The Future of Triage in Emergency Healthcare Response to Global Health Threats
This report outlines a strategic imperative for investing in AI to cultivate more resilient, responsive, and equitable emergency healthcare systems globally, positioning AI as an indispensable catalyst for future pandemic preparedness and crisis management.


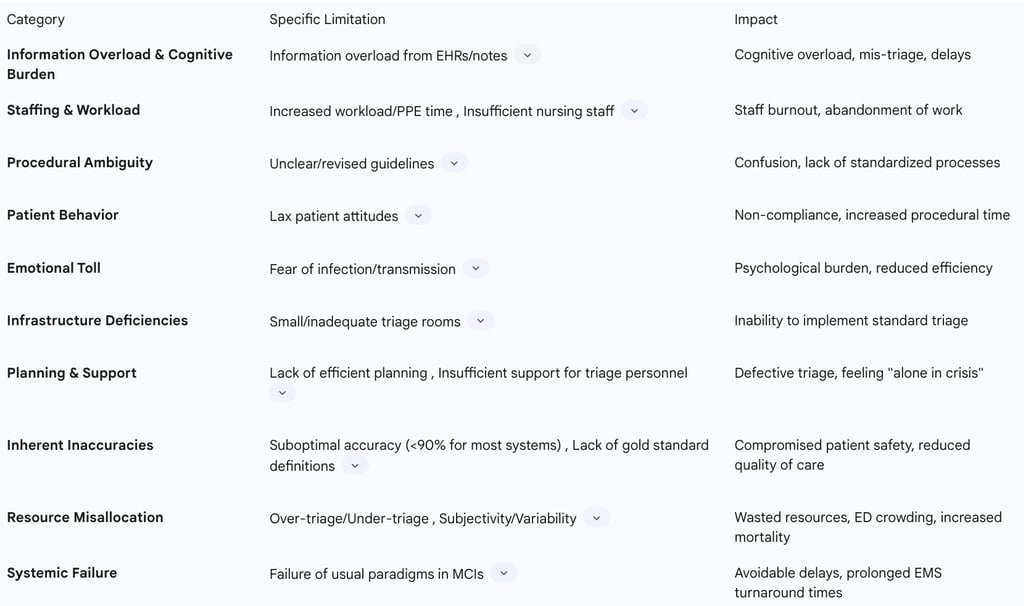
The landscape of global health is increasingly defined by the emergence of novel threats, from rapidly spreading infectious diseases to large-scale mass casualty incidents. In this evolving environment, the efficacy of emergency healthcare response hinges critically on robust and adaptive triage systems. Traditional triage methodologies, however, are demonstrably strained, exhibiting significant limitations when confronted with the immense pressures of these crises. These include overwhelming information overload, profound staffing shortages, inherent subjectivity in decision-making, and a reactive operational paradigm that struggles to keep pace with dynamic patient flows.
Artificial Intelligence (AI) presents a compelling and multifaceted solution to these systemic vulnerabilities. By integrating advanced machine learning for precise patient acuity prediction, leveraging natural language processing for comprehensive unstructured data interpretation, and employing predictive analytics for dynamic operational optimization, AI can fundamentally transform emergency triage. Early pilot programs and systematic reviews demonstrate AI's capacity to significantly enhance diagnostic accuracy, reduce mis-triage rates, streamline workflows, and optimize resource allocation, thereby improving patient outcomes and alleviating clinician burden.
However, the widespread adoption of AI in emergency healthcare is not without its complexities. Critical ethical considerations, including algorithmic bias, data privacy, and the imperative for transparency and accountability, must be meticulously addressed. Furthermore, the evolving regulatory landscape demands rigorous validation and clear guidelines for AI-enabled medical devices. Responsible and equitable AI deployment necessitates a collaborative, multi-stakeholder approach involving healthcare providers, technology developers, policymakers, and regulators. This report outlines a strategic imperative for investing in AI to cultivate more resilient, responsive, and equitable emergency healthcare systems globally, positioning AI as an indispensable catalyst for future pandemic preparedness and crisis management.
II. The Imperative for Transformation: Limitations of Current Triage Systems
The escalating frequency and complexity of global health threats underscore a critical need for fundamental transformation within emergency healthcare triage. Current methodologies, largely reliant on human judgment and traditional processes, exhibit systemic vulnerabilities and operational inefficiencies that are acutely exposed during large-scale health crises and contribute significantly to everyday emergency department (ED) overcrowding.
Challenges in Large-Scale Health Crises and Pandemics
Emergency departments, serving as the frontline during health crises, face immense pressure. Traditional decision-making in these settings heavily relies on the experience of individual clinicians, a method that struggles profoundly with the overwhelming volume of information generated by Electronic Health Records (EHRs) and unstructured clinical notes. This leads to significant cognitive overload, hindering efficient and accurate triage, especially when rapid decisions are paramount during large-scale events. The combination of this cognitive burden, coupled with the emotional distress and physical demands inherent in crisis environments, directly compromises the accuracy, consistency, and safety of triage decisions. This is not merely an issue of inefficiency; it represents a systemic vulnerability where inherent human limitations are amplified by crisis conditions, leading to widespread mis-triage, avoidable delays in care, and potentially adverse patient outcomes. The system can enter a negative feedback loop where overcrowding and staff burnout worsen triage quality, further intensifying the crisis and diminishing the overall emergency response capacity.
Pandemics, such as the COVID-19 outbreak, have dramatically increased the information required for patient assessment and the procedural steps involved in triage. The necessity of donning and doffing Personal Protective Equipment (PPE) further prolongs the time needed for each patient, imposing an overwhelming workload on triage nurses. These professionals often find themselves solely responsible for critical decisions, such as patient isolation and managing negative pressure room availability, without adequate support. Additionally, during public health crises, guidelines are frequently established and repeatedly revised in response to emerging pathogens or new mutations. This constant flux in protocols can cause significant confusion and skepticism among healthcare professionals, undermining the clarity and transparency of infection control systems and impeding standardized, efficient triage processes.
Compounding these challenges, patient cooperation during history taking can decline as crises prolong, and their adherence to infectious disease protocols may become lax. Discrepancies between government and hospital infection control guidelines further complicate the triage process, requiring nurses to ensure both patients and their caregivers comprehend and comply with hospital-specific requirements. The profound emotional and psychological burden on triage nurses, stemming from the fear of infection and potential transmission to family members, particularly in the early stages of an unfamiliar outbreak, contributes significantly to staff burnout and, in severe cases, abandonment of work. Furthermore, Mass Casualty Incidents (MCIs) and pandemics frequently overwhelm available resources, causing traditional triage and treatment paradigms to fail. Many hospitals lack sufficient training or experience in triaging exceptionally large numbers of patients, leading to mis-triage and avoidable delays in care. This challenge is exacerbated by inadequate physical infrastructure, such as small triage rooms, a lack of windows, and distant laboratory and radiology units. The concept of "defective triage" in pandemics highlights a pervasive lack of efficient planning, including insufficient workforce, absence of physicians from the triage area, and inadequate support systems for triage personnel, leaving them feeling "alone in crisis".
Issues Contributing to Emergency Department Overcrowding
Emergency department crowding is a critical symptom of broader, system-wide healthcare problems. It is primarily driven by increased patient volumes, persistent staff shortages, insufficient inpatient beds, and inefficient patient flow systems within the hospital. Inefficient triage processes themselves, alongside prolonged radiology and laboratory turnaround times and non-flexible staffing, directly contribute to inefficient ED operations and patient queuing. While existing triage scales are useful for identifying less urgent cases, they have not yet been safely utilized to refer patients from EDs to alternative, less acute care settings like primary care. The pervasive issue of ED crowding is directly associated with increased patient mortality, reduced quality of care, and severe staff burnout.
The breakdown in triage is not an isolated problem within the ED but a central bottleneck that creates cascading failures throughout the entire emergency healthcare ecosystem. Inefficient internal ED triage directly contributes to overcrowding, which then necessitates external measures like ambulance diversion. Ambulance diversion, employed when internal crowding mechanisms fail, leads to additional travel distances for Emergency Medical Services (EMS) providers and significantly prolonged turnaround times, rendering EMS units unavailable during these delays. This, in turn, stresses pre-hospital resources and increases overall system delays, creating a negative feedback loop where internal ED inefficiencies propagate outwards, diminishing the entire emergency response chain's capacity and resilience during a crisis.
Inherent Inaccuracies and Inconsistencies in Traditional Human-Based Triage Systems
A systematic review of 13 commonly used triage systems, including START, mSTART, SALT, Smart, Care Flight, ASAV, MPTT, Sieve, and ESI, revealed that most demonstrated an accuracy, sensitivity, and specificity of less than 90%. Only the Smart triage system achieved an overall accuracy exceeding 90%. This indicates a significant and concerning margin for error in patient prioritization.
A fundamental limitation of current triage systems is the absence of universally agreed-upon "gold standard" definitions for each triage category. Without such a standard, it becomes impossible to accurately calculate sensitivity and specificity or to reliably compare the accuracy of different triage systems across various studies and conditions. This heterogeneity in standards contributes to inconsistent performance and evaluation. The inherent subjectivity and absence of a universally agreed-upon standard for patient classification mean that current EDs operate with significant, built-in inefficiencies and risks, even during non-crisis periods. The cost of this subjectivity is not solely financial (wasted resources); it is profoundly measured in compromised patient safety, reduced quality of care, and an inability to reliably compare or improve triage performance across institutions. This highlights a fundamental design flaw that AI could directly address by introducing objective, data-driven standardization.
When triage systems do not function properly and miscategorize patients, it leads to a significant waste of valuable resources, delays in providing appropriate services based on patient needs, increased patient dissatisfaction, and, in critical cases, can directly endanger a patient's life. Over-triage results in the provision of unnecessary services, consuming time and resources, while under-triage leads to insufficient care, which can have life-threatening consequences. The accuracy of human-based triage is significantly influenced by the sheer number of injured patients, the scarcity of resources, the urgent demand for medical services, and the high environmental stress inherent in real disaster situations. Furthermore, the knowledge and experience of triage personnel are critical; a lack of sufficient training and experience can directly lead to misclassification of injured individuals. Internal injuries, such as internal bleeding or organ rupture, are particularly challenging to detect using standard anatomical or physiological findings, increasing the likelihood of misclassification. Some traditional triage tools, such as the START triage system, lack specific ranges for critical indicators like breathing and pulse. In contrast, systems like Sieve and Sort triage offer more precise ranges for these indicators, highlighting a potential design flaw in less granular tools that can affect precision and accuracy.
Table 1: Limitations of Traditional Triage Systems in Crisis Scenarios
III. AI as a Catalyst: Core Applications in Emergency Triage
Artificial Intelligence, through its specialized disciplines of machine learning, natural language processing, and predictive analytics, is uniquely positioned to revolutionize emergency triage by directly addressing the profound limitations inherent in current systems. AI's capabilities move beyond mere augmentation, offering a transformative shift in how emergency healthcare is delivered, particularly in high-stakes, high-volume environments.
Machine Learning for Enhanced Patient Acuity Prediction
AI-driven triage systems are fundamentally designed to overcome the challenge of information overload by seamlessly fusing multimodal data. This includes structured data, such as vital signs, laboratory results, patient demographics, medical history, and risk factors, alongside unstructured data like clinical notes, physician referrals, and patient reports. This comprehensive data integration provides a holistic and nuanced view of a patient's condition, significantly improving diagnostic accuracy and the effectiveness of treatment decisions.
Machine learning models, including advanced deep learning algorithms, consistently demonstrate superior predictive performance compared to traditional triage tools and even human judgments. These models excel at forecasting crucial outcomes such as patient disposition (e.g., discharge versus admission), identifying critical illness, predicting hospital admission, and determining eligibility for fast-track care. For example, Random Forest and Logistic Regression models have shown robust predictive capabilities in this domain. A Gradient Boosting Machine (GBM) model, for instance, achieved an impressive AUC ROC of 0.8256 in predicting hospital admissions, underscoring its efficacy in real-world scenarios.
AI tools can rapidly analyze vast data streams to standardize acuity scoring, accurately predict disease severity, and proactively flag high-risk patients who might otherwise be overlooked by busy clinicians. These systems are adept at aiding in the early recognition of critical patient deterioration, such as the onset of sepsis, stroke, or myocardial infarction, thereby prompting timely escalation of care and intervention. By applying data-driven algorithms, AI offers a consistent and objective approach to patient assessment, significantly reducing human error and the variability in triage decisions that commonly lead to over-triaging or under-triaging in traditional systems. This provides a consistent, objective, and data-driven assessment framework, which can significantly mitigate the impact of human variability, fatigue, and cognitive biases on triage decisions. This is especially crucial during large-scale health crises where staff experience levels may differ, and stress is high. This standardization promotes a more equitable standard of care, ensuring that patient prioritization is based on objective data and predicted acuity rather than individual clinician judgment or the immediate pressures of the environment. It effectively provides an algorithmic "standard" where a human one is lacking, potentially reducing health disparities.
Furthermore, AI systems provide real-time clinical decision support, empowering clinicians to validate or refine their prioritization decisions and identify subtle patterns or correlations in patient data that might escape the attention of busy human staff, especially during high-pressure situations. AI's ability to process and synthesize overwhelming amounts of diverse data effectively transforms it from raw information into actionable insights. This positions AI as an intelligent filter or cognitive offloader for human clinicians. By automating the extraction and initial synthesis of complex data, AI reduces the cognitive burden on human experts, allowing them to focus their valuable time and expertise on higher-order tasks such as complex clinical reasoning, nuanced patient interaction, and ethical decision-making. This fundamentally unlocks a vast reservoir of previously underutilized clinical intelligence embedded in unstructured notes, moving beyond simple keyword searches to deep semantic understanding, directly addressing a core human limitation in high-stakes, data-rich environments.
Natural Language Processing (NLP) for Unstructured Clinical Data
Large Language Models (LLMs) and Natural Language Processing (NLP) have demonstrated remarkable capabilities in understanding and generating clinical language, even achieving proficiency levels comparable to passing medical licensing exams. These models can effectively extract nuanced medical concepts, suggest differential diagnoses, and provide natural-language rationales for clinical decisions.
NLP plays a pivotal role in converting free-text clinical notes, physician referrals, patient reports, and chief complaints—which often contain critical diagnostic information—into structured, quantitative parameters that can be readily utilized by machine learning models for predictive analysis. Studies consistently show that incorporating unstructured data processed via NLP techniques significantly enhances the overall predictive performance of machine learning models compared to models that rely solely on structured data. This highlights the rich, unexploited information contained within clinical narratives.
For global health, advanced NLP systems, such as TriagE-NLU, integrate fine-tuned multilingual transformers. This enables them to interpret medical dialogues across multiple languages, assess urgency, and recommend appropriate interventions based on a structured semantic framework, which is crucial for emergency response in diverse populations and during global health crises. Beyond clinical interpretation, NLP-powered chatbots and voice assistants can automate initial patient information collection, appointment scheduling, and symptom sorting before patients physically interact with staff. They can also transcribe patient-clinician conversations in real-time, reducing manual documentation workload for healthcare professionals and improving the accuracy and completeness of clinical records.
Predictive Analytics for Operational Optimization
Predictive analytics offers a strategic shift from reactive to proactive emergency healthcare management. It leverages extensive historical data, including factors like day of the week, time of day, weather conditions, and even local events, combined with real-time data feeds from ambulance dispatch systems, patient registration desks, and social media sentiment analysis. This comprehensive data integration allows for accurate forecasting of incoming patient volumes and their anticipated acuity levels. This foresight enables ED leadership to proactively adjust staffing levels and allocate resources effectively in anticipation of demand surges.
AI models can accurately predict a patient's length of stay (LOS) within the ED or hospital by incorporating a wide range of factors, including patient demographics, presenting complaints, initial vital signs, and diagnostic test results. Accurate LOS prediction is critical for minimizing bottlenecks within the ED, optimizing bed management, and improving the timely deployment of ancillary services such as radiology and laboratory. By anticipating patient influx and resource demands, AI-based predictive analytics significantly enhances overall operational efficiency within the ER. This leads to substantial reductions in patient waiting times and optimizes the utilization of limited resources. Real-time AI-driven triage systems further enhance patient prioritization, ensuring that critically ill individuals receive immediate attention without delay. Moreover, AI models that integrate real-time hospital capacity data can dynamically adjust resource allocation, minimizing delays in patient transfers and discharges. This changes the operational paradigm, leading to significantly reduced wait times, improved patient outcomes, and optimized resource utilization, thereby enhancing overall system resilience and efficiency. This proactive capability is particularly vital for mitigating the impact of unexpected surges, such as those caused by emerging global health threats.
AI in Crisis Response: Addressing Emerging Global Health Threats
Beyond its profound impact on individual patient triage, AI's transformative potential extends to broader systemic applications in public health preparedness and response, particularly critical for addressing emerging global health threats like pandemics and mass casualty incidents.
Syndromic Surveillance and Early Outbreak Detection
AI has emerged as a powerful tool for significantly improving infectious disease surveillance and early warning systems. It achieves this by processing and analyzing massive datasets from diverse sources in real-time. These sources include open-source internet data, such as news reports, social media activity, and health forums, which provide early outbreak signals before official health notifications. Additionally, traditional health system data, including Electronic Health Records (EHR), laboratory information systems, and official epidemiological reports, along with personal health data from wearable devices, and environmental/contextual data like temperature, humidity, travel patterns, genomic data, and wastewater surveillance, are all integrated.
AI algorithms are adept at identifying subtle patterns and detecting anomalies within these diverse data streams that may signal emerging public health threats, often before official health notifications are released. A notable example is BlueDot, an AI-driven platform that identified an unusual pneumonia outbreak in Wuhan prior to official confirmation, demonstrating AI's predictive power. This capability enables earlier detection of threats and more accurate prediction of their trajectory. This represents a fundamental shift from traditional epidemiological surveillance, which often causes delays, to a dynamic, anticipatory model, thereby profoundly enhancing pandemic preparedness at a population level and enabling more agile policy interventions.
AI algorithms can predict potential outbreaks based on historical and real-time data, enabling earlier detection and more timely interventions. This capability is crucial for pinpointing areas of high-transmission potential, allowing for the efficient and targeted allocation of limited healthcare resources. AI-powered syndromic surveillance systems automatically generate alerts to notify public health officials, healthcare providers, and other key stakeholders. These alerts are often accompanied by actionable recommendations, significantly speeding up response times and enabling more informed decision-making. Recent advances in AI methodologies demonstrate improved performance even when dealing with limited or noisy data, which has historically been a major bottleneck in rapid pandemic preparedness and response efforts. This positions AI as the central nervous system for global health security, integrating disparate data streams and identifying subtle anomalies that human systems might miss, creating a comprehensive, real-time intelligence layer.
Mass Casualty Incident (MCI) Management and Resource Deployment
Mass Casualty Incidents (MCIs) pose significant challenges, often overwhelming available resources and causing traditional triage systems to fail. AI tools, when integrated into comprehensive emergency response toolkits such as the EU-funded NIGHTINGALE project, significantly improve situational awareness, optimize the allocation of scarce resources, and provide critical support for patient prognosis and decision-making during MCIs. The NIGHTINGALE toolkit, for example, facilitates rapid victim identification and assessment through innovative technologies like digital triage tags, augmented reality glasses, wearables, and earplug sensors. Mobile applications and triage dashboards enable responders to instantly visualize vital signs in real-time, streamlining initial assessments.
AI, particularly through the integration of robotics, unmanned aerial vehicles (UAVs), and advanced logistics, directly addresses the critical "last mile" problem in disaster response. This means getting crucial information and life-saving resources to where they are most needed, quickly and safely, even in dynamic, hazardous, or inaccessible environments. UAVs and mobile systems leverage AI to perform rapid scanning and remote detection of vital signs, providing crucial insights even before human first responders arrive on the scene. Systems like ARTEMIS, an AI-driven Robotic Triage labeling and Emergency Medical Information System, utilize speech processing, Natural Language Processing, and deep learning on quadruped robots for victim localization and preliminary injury severity assessment, achieving high accuracy, particularly for the most critical victims. This capability reduces the reliance on human responders for initial assessment in dangerous zones and ensures that scarce medical resources are deployed with unprecedented precision, minimizing avoidable delays and improving patient outcomes in chaotic, high-stakes scenarios.
AI is also increasingly being adopted in both military and civilian supply chains to accurately forecast supply needs, automate procurement processes, and intelligently orchestrate routing in fluid, high-risk environments. This includes predicting demand for critical items like trauma kits, blood products, and vaccines, and dynamically adjusting delivery routes based on real-time threats or disruptions. AI-driven command centers can interpret pathogen trends at scale, enabling quick, evidence-based decisions on interventions such as testing, vaccination campaigns, and local guidelines.
Accelerating Pathogen Characterization and Vaccine Development
AI is revolutionizing vaccine development by significantly enhancing the speed, precision, and scalability of immunological research. Deep learning algorithms streamline the identification of immunogenic targets and conserved antigens, which is critical for the rapid creation of vaccines for highly mutable pathogens like SARS-CoV-2, HIV, and influenza. AI also plays a role in optimizing adjuvants to enhance vaccine efficacy.
AI offers a powerful alternative to traditional, time-consuming laboratory experiments by simulating immune responses in silico (via computer models). This provides invaluable insights into vaccine efficacy and safety profiles, significantly benefiting and accelerating the clinical trial process. A key advancement is AI's ability to predict pathogen evolution. This enables the design of "future-proof" vaccines that anticipate future mutations, a crucial capability for responding to rapidly evolving infectious agents.
AI transforms biomedical research from a largely retrospective, labor-intensive, and often trial-and-error process into an anticipatory, data-driven, and highly efficient endeavor. By rapidly synthesizing existing scientific knowledge and predicting future biological trends (e.g., viral mutations, disease spread patterns), AI dramatically shortens the discovery-to-deployment cycle for vaccines and therapeutic treatments. This is not merely an incremental improvement but a fundamental shift in how humanity can proactively develop defenses against novel and re-emerging pathogens, offering a powerful, anticipatory mechanism against future global health threats.
AI and machine learning tools, such as the RAPTER project, are designed to screen vast scientific publications and databases. This allows them to rapidly collect existing research data, identify critical knowledge gaps, and systematically lay out the best options for vaccine development based on a pathogen's genetic sequence data. This capability significantly speeds up the initial research and development phases, enabling a more rapid response to disease outbreaks.
Implementation Realities: Case Studies, Challenges, and Ethical Imperatives
While the theoretical potential of AI in emergency healthcare is immense, its practical implementation is subject to real-world complexities. This section highlights successful pilot programs, alongside critical challenges that must be addressed to ensure widespread, equitable, and ethical adoption.
Pilot Programs and Observed Outcomes
Several initiatives demonstrate the tangible benefits of AI in emergency triage. UMass Memorial Health, for instance, has successfully deployed KATE AI, a machine learning platform designed to support ED triage nurses. This system analyzes intake form data and Electronic Health Records (EHRs) to generate Emergency Severity Index (ESI) scores, providing a more nuanced picture of a patient's condition. KATE AI enhances triage by identifying clinical subtleties, such as underlying chronic conditions that might otherwise be overlooked, and offers early sepsis detection capabilities, alerting nurses to potential red flags and supporting timely interventions. Observed improvements include a significant increase in ESI scoring accuracy, rising from approximately 55% to nearly 70%, improved clinical documentation accuracy, reduced "left-without-being-seen" rates, fewer risk reports related to triage, and enhanced analytical capabilities for understanding complex patient populations (e.g., drug overdoses, cardiac events), thereby aiding in targeted interventions and long-term planning.
The EU-funded NIGHTINGALE project aimed to radically improve pre-hospital emergency responses during Mass Casualty Incidents (MCIs) through an advanced, integrated toolkit. Key outcomes include rapid victim identification and assessment facilitated by digital triage tags, augmented reality glasses, wearables, and earplug sensors. A mobile app and triage dashboard enable responders to visualize vital signs instantly and in real-time. The toolkit integrates powerful AI components to enhance situational awareness, optimize resource allocation, and support patient prognosis and decision-making. Unmanned aerial vehicles (UAVs) and mobile systems facilitate rapid scanning and remote detection of vital signs, providing crucial insights even before responders arrive. The project also emphasized user-centric design, ensuring adaptability to extreme conditions like network loss or power outages, and seamless integration with existing EMS systems.
Systematic reviews of AI-driven triage systems generally indicate their potential to reduce triage time, improve documentation accuracy, and enhance decision support. For example, voice-based AI systems have achieved 19% faster documentation compared to manual methods, while machine learning algorithms have reduced mis-triage rates by 0.3-8.9%. Overall, AI-based applications have demonstrated acceptable accuracy levels and facilitate prompt and precise decision-making in emergency settings.
Despite these promising results, most existing studies on AI in triage are single-center, retrospective, and carry a high risk of bias, with very few examples of models successfully deployed into routine clinical practice. Identified limitations include risks of undertriage, variable accuracy across different contexts, significant workflow integration barriers, and insufficient metrics to assess clinician acceptance.
Ethical Considerations
The integration of AI into healthcare, while beneficial, introduces significant ethical complexities. A primary concern is algorithmic bias and fairness. AI models, particularly those trained on unrepresentative or biased historical data, possess the potential to perpetuate and even exacerbate existing racial, gender, and socioeconomic disparities within healthcare. This can manifest as inaccurate diagnoses, unfair treatment, or disproportionate harm for vulnerable patient groups. Studies indicate that a substantial percentage of AI models in healthcare lack transparency regarding their internal workings, making bias detection and mitigation challenging.
Many AI systems operate as "black boxes," meaning their decision-making processes are opaque and difficult for clinicians and patients to understand. This lack of interpretability can erode trust in the AI system and hinder its full adoption and effective utilization by healthcare professionals. Tools like SHAP (SHapley Additive exPlanations) and LIME (Local Interpretable Model-agnostic Explanations) are being developed to make AI decisions more understandable and auditable.
Establishing clear lines of responsibility is crucial when AI triage leads to adverse patient outcomes. This requires navigating complex legal frameworks and determining who is accountable—the clinician, the AI developer, or the hospital. Compliance with data privacy regulations such as HIPAA (Health Insurance Portability and Accountability Act) and GDPR (General Data Protection Regulation) for data privacy and use is also a significant legal and ethical challenge. AI systems necessitate access to vast amounts of highly sensitive patient data for training and operation. This raises paramount concerns about how this data is collected, stored, utilized, and protected from potential breaches or unintended misuse.
Clinician acceptance and trust are paramount for the successful integration of AI. If emergency workers doubt the AI's fairness, accuracy, or reasoning, they may choose to ignore its advice, thereby negating its potential benefits. Similarly, public trust in AI for direct health advice remains low.
To address these ethical challenges, several solutions and frameworks are proposed. Bias mitigation strategies include implementing fairness-constrained optimization techniques, training AI with diverse, complete, and representative datasets, and establishing continuous monitoring mechanisms for algorithmic bias. Transparency can be enhanced by requiring AI systems to provide clear explanations for their risk assessments and recommendations, utilizing explainable AI tools, and designing protocols that integrate AI advice with human clinician judgment to maintain a clear understanding of decision-making. Accountability necessitates establishing clear ethical rules and protocols that define responsibility for AI decisions, requiring a collaborative effort involving AI experts, clinicians, hospital leaders, and regulatory bodies in the policy creation process. Data privacy requires ensuring strict compliance with privacy laws like HIPAA and GDPR, implementing robust data protection measures (e.g., end-to-end encryption, federated learning), and ensuring secure data integration with existing hospital systems. Finally, clinician engagement is fostered by providing comprehensive training for staff on AI's capabilities and limitations, fostering continuous dialogue with regulators, and prioritizing clinician input throughout the AI system design and implementation phases.
Regulatory Landscape and Challenges
The regulatory landscape for AI in healthcare is rapidly evolving. Medical device regulators worldwide, notably the FDA in the U.S. and the European Union (EU) with its AI Act, are becoming increasingly proactive in developing and implementing new frameworks. These frameworks demand more rigorous development, validation, and post-market surveillance for AI-enabled medical devices compared to traditional "rule-based" software.
The U.S. FDA adopts a "Total Product Lifecycle" model for AI/ML-based Software as a Medical Device (SaMD). This includes "Predetermined Change Control Plans" (PCCPs) for adaptive AI/ML devices and a growing reliance on "Real-World Evidence" (RWE) for continuous post-market monitoring and improvement. The FDA aims to strike a balance between enabling innovation and ensuring patient safety, and has already authorized many AI-enabled devices, particularly in radiology.
In contrast, the EU AI Act represents a comprehensive, risk-based regulatory framework that classifies AI systems, with AI-based medical devices falling into the "high-risk" category. It mandates stringent requirements for risk-mitigation systems, high-quality datasets, clear user information, human oversight, and robust post-market surveillance. A unique challenge in Europe is the requirement for "dual certification," necessitating compliance with both existing Medical Device Regulations (MDR/IVDR) and the new AI Act.
A significant challenge in adapting to these frameworks is that the traditional "train-then-validate" approach for static software is not well-suited for adaptive AI models that continuously learn and evolve. Ensuring that AI performance does not degrade or worsen with continuous learning requires robust safeguards. Furthermore, regulatory frameworks must adapt to effectively support and govern telemedicine services, which are increasingly integrated with AI. A significant gap remains in the need for rigorous multi-center validation and standardized outcome reporting for AI systems. While the FDA and EU are leading in AI regulation, the global AI medical device regulatory landscape is rapidly expanding, requiring manufacturers and healthcare providers to stay informed and engaged with diverse international requirements.
Implementation Challenges (Broader Operational and Technical)
Beyond ethical and regulatory hurdles, the practical integration of AI into emergency healthcare faces several broader operational and technical challenges. Integrating new AI tools into existing, often complex and entrenched, emergency department workflows presents a significant operational barrier. This requires careful planning and adaptation to avoid disrupting daily routines and to ensure seamless adoption.
Gaining the trust and buy-in from frontline healthcare professionals is crucial for the successful and effective adoption of AI. Without adequate acceptance, AI tools may be underutilized or bypassed, negating their potential benefits. The effectiveness of AI models is fundamentally dependent on the availability of large, diverse, high-quality, and well-annotated datasets for training. Poor, biased, incomplete, or inconsistent data can lead to inaccurate predictions, exacerbate existing health disparities, and ultimately hinder the AI system's performance. Furthermore, reliable and low-latency internet connectivity is essential for the seamless operation of telemedicine services and AI-driven systems, particularly for real-time data streaming and processing in high-stakes clinical settings. Finally, healthcare professionals require adequate and ongoing training not only in telemedicine practices but also in the effective and ethical use of AI tools.
VI. Conclusion and Recommendations
The transformation of emergency healthcare triage through Artificial Intelligence is not merely an incremental upgrade but a strategic imperative for building resilient and responsive global health systems capable of confronting emerging threats. Traditional triage methodologies, characterized by human cognitive overload, staffing limitations, inherent subjectivity, and reactive operational models, are demonstrably inadequate in the face of large-scale health crises and persistent emergency department overcrowding. These limitations lead to suboptimal accuracy, inefficient resource allocation, and compromised patient outcomes.
AI, through its capabilities in machine learning, natural language processing, and predictive analytics, offers a profound paradigm shift. It enables the comprehensive analysis of multimodal patient data, leading to superior acuity prediction and risk stratification. AI-driven systems can mitigate human error and subjectivity, providing consistent and objective assessments that standardize care. Furthermore, AI facilitates proactive operational optimization by accurately forecasting patient flows, predicting length of stay, and dynamically allocating resources, moving emergency care from a reactive to an anticipatory model. Beyond the individual patient, AI serves as a critical nervous system for global health security, enabling early outbreak detection through syndromic surveillance and enhancing mass casualty incident management via improved situational awareness, robotic assistance, and streamlined logistics. Moreover, AI is accelerating biomedical innovation, particularly in pathogen characterization and vaccine development, fundamentally transforming the pace at which humanity can respond to novel biological threats.
However, the successful and equitable integration of AI into emergency healthcare demands meticulous attention to implementation realities. Ethical considerations, particularly algorithmic bias, transparency, accountability, and data privacy, must be proactively addressed through robust frameworks, diverse data training, and clear guidelines. The evolving regulatory landscape, exemplified by the FDA's lifecycle approach and the EU AI Act's comprehensive risk-based framework, necessitates rigorous validation, continuous monitoring, and international collaboration. Operational challenges, including workflow integration, clinician acceptance, data quality, and infrastructure requirements, also require strategic planning and investment.
To realize the full transformative potential of AI in emergency healthcare, the following recommendations are put forth:
Prioritize Collaborative Research and Development: Foster multi-center, prospective studies with standardized outcome reporting to rigorously validate AI-driven triage systems in diverse real-world settings. Encourage collaboration between AI developers, healthcare institutions, and public health agencies to ensure solutions are clinically relevant, scalable, and adaptable to various crisis scenarios.
Invest in Robust Data Infrastructure and Governance: Establish secure, interoperable data ecosystems that facilitate the collection, integration, and analysis of high-quality, diverse, and representative multimodal healthcare data. Implement strong data governance frameworks that ensure privacy (e.g., HIPAA, GDPR compliance), security (e.g., federated learning, encryption), and ethical data use for AI model training and deployment.
Develop and Enforce Ethical AI Guidelines: Implement comprehensive ethical frameworks that mandate bias mitigation strategies (e.g., fairness-constrained optimization, diverse datasets), ensure transparency and explainability of AI decisions (e.g., explainable AI tools), and clearly define accountability for AI-driven outcomes across all stakeholders.
Strengthen Regulatory Pathways and International Harmonization: Actively engage with regulatory bodies (e.g., FDA, EU AI Act) to shape agile and comprehensive regulatory pathways for AI-enabled medical devices, particularly those with adaptive learning capabilities. Promote international harmonization of AI regulations to facilitate global adoption and cross-border emergency response.
Cultivate a Culture of AI Literacy and Trust: Implement extensive training and education programs for healthcare professionals, from frontline staff to leadership, on the capabilities, limitations, and ethical implications of AI tools. Foster clinician engagement in the design and implementation phases to build trust and ensure seamless workflow integration. Educate the public on the role of AI in healthcare to enhance acceptance and cooperation during crises.
Integrate AI into National and Global Health Preparedness Strategies: Incorporate AI-driven syndromic surveillance, predictive analytics for resource allocation, and AI-accelerated vaccine development into national and international pandemic preparedness and mass casualty incident response plans. This includes investing in AI-enabled robotics and UAVs for remote assessment and logistics in hazardous environments.
