settings, organizations should not assume the system is valid in their specific context. They should conduct local monitoring of the system's validity, paying particularly close attention to its performance in high-risk and vulnerable populations (e.g., the elderly, infants) and for challenging presentations (e.g., "Unwell Adult," "Abdominal Pain").
Guarantee High-Fidelity Software Implementation: When integrating the MTS into a Hospital Information System (HIS) or Electronic Health Record (EHR), it is critical to ensure the software implementation is correct. The MTG provides licensed software companies with a detailed map to ensure that the hierarchical order of discriminators within each flowchart is preserved and that risk limits are displayed correctly. Deviations in the software build can compromise the system's logic and safety.
Conclusions
The Manchester Triage System has established itself as a cornerstone of modern emergency care, providing a structured, risk-averse, and auditable methodology for patient prioritization. Its development marked a pivotal transition away from inconsistent, intuitive triage towards a standardized, evidence-informed process. The system's core strengths lie in its reductive philosophy, which prioritizes safety by assuming the highest level of risk until proven otherwise, and its presentation-based flowcharts, which create a common language and a consistent approach to clinical assessment across practitioners and institutions.
However, this comprehensive analysis reveals that the MTS is a tool with a distinct and complex performance profile, characterized by inherent trade-offs. Its greatest strength—the risk-averse design that promotes patient safety—is inextricably linked to its most significant operational weakness: a high rate of overtriage that can lead to inefficient resource allocation. The system's algorithmic, flowchart-driven structure, while excellent for standardizing the assessment of typical clinical presentations, demonstrates significant vulnerabilities when faced with the atypical or non-specific complaints that are increasingly common in elderly and multi-morbid patient populations. This results in a well-documented and concerning pattern of underperformance and potential undertriage in these vulnerable groups.
Furthermore, the validity and reliability of the MTS, while generally rated as moderate to good, are not absolute. Performance varies considerably depending on the clinical setting, the specific presenting complaint, and the experience level of the triage nurse. This underscores that the MTS is not a "fire-and-forget" solution. Its safety and effectiveness are not guaranteed by simple adoption but are contingent upon an organization's deep commitment to a continuous cycle of quality assurance.
Therefore, the following conclusions and recommendations are paramount for any healthcare leader, educator, or policymaker involved with the Manchester Triage System:
MTS is a System, Not Just a Tool: The MTS should be viewed not as a standalone product but as an integrated clinical risk management system. Its successful implementation requires ongoing engagement with the entire ecosystem, including mandatory use of the latest version, robust and continuous training, a structured audit program, and high-fidelity integration into clinical software.
Acknowledge the Safety-Efficiency Trade-Off: Organizations choosing the MTS must explicitly acknowledge and accept its inherent philosophical bias towards clinical safety at the cost of operational efficiency (i.e., high overtriage). Strategies to manage the downstream effects of overtriage on patient flow and resource use must be developed in parallel.
Targeted Monitoring for High-Risk Scenarios: Given the evidence of underperformance, organizations must implement targeted quality monitoring and supplementary protocols for high-risk populations (infants and the elderly) and for patients triaged with non-specific flowcharts like "Unwell Adult." Reliance on the standard MTS algorithm alone for these patients is insufficient to guarantee safety.
Embrace the Broader Ecosystem: The expansion of MTS into prehospital, telephone, and community settings offers a powerful opportunity to standardize risk assessment across the entire patient journey. Healthcare systems should look to leverage this ecosystem to improve communication and safety at the interfaces of care.
Ultimately, the Manchester Triage System is a powerful and essential instrument for managing risk in the modern emergency department. Yet, like any complex clinical tool, its potential can only be fully realized when its limitations are understood, its performance is actively monitored, and its application is supported by a robust culture of safety, training, and continuous quality improvement.
FAQ Section:
Q1: What is the Manchester Triage System (MTS)?
The Manchester Triage System (MTS) is a widely used system for determining priority based on urgency, primarily in emergency departments globally. It includes 52 flowcharts with specific and general discriminators and is known for its high interrater reliability and widespread implementation.
Q2: How does the Emergency Severity Index (ESI) differ from the Manchester Triage System (MTS)?
The Emergency Severity Index (ESI) focuses on predicting resource needs and acuity, while the Manchester Triage System (MTS) emphasizes time-to-treatment and specific discriminators. The ESI is widely used in the U.S. and is a strong predictor of admission and mortality, but it may have higher undertriage rates compared to the MTS.
Q3: What are the key features of the Canadian Triage and Acuity Scale (CTAS)?
The Canadian Triage and Acuity Scale (CTAS) is well-validated in Canada and internationally. It focuses on time-to-treatment and clinical judgment, with 5 levels based on the severity of the illness or time needed before medical intervention combined with a standardized presenting patient complaint list.
Q4: How is the Australasian Triage Scale (ATS) structured?
The Australasian Triage Scale (ATS) is a 5-level system used in Australia and New Zealand. It focuses on presenting complaints and clinical signs, with categories based on the severity of the illness or time needed before medical intervention. The ATS is well-validated in Australasia and is known for its simple structure and suitability for emergency departments.
Q5: What makes the South African Triage Scale (SATS) unique?
The South African Triage Scale (SATS) is designed for low-resource settings and uses color-coded categories and physiological parameters. It is validated in resource-limited settings and is known for its simplicity and effectiveness in handling high patient volumes with limited resources.
Q6: What are the benefits of the Rapid Emergency Triage and Treatment System (RETTS)?
The Rapid Emergency Triage and Treatment System (RETTS) integrates physiological parameters with symptom-based algorithms, providing a comprehensive assessment tool. It is used primarily in Sweden and is known for its high specificity and effectiveness in emergency assessments.
Q7: How does the sensitivity and specificity of these triage systems compare?
The sensitivity and specificity of these triage systems vary. The Emergency Severity Index (ESI) has higher sensitivity for resource-intensive cases, while the Manchester Triage System (MTS) has high specificity across urgency levels. The Canadian Triage and Acuity Scale (CTAS) and Australasian Triage Scale (ATS) also have high specificity, and the South African Triage Scale (SATS) is known for its high specificity in low-resource settings.
Q8: What are the limitations of the Emergency Severity Index (ESI)?
The Emergency Severity Index (ESI) has higher undertriage rates compared to the Manchester Triage System (MTS) and may require more complex clinical training. It is widely used in the U.S. and is a strong predictor of admission and mortality, but its complexity and higher undertriage rates can be challenging.
Q9: How is the Canadian Triage and Acuity Scale (CTAS) validated?
The Canadian Triage and Acuity Scale (CTAS) is well-validated in Canada and internationally. It is known for its strong focus on time-to-treatment and clinical judgment, with 5 levels based on the severity of the illness or time needed before medical intervention combined with a standardized presenting patient complaint list.
Q10: What are the strengths of the Australasian Triage Scale (ATS)?
The Australasian Triage Scale (ATS) is well-validated in Australasia, with a simple structure well-suited for emergency departments. It focuses on presenting complaints and clinical signs, with categories based on the severity of the illness or time needed before medical intervention.
