The French Emergency Nurses Classification in Hospital (FRENCH)
The French Emergency Nurses Classification in Hospital (FRENCH) is a standardized, multi-level triage system officially recommended by the French Society of Emergency Medicine (SFMU) for use in French emergency departments (EDs).

The French Emergency Nurses Classification in Hospital (FRENCH) is a standardized, multi-level triage system officially recommended by the French Society of Emergency Medicine (SFMU) for use in French emergency departments (EDs). Developed to streamline patient prioritization and optimize resource allocation, the system provides a structured framework for nurses to make critical, time-sensitive decisions. While the scale is formally described as having five levels, a key modification functionally transforms it into a six-level system by splitting the third category into two sub-levels, 3A and 3B, to account for patient comorbidities and referral sources.
This analysis indicates that the FRENCH scale is a robust and highly validated tool. Research has demonstrated its strong reliability and validity, with a clear correlation between a patient's triage category and their subsequent resource consumption and hospital admission rates. A comparative study found that the FRENCH scale provides superior triage results compared to the widely used US-based Emergency Severity Index (ESI), exhibiting a significantly lower tendency for under-triage, particularly for the most severe patients.
However, the system's effectiveness is not without its challenges. The FRENCH scale is based on an extensive list of approximately 100 determinants, including vital signs, chief complaints, and suspected diagnoses. This complexity, while enhancing clinical precision, can also contribute to inconsistencies in application due to human factors such as disparities in nurse experience, time pressure, and fatigue. These inconsistencies can lead to triage errors, a problem that has prompted the development of artificial intelligence (AI) models to improve consistency and accuracy in classification.
In conclusion, the FRENCH scale represents a sophisticated and contextually tailored solution to the challenges of emergency department management. Its clinical superiority over other scales and its strong internal validation affirm its value. For continued success, its implementation must be supported by robust, continuous training and a strategic exploration of how emerging technologies can mitigate the impact of human variability on its consistent application.
The Evolution and Mandate of Triage in France
The practice of triage, a cornerstone of modern emergency medicine, finds its origins in the French military. The term itself is derived from the French verb "trier," which means to sort, separate, or select. This concept was first operationalized in a systematic way by Baron Dominique Jean Larrey, a surgeon in Napoleon Bonaparte's imperial guard, who created a system to quickly evaluate and categorize wounded soldiers based on the severity of their injuries and the urgency of their need for care. This principle—that priorities should be based on need, not on rank or status—established the ethical and logistical foundation for modern triage.
The application of triage to civilian hospitals began in the 1960s as a response to the increasing demand on emergency departments. The imperative for a structured system became clear as EDs experienced a steady rise in patient volumes, leading to significant challenges such as overcrowding and prolonged waiting times. Prolonged waiting times are not merely an inconvenience; they are a persistent challenge that can lead to delayed medical intervention, a decline in the quality of care, and increased patient dissatisfaction. In France, this issue is particularly pronounced, with data revealing that a significant percentage of patients experience wait times exceeding four hours, and elevated waiting times are identified as the sole independent risk factor for patient dissatisfaction.
To address these systemic challenges, a standardized approach to patient sorting and resource allocation became a necessity. The French healthcare system, recognizing this, developed context-specific tools to fit its unique professional practices and linguistic requirements. The French Emergency Nurses Classification in Hospital (FRENCH) was created to serve as a national, standardized triage scale. The development of such a French-language system was crucial, as direct translations of pre-existing English-language scales were found to be insufficient due to linguistic constraints and major differences in prehospital medical care models, which in Europe are often physician-led as opposed to paramedic-based systems used elsewhere. The creation of the FRENCH scale is a reflection of a deliberate national effort to produce a robust, context-specific classification tool.
The FRENCH Triage System: Foundational Principles and Structure
The French Emergency Nurses Classification in Hospital (FRENCH) is the official name of the triage system recommended by the French Society of Emergency Medicine (SFMU) for use in emergency departments. The core purpose of the system is to distribute the ED workload and ensure the optimal utilization of resources by categorizing patients based on the urgency and severity of their conditions. The triage process is a two-stage nursing intervention: an initial assessment that results in the assignment of a triage category, followed by the initiation of nursing interventions to facilitate care and reduce patient discomfort.
A central point of discussion and clarification for the FRENCH scale is its classification structure. Although it is frequently cited as a five-level system, it is more accurately described as a six-level system in practice. The SFMU initially created a five-priority-level scale, but subsequently, a critical modification was made. The original level 3 was split into two additional sub-levels, 3A and 3B, specifically to better prioritize patients who were either referred by a physician or who presented with a comorbidity related to their reason for seeking care. This segmentation of level 3 into two distinct categories demonstrates a nuanced approach to risk stratification, acknowledging that patient complexity extends beyond immediate signs and symptoms to include a patient's clinical history and care pathway. Therefore, while the scale is conceptually a five-category framework, its practical application involves six distinct priority levels: 1, 2, 3A, 3B, 4, and 5.
This nuance in the FRENCH scale's design sets it apart from other triage systems and is a primary reason why other French-language scales have been developed. For example, the Echelle Liégeoise d'Index de Sévérité à l'Admission (ELISA), another five-category system, was created because the FRENCH scale was perceived as having a "discouraging number of determinants" that included a "suspected diagnosis" and complex "triage modulators". The creators of ELISA aimed for a simpler, flowchart-based system that intentionally omits diagnostic hypotheses and requires less training time to master. This contrasts with the
Classification Clinique des Malades aux Urgences (CCMU), which is a physician-determined, seven-level scale used in both pre-hospital and hospital settings, and is not a nurse-led tool like the FRENCH and ELISA scales. These distinctions highlight a broader professional culture in France of developing specialized, contextually relevant tools rather than adopting a single, universal system.
Algorithmic Criteria and Clinical Application
The FRENCH scale is predicated on an extensive, detailed algorithm based on approximately 100 determinants, which include patient complaints, vital signs, and other clinical parameters. The system is designed to provide a high level of precision and reliability in its classifications. Each triage criterion is specifically linked to a triage level, with a definitive hierarchy of urgency. The following is a detailed breakdown of each level, synthesizing information from various clinical examples and criteria presented in the research.
This granular approach, with its many determinants, is a double-edged sword. On one hand, it enhances the clinical precision of the classification. On the other, the research notes that this level of detail, particularly the complexity of "triage modulators" that influence a nurse's final judgment, may have limited the widespread implementation of the scale due to the perceived need for "onerous" training.
The Triage Nurse: Role, Training, and Consistency
The naming of the system as the "French Emergency Nurses Classification" highlights the central and authoritative role of the ED nurse in the triage process. The nurse is responsible for the critical two-stage intervention: first, making a rapid and accurate assessment to assign a triage category and, second, initiating early interventions to reduce discomfort and facilitate the patient's care pathway. This role demands a high degree of clinical expertise and judgment.
The system's complexity is a defining feature of the nurse's role. The FRENCH scale is based on an extensive list of determinants, with some clinical tools like ELISA being developed as a simpler alternative because of the perceived burden of training for the FRENCH algorithm. However, a direct comparison of FRENCH to the American ESI scale reveals a more nuanced perspective. In a study involving both experienced nurses and nursing students, the FRENCH scale was found to be more practical and safer to use than the ESI scale, suggesting that a well-designed system, even with a high number of determinants, can be intuitive and effective in practice. The existence of a dedicated course on the FRENCH scale on the SFMU’s e-learning platform demonstrates that formalized training resources are available to support nurses in mastering the system.
Despite the system's design and training efforts, its application often varies in real-world clinical settings. This variability is driven by a range of human factors, including differences in nurse experience, the immense pressure of time, interpretive inconsistencies, and fatigue. Such inconsistencies can lead to significant triage errors. For instance, "undertriage" occurs when a high-acuity patient is misclassified as a lower priority, risking treatment delays and negative patient outcomes. Conversely, "overtriage" involves assigning a disproportionately high priority to a low-acuity case, which leads to inefficient resource allocation and contributes to ED crowding. These persistent human-factor challenges are a primary motivation behind the development of artificial intelligence models, which are being trained and validated using the FRENCH scale to see if they can improve the consistency and accuracy of patient triage.
Performance Analysis: Effectiveness, Validity, and Outcomes
The FRENCH scale has been rigorously evaluated for its reliability and validity in clinical practice. The research indicates that the scale exhibits a good level of inter-rater reliability, with a weighted kappa coefficient of 0.77, which suggests a strong and consistent agreement between different nurses applying the scale to the same patient scenarios.
The scale's validity, or its ability to accurately predict patient outcomes and needs, is also well-supported by data. Studies have found a strong correlation between a patient's assigned triage category and their subsequent resource consumption and admission to the hospital. This demonstrates that the scale effectively stratifies patients according to their true clinical severity and complexity. Furthermore, the predictive accuracy of the scale for hospital admission is high, with the area under the receiver operating characteristic curve (AUC) measured at 0.858. These findings affirm that the FRENCH scale is a robust and validated tool for clinical use.
While the research does not provide a direct, longitudinal study on the FRENCH scale's impact on waiting times, it provides significant contextual information. The problem of prolonged waiting times and ED overcrowding is a major concern in France. Triage is identified as a primary intervention to address this issue by expediting patient assessment and optimizing resource allocation. General evidence suggests that implementing streamlined triage protocols can significantly decrease patient wait times and improve ED efficiency. Moreover, a study on "team triage," which involves both nurses and physicians, was found to reduce waiting times and the overall length of stay compared to conventional triage methods. This indicates that the effectiveness of the FRENCH scale is not only a function of the algorithm itself but also of the operational workflow into which it is integrated.
A significant new development is the use of the FRENCH scale as a benchmark for AI-based triage systems. Recent studies have developed and tested AI models, such as Large Language Models (LLMs), to predict patient triage levels based on clinical data and nurse-patient interactions. One such study found that an LLM model, URGENTIAPARSE, demonstrated higher accuracy than human nurses in predicting FRENCH triage outcomes. The success of these models validates the underlying rigor of the FRENCH scale while simultaneously suggesting a future where technological tools may be used to augment human decision-making, improving consistency and reducing the impact of human factors on patient prioritization in a crowded clinical environment.
Comparative Triage Systems: A Global and Local Context
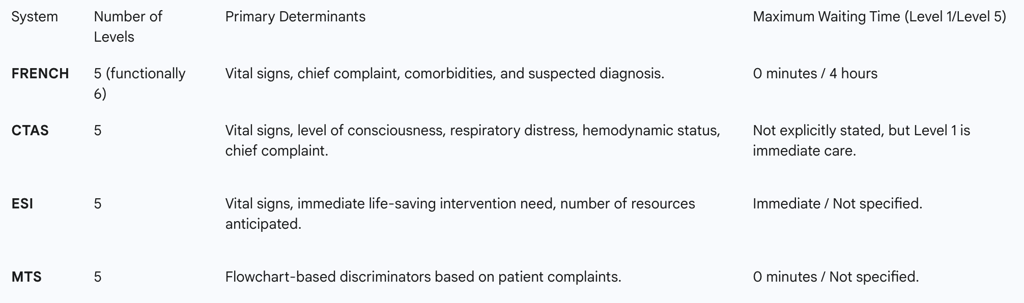
The FRENCH scale is a part of a global landscape of five-level triage systems, each developed to suit the specific healthcare context and practices of its respective country. Other prominent systems include the Canadian Triage and Acuity Scale (CTAS), the Australasian Triage Scale (ATS), the Manchester Triage System (MTS), and the Emergency Severity Index (ESI). A comparison of these systems provides a clearer understanding of the FRENCH scale's unique features and strengths.
FRENCH versus ESI
The most direct comparison available in the research is between the FRENCH scale and the American-based Emergency Severity Index (ESI). A study comparing these two scales found that the FRENCH scale provided "better triage results" than the ESI scale. A particularly critical finding was that the ESI had a "big tendency to under-sort," especially for the most severe patients, a dangerous error that the FRENCH scale was less prone to. This finding is a significant validation of the FRENCH scale’s ability to accurately and safely prioritize high-acuity cases. Furthermore, despite the perceived complexity of the FRENCH algorithm, nurses and nursing students found it "significantly more practical" and "safer" to use than the ESI scale, indicating a positive user experience that likely enhances its consistent application in clinical practice.
FRENCH versus Other Systems
The Manchester Triage System (MTS), widely adopted across Europe and Australia, is a flowchart-based system that assigns patients to one of five urgency categories, each with a color code and a defined maximum waiting time (e.g., Red for 0 minutes, Orange for 10 minutes). The FRENCH scale also assigns maximum delays to its categories, such as up to four hours for non-urgent patients. The Canadian Triage and Acuity Scale (CTAS) shares similar level nomenclature with FRENCH, categorizing patients into levels such as Resuscitation, Emergent, Urgent, Less Urgent, and Non-Urgent, and uses vital signs and chief complaints as key determinants. These similarities suggest a convergence of professional best practices across different national healthcare systems, even with the use of distinct, locally developed scales.
The following table provides a concise comparative overview of the key features of these major triage systems.
Conclusion: Synthesis, Challenges, and Future Perspectives
The French Emergency Nurses Classification in Hospital (FRENCH) scale stands as a reliable and validated triage tool specifically designed for the unique clinical and cultural context of French emergency medicine. Its strengths are evident in its detailed, multi-level structure, which includes a sophisticated split of the urgent category (3A and 3B) to account for patient complexity. The scale's strong correlation with resource consumption and admission rates confirms its predictive validity, and a comparative analysis has positioned it as a superior tool for preventing dangerous under-triage when compared to the ESI scale.
The primary challenges confronting the FRENCH scale are not with its design but with its application. The algorithm's complexity and the influence of human factors, such as fatigue and varying levels of nurse experience, can lead to inconsistencies in its use. These factors create a systemic vulnerability to triage errors, which can compromise patient safety and clinical efficiency. This inherent human variability has become the most significant hurdle to achieving perfect triage consistency, a challenge that has catalyzed innovation within the field.
The future of the FRENCH scale lies in a strategic synthesis of its proven clinical framework with modern technology. The emergence of AI models that can accurately predict FRENCH triage outcomes presents a promising path forward. By integrating AI-assisted tools, it may be possible to standardize the application of the scale, reducing the impact of human variability and freeing nurses to focus on the immediate clinical care and intervention that is the second stage of their triage role. Ongoing research should continue to explore how to best integrate these technologies to enhance the scale's effectiveness in managing the persistent challenges of ED overcrowding and patient flow. The FRENCH scale, a testament to a national commitment to specialized and validated tools, remains a powerful and relevant instrument for emergency medicine, poised to evolve alongside new technologies to meet the demands of modern healthcare.
