The Evolution and Importance of Modern Healthcare Triage


This report offers a comprehensive examination of healthcare triage, tracing its historical evolution from military origins to its indispensable role in modern civilian healthcare. It delves into the foundational principles, diverse methodologies, profound benefits, inherent challenges, and the transformative impact of technology on triage practices. The report underscores triage as a dynamic process critical for optimizing patient outcomes, resource allocation, and operational efficiency, particularly in high-demand environments.
The analysis reveals that the core purpose of triage—sorting and prioritizing individuals to facilitate decision-making and optimize care—has remained remarkably consistent despite vastly different historical and technological contexts. This enduring relevance highlights triage not merely as a historical artifact but as a fundamental, adaptive principle of resource management. A significant ethical shift occurred early in its history, moving from prioritizing military expediency to a more humanitarian, patient-centered approach based on injury severity. This foundational ethical framework laid the groundwork for universal application in civilian settings.
Key findings include the catalytic role of conflict in driving medical innovation, particularly in trauma care and prehospital systems, which subsequently migrated to civilian practice. However, a persistent challenge lies in translating these innovations into sustained, integrated national healthcare systems, often hindered by inconsistent policy and funding. Modern triage systems, while diverse in their methodologies (e.g., START, ESI, CTAS, MTS), continuously seek to balance speed with diagnostic accuracy. The inherent ethical complexities of triage, particularly in resource-constrained environments, necessitate robust frameworks and transparent decision-making.
Technological advancements, especially in Artificial Intelligence (AI) and predictive analytics, are poised to revolutionize triage by enhancing accuracy, reducing wait times, and optimizing resource allocation. Yet, their successful integration requires addressing critical issues such as data quality, algorithmic bias, and fostering clinician and patient trust. The future of triage demands continuous adaptation, research, and technological integration to meet evolving healthcare demands and improve global health outcomes, ensuring that care remains equitable and efficient.
Defining Triage in Modern Healthcare
Etymology and Core Definition
The term "triage" originates from the French word "trier," meaning "to choose" or "to sort". In the context of healthcare, it is precisely defined as "the assignment of degrees of urgency to wounds or illnesses to decide the order of treatment of a large number of patients or casualties". This process becomes crucial when the demand for medical personnel and resources outstrips the available supply, necessitating a systematic approach to prioritize care. The fundamental definition and application context of triage have remained consistent across centuries, from its purported origins in sorting coffee beans to its first recorded applications on battlefields and its indispensable role in today's urban mass casualty situations.
Brief Historical Context and Report Overview
Triage, born out of necessity in the early days of modern medicine, has evolved into a critical component of healthcare systems worldwide. Its initial recorded applications were on Napoleon's battlefields, where it facilitated the grouping and decision-making for the wounded. Today, its importance extends beyond mass casualty incidents to routine emergency department operations, where it is vital for managing patient flow, efficiently allocating resources, and ensuring timely care.
The enduring core purpose of triage, which is to sort and prioritize based on urgency, has remained a constant throughout its evolution. Despite vastly different historical contexts—from military conflicts with limited surgical options to modern urban healthcare with advanced technology—the fundamental challenge that triage addresses, namely the imbalance between patient demand and available resources, persists. This highlights that triage is not merely a historical artifact but a foundational, adaptive principle of resource management in healthcare. Its continuous presence underscores that resource scarcity, whether absolute (e.g., a mass casualty event) or relative (e.g., daily emergency department overcrowding), is an inherent and ongoing challenge in healthcare systems. This enduring relevance further emphasizes that triage is a continuous, dynamic process of ethical resource allocation, not just an emergency measure. Its evolution reflects society's changing values regarding who receives care and why, shifting from prioritizing soldiers who could quickly return to duty to prioritizing based on medical severity regardless of rank or nationality. This adaptability makes triage a cornerstone of resilient healthcare systems. This report will explore this evolution, its underlying principles, various modern systems, profound benefits, inherent challenges, and the transformative future role of technology.
The Historical Evolution of Triage: From Battlefield to Bedside
Pioneering Efforts: Dominique-Jean Larrey and Military Medicine
Baron Dominique-Jean Larrey (1766–1842), Napoleon's surgeon, is widely recognized for establishing both an ambulance corps, known as the "ambulances volantes," and a classification system for the wounded on the battlefield that enabled the prioritization of evacuation. He is frequently referred to as the "father of modern-day ambulance services" due to his profound contributions.
Larrey's innovations revolutionized military medical care by advocating for the rapid evacuation of the wounded. Prior to his efforts, medical teams were typically stationed at least three miles behind the frontline, compelling wounded soldiers to wait for days for treatment or, in many cases, never receive it, with higher-ranking soldiers often receiving preferential treatment. Larrey's "flying ambulances" were light, wooden horse-drawn carriages designed for swift transport, which significantly reduced response times and increased survival rates by quickly moving soldiers from the battlefield.
A crucial aspect of Larrey's contribution was his introduction of a new system for treating the wounded based on the seriousness of their injuries, rather than their military rank or nationality. This represented a significant departure from earlier military triage practices, which primarily valued soldiers who could be quickly returned to duty. Larrey theorized that critically injured patients should undergo surgery first and as soon as possible, ideally within an hour of presentation. He correctly believed that surgical procedures would be shorter, cleaner, safer, and less painful when the patient was in shock due to relaxed muscles and lower blood pressure. His profound humanism, extending care even to enemy soldiers, earned him the reputation as "father to the wounded". The first application of this refined modern triage system, distinct from the earlier "Napoleonic triage" which prioritized sustaining military strength, occurred at the Battle of Jena in 1806.
This historical development reveals a foundational ethical shift in triage. Earlier military triage prioritized soldiers who could be quickly returned to duty, aligning with a utilitarian military objective of maximizing fighting force. In stark contrast, Larrey's system prioritized treatment based on injury severity, irrespective of rank or nationality, and notably included the treatment of enemy soldiers. This represents a profound ethical movement from a purely utilitarian military objective to a more humanitarian, patient-centered approach focused on saving lives based on medical need and the principle of beneficence. The "Napoleonic triage" focused on military expediency, whereas Larrey's refined system aimed to save as many lives as possible, embedding a moral imperative into medical practice during conflict. This early ethical framework laid the groundwork for the universal application of triage in civilian settings, where the primary goal is individual patient well-being and equitable care. Larrey's innovation was not just logistical (ambulances) or procedural (sorting by severity); it infused a profound ethical dimension into medical practice. This shift highlights that major medical advancements are often intertwined with evolving societal values and ethical considerations, frequently driven by the intense pressures of combat. It underscores how humanitarian principles, even in the brutal context of war, can become the bedrock for future healthcare systems.
Wartime Advancements and the Transition to Civilian Care
The systematization of care for injured service members began during the Civil War (1861-1865), with rudimentary triage, aid stations, and rapid transport to field hospitals. During this period, President Abraham Lincoln initiated the creation of the first trauma manual, formally documenting processes for patient care. World War I brought significant medical and surgical advancements, including well-developed anesthesia methods and widespread availability of tetanus antiserum. Gunshot wounds were irrigated with antiseptic fluid (Carrel-Dakin treatment) to prevent gangrene. The practice of bringing researchers to the battlefield to study outcomes began during World War II, with many wartime advances serving as models for modern trauma systems.
The Vietnam War marked a pivotal moment with the maturation of rotary wing transportation, specifically helicopters. This development revolutionized combat medical care by dramatically reducing the time from wounding to surgical care from hours to minutes, thereby saving soldiers who would have perished in earlier conflicts. This innovation also compelled the civilian world to re-evaluate its concepts of triage for the injured. As war increasingly involved civilian population centers, triage extended into the entire medical community, necessitating the prioritization of wounded civilians. Collaboration between civilian and military health systems has a long history, spanning over a century, and has consistently advanced care during both peacetime and conflict.
The major advancements in the transportation of the wounded and in stabilization by medics with advanced capabilities seamlessly migrated from Vietnam to the home front, igniting a revolution in prehospital care. In the mid-1960s, Dr. R Adams Cowley pioneered one of the first civilian helicopter ambulance services in Baltimore. The publication of the groundbreaking 1966 National Research Council report, "Accidental Death and Disability: The Neglected Disease of Modern Society," catalyzed the rapid adoption of dedicated ambulances and standardized medical equipment. This led to trained, skilled medics triaging victims in non-urban areas, a significant improvement over the local hearse drivers who had previously provided civilian medical transportation services. Following the Vietnam War, triage began to assume its modern form, and methods for managing mass casualties in civilian settings started to be organized. In 1973, the Emergency Medical Services Systems Act further supported this transition by establishing a grant program for regional EMS systems, emergency medical technician (EMT) training, and the development of air transport services.
The catalytic role of conflict in healthcare innovation and systematization is evident throughout this period. The extreme pressures and high casualty rates of warfare create an urgent, unforgiving environment that compels rapid innovation and systematization in medical care. The military context serves as a crucible for testing and refining medical practices, which then migrate or foment a revolution in civilian healthcare. This suggests a cyclical relationship where military necessity drives innovation, which then diffuses into civilian practice, often formalized through legislation, such as the EMS Systems Act , and professionalization, like the establishment of EMT and paramedic services. The direct involvement of civilian populations in war further blurred the lines, necessitating the transfer of military medical expertise. This pattern highlights that systemic improvements in healthcare often arise from acute crises rather than solely from incremental peacetime development. It also underscores the critical importance of military-civilian collaboration for knowledge transfer and the development of robust, nationwide emergency response infrastructure. The shift from rudimentary "patching up" soldiers to advanced stabilization and rapid transport reflects a broader societal value placed on individual life, even in the context of mass casualties, and the recognition that rapid, organized care can significantly alter outcomes.
Emergence of Organized Emergency Medical Services (EMS)
The formalization of EMS and trauma systems in the United States began to take shape in the mid-20th century, heavily influenced by military advancements. The American College of Surgeons (ACS) played a significant role in this development. Its Verification Review Committee initiated on-site reviews for hospitals seeking trauma designation in the 1980s. Furthermore, the ACS created influential education programs, such as Advanced Trauma Life Support (ATLS), introduced in 1980, which teaches the immediate management of injured patients, including resuscitation, stabilization, triage, and transfer.
Despite these advancements, federal leadership in trauma systems has been inconsistent. Grant programs established to support these initiatives, such as the 1973 EMS Systems Act and the 2001 Healthcare Resources and Service Administration (HRSA) Trauma/EMS Systems Program, were later eliminated. Multiple reports over the past 50 years have consistently highlighted the persistent need for a cohesive national trauma system.
Triage itself began to emerge in emergency departments across the US, UK, and Europe in the early 1900s. During this period, it typically involved a brief clinical assessment to determine the appropriate time and sequence for a patient to be seen, given limited resources. In field settings, it guided the speed of transport and the choice of hospital destination for initial treatment. Modern healthcare systems have subsequently seen the emergence of three distinct phases of triage: first, prehospital triage, which focuses on dispatching ambulance and prehospital care resources; second, triage conducted at the scene by the first clinician attending the patient; and third, triage upon arrival at the emergency department or receiving hospital.
This historical progression reveals a paradox of progress: innovation versus sustained systemic implementation. Significant advancements in prehospital care and trauma systems occurred, often driven by military innovations. However, federal programs supporting these systems were eliminated, and a national trauma system has been called for over 50 years without full realization. This highlights a critical challenge in healthcare policy: the difficulty of translating proven innovations and recognized needs into sustained, federally supported, and integrated national systems. While individual advancements, such as ATLS , and regional initiatives improve care, the lack of consistent federal leadership creates gaps and fragmentation. This suggests that while medical science and clinical practice can evolve rapidly, political will, consistent funding, and long-term systemic commitment are often slower, more vulnerable to budgetary shifts, and subject to fluctuating priorities. This paradox implies that even with clear evidence of benefit and expert consensus on the need for a national system, the institutionalization of comprehensive healthcare infrastructure faces significant political, economic, and bureaucratic hurdles. This can lead to disparities in care quality and outcomes across different regions and populations without a robust, federally supported framework.
Core Principles and Objectives of Modern Triage
Ethical Foundations
Modern triage decisions are deeply rooted in several ethical frameworks, ensuring a delicate balance between individual patient needs and broader societal welfare. These principles collectively guide healthcare professionals in making complex prioritization decisions, particularly in high-stakes environments.
Utilitarianism and Distributive Justice: Triage fundamentally aims to maximize overall health benefits and minimize harm, striving for the greatest good for the greatest number of individuals. This principle is particularly salient in mass casualty situations, where the overarching goal is to save the largest number of lives in the shortest possible time. Complementing this, distributive justice focuses on the fair, equitable, and transparent allocation of limited resources, emphasizing that triage decisions must be just and unbiased.
Beneficence and Non-Maleficence: These are fundamental tenets of medical ethics, guiding healthcare professionals to act in the best interests of their patients (beneficence) while actively avoiding harm (non-maleficence). Triage decisions are thus made to provide care that is most likely to yield positive outcomes for patients and minimize adverse effects.
Autonomy and Patient-Centered Care: This principle recognizes the patient's inherent right to make informed decisions about their own care. While the urgent need for prioritization often exists, especially in emergency scenarios, healthcare professionals are tasked with balancing this imperative with respecting patient autonomy and involving them in decision-making processes whenever feasible.
The application of these principles often creates an inherent ethical tension in triage. While triage is guided by utilitarianism and distributive justice, which focus on population-level benefits, it also must contend with the individual-focused principles of beneficence and autonomy. This tension is particularly pronounced in mass casualty or severely resource-constrained scenarios. For instance, a patient categorized as "expectant" may not receive immediate care to maximize resources for others, directly challenging the principles of individual beneficence and autonomy. This ethical dilemma was starkly highlighted during the COVID-19 pandemic, when some countries were compelled to deny care to large groups of individuals due to severe shortages of supplies and ventilators. The deliberate separation of the triage role from the clinical treatment role in crisis situations is a direct attempt to mitigate this moral distress for clinicians and enhance the objectivity of resource allocation decisions. This ethical tightrope underscores that triage is not merely a clinical algorithm but a profound moral act. The continuous evolution of triage systems reflects ongoing societal and professional debates about how to balance these competing ethical demands, especially when resources are scarce. This necessitates robust ethical frameworks, transparent decision-making processes, and clear communication to maintain public trust and minimize moral distress for healthcare providers.
Primary Goals: Prioritization, Resource Allocation, and Patient Flow Management
The primary objectives of modern triage are multifaceted, extending beyond mere sorting to encompass comprehensive management of healthcare delivery. The main purpose of emergency department (ED) triage is to rapidly identify severely ill patients for prompt management, thereby allocating priorities according to the severity of their condition. This ensures that patients receive a level and quality of care precisely matching the urgency of their medical needs.
Beyond individual patient care, triage is vital for efficient management of overall patient flow, effective allocation of limited resources, and timely delivery of care within hospitals and emergency services. In mass casualty incidents (MCIs), the overarching goal of triage is to save the largest number of people in the shortest possible time. This involves quickly identifying victims who not only have immediately life-threatening injuries but also possess the best chance of survival with immediate intervention. Furthermore, triage systems facilitate systematic assessment and treatment, contribute to patient comfort and reassurance, enable thorough documentation of patient needs, and improve communication with patients and their caregivers regarding the nature of their problems and the subsequent process of medical care.
Key Modern Triage Systems: Methodologies and Applications
Overview of Triage Scales
Modern triage scales typically employ a system of 3 to 5 categories, utilizing algorithms, protocols, or specific diagnoses as reference points for decision-making. While numerous studies indicate that patient sorting depends on clinical characteristics, vital signs, and the severity of the condition, there is no single universal scale. Instead, systems are often adapted to specific regions and healthcare contexts. The evolution from simpler to more complex, multi-level systems reflects a continuous effort to balance the speed of assessment with accuracy and nuance in patient prioritization. While simpler systems are highly effective for rapid mass casualty sorting where speed is paramount, their limitations in non-mass casualty settings highlight the need for more detailed approaches. The more comprehensive systems aim to capture nuance but inherently require more training and time per patient, potentially impacting throughput in high-volume settings. This indicates that the "ideal" triage system is context-dependent, necessitating a strategic choice based on the specific operational environment. The ongoing development and adaptation of these systems underscore a continuous refinement process driven by the need to improve diagnostic accuracy and patient safety across diverse clinical scenarios, acknowledging that a "one-size-fits-all" approach is rarely optimal in healthcare.
Simple Triage And Rapid Treatment (START)
Methodology and Scoring Criteria: The START (Simple Triage And Rapid Treatment) system is primarily utilized by prehospital providers to categorize casualties during mass casualty events. It is designed for extremely rapid assessment, with the goal of determining triage status in less than 60 seconds per patient.
START divides casualties into four color-coded categories:
Expectant (Black): These individuals are either already deceased or are deemed likely to die despite medical treatment. This category includes those who are not breathing even after their airway has been repositioned.
Immediate (Red): These casualties have immediately life-threatening injuries and are likely to succumb without rapid intervention. They require advanced medical care within the hour.
Delayed (Yellow): These individuals have serious injuries but their treatment can be postponed for a period. They are in a stable condition but will require medical assistance.
Minor (Green): These casualties have injuries that do not require immediate prehospital treatment, and they are typically capable of transporting themselves to a medical facility. They are not evacuated until all immediate and delayed patients have been transported.
The algorithm, often remembered by the mnemonic "RPM" (Respirations, Perfusion, Mental Status), considers the following criteria:
Ability to Walk: Patients who are able to walk are immediately triaged as Minor/Priority 3.
Respirations: If a patient is not breathing, their airway is opened. If spontaneous breathing is still absent, the patient is categorized as DECEASED/EXPECTANT. If breathing is restored, the patient is IMMEDIATE. If breathing is present, the rate is checked: a rate greater than 30 breaths per minute indicates IMMEDIATE status. If the rate is less than 30 breaths per minute, Perfusion is assessed.
Perfusion: If a radial pulse is absent or capillary refill time is greater than 2 seconds, the patient is categorized as IMMEDIATE. If a radial pulse is present or capillary refill is less than 2 seconds, Mental Status is assessed.
Mental Status: If the patient cannot follow simple commands (indicating unconsciousness or altered level of consciousness), they are categorized as IMMEDIATE. If they can follow simple commands, they are DELAYED.
Application Contexts: START is primarily applied in mass casualty incidents (MCIs) where a limited number of rescuers must rapidly triage a large volume of patients without requiring specialized training. For pediatric patients, the Jump-START algorithm is commonly employed, which specifically accounts for the increased likelihood of respiratory failure in children and their potential inability to follow verbal commands.
Limitations: START has faced criticism for being difficult to implement accurately, as it requires precise assessment of parameters like respiratory rate or capillary refill in chaotic environments. A notable limitation of START is that all walking casualties are designated "minor" and directed to "secondary triage," even if they possess serious and potentially life-threatening injuries that may not immediately present with overt physiological distress, such as an isolated gunshot wound to the chest with normal vital signs. Additionally, certain conditions, such as burns, are not explicitly integrated into the core START algorithm.
Emergency Severity Index (ESI)
Methodology and Scoring Criteria: The Emergency Severity Index (ESI) is a widely adopted five-level triage acuity scale utilized in emergency departments (EDs) across the United States. Patients are classified and prioritized based on the severity of their condition and the estimated number of resources anticipated for their care.
The ESI employs decisive points where a trained nurse considers four key questions to classify patients:
Does the patient require a rapid, life-saving intervention?
Is this a patient who cannot wait for care?
How many resources will this patient likely need?
What are their vital signs?
Levels:
Level 1 (Highest Acuity): Patients requiring immediate, life-saving interventions.
Level 2 (High Acuity): Patients in high-risk situations or experiencing severe pain/distress, including stroke patients. They may require immediate intervention or can wait for up to ten minutes.
Level 3 (Moderate Acuity): Patients who will likely require multiple resources but have stable vital signs. They can be "up-triaged" to Level 2 if their vital signs fall into "danger zones" (e.g., abnormal respiratory rate, heart rate, or oxygen saturation).
Level 4 (Lower Acuity): Patients who are anticipated to require only one resource.
Level 5 (Lowest Acuity): Patients who are anticipated to require no resources.
Resources Considered (Examples from an adapted ESI scale): Laboratorial tests, electrocardiogram, ultrasonography, and radiological tests, intravenous hydration, intravenous drugs (if time of infusion is relevant), consultation with specialists, simple procedures (e.g., sutures, urinary catheterization delay), dressings (if a second application is needed), and inhalation treatments (only for a second dose).
Application Contexts: The ESI system is recommended for emergency departments, particularly those with high patient volumes. Its objective is to decentralize medical care, with an initial focus on efficiently managing low-complexity patients (Levels 3, 4, and 5) who typically consume fewer resources and rarely require hospitalization.
Limitations: The ESI score has shown poor correlation with serious outcomes in patients with suspected acute coronary syndrome, suggesting that it may not always accurately identify high-risk cardiac patients. Furthermore, higher acuity patients may occasionally face inappropriate stratification or experience longer waiting times due to the system's design or implementation challenges.
Canadian Triage & Acuity Scale (CTAS)
Methodology and Scoring Criteria: The Canadian Triage & Acuity Scale (CTAS) is a five-level scale widely used in prehospital care and emergency departments across Canada. Introduced in 1999, it has undergone several revisions to enhance its accuracy and reliability.
The determination of a CTAS level involves establishing a relationship between a patient’s presenting complaint (or chief complaint) and potential causes, defined as sentinel events, which are further refined by specific modifiers. The CTAS process is a four-step rapid evaluation and decision-making process, with an additional fifth step for infection control :
"Quick Look" / "Critical First Look": This is an initial 3-5 second scan upon patient arrival, primarily used for critically ill patients who appear in extremis. Its sole purpose is to quickly assign a patient directly to CTAS Level 1.
Screening for Infectious Diseases: Patients are screened for febrile respiratory illnesses and influenza-like illness to implement appropriate protective measures.
Interviewing and Assessing the Patient: This step involves gathering both subjective information (the patient's or caregiver's report of symptoms) and objective information (observable indicators, vital signs, pain severity, mechanism of injury, and other modifiers) to determine the presenting complaint using the Canadian Emergency Department Information System (CEDIS) list.
Modifiers: These provide additional acuity information and help assign the appropriate CTAS level.
First Order Modifiers are broadly applicable (e.g., respiratory distress, hemodynamic stability, level of consciousness, temperature, pain score, bleeding disorder, mechanism of injury).
Second Order Modifiers are more complaint-specific (e.g., blood glucose, obstetrics, mental health).
Making the Triage Decision and Assigning Acuity Level: Based on the critical look, subjective and objective assessments, and the application of modifiers, the triage nurse assigns one of the five CTAS levels. Nurse judgment also plays a role, allowing for "up-triaging" if clinical gestalt suggests a higher risk.
Levels (with Emergency Department reassessment times):
Level 1 (Resuscitation): Immediate threat to life or limb, requiring aggressive interventions (continuous nursing care).
Level 2 (Emergent): Potential threat to life, limb, or function, requiring rapid medical interventions (reassessment every 15 minutes).
Level 3 (Urgent): Could potentially progress to a serious problem, often associated with significant discomfort (reassessment every 30 minutes).
Level 4 (Less-Urgent): Conditions that would benefit from intervention or reassurance within one or two hours (reassessment every 60 minutes).
Level 5 (Non-Urgent): Acute but non-urgent, or part of a chronic problem; investigation or interventions could be delayed (reassessment every 120 minutes).
Application Contexts: CTAS is applied and documented a minimum of two times for prehospital care patients: an initial assessment upon arrival at the patient and a second assessment after interventions or at the time of departure. It covers a broad spectrum of emergency department presentations, including major to minor trauma, cardiovascular complaints, mental health problems, eye pain, obstetrical emergencies, and diverse pediatric presentations. For pediatric patients, CTAS incorporates the Pediatric Assessment Triangle (PAT).
Value: CTAS is structurally simple yet content-rich, making it conducive to computerization and capable of offering decision support at the point of care.
Manchester Triage System (MTS)
Methodology and Scoring Criteria: The Manchester Triage System (MTS) is a clinical risk management tool used globally by clinicians to manage patient flow when clinical need exceeds available capacity. It employs a reductive system featuring 53 Emergency Triage charts that are presentation-based, focusing on the patient's stated symptoms rather than a definitive diagnosis of the underlying cause. To ensure consistency, safety, and robust auditing, MTS utilizes common names, discriminators, and definitions.
The assessment is conducted immediately upon patient arrival, ideally before administrative tasks. This process leads to the allocation of a specific time window within which the patient should have their first contact with a physician. Symptoms are linked to fixed urgency groups with predefined timeframes, based on the likelihood of risk associated with that symptom. A particular symptom consistently receives the same urgency level, irrespective of the chosen presentation. Symptoms are also sorted by urgency within each level using the ABCDE scheme, rather than alphabetical order. If the initial time window for physician contact cannot be met, a secondary assessment is performed for documentation of patient observation, which can increase urgency if the patient's condition deteriorates.
Application Contexts: MTS is suitable for hospitals of all care levels and sizes, and can be effectively used in both dedicated emergency rooms (NA) and mixed elective/emergency outpatient clinics. The system was developed exclusively for registered Health Care Professionals (HCPs) due to the clinical skills and knowledge required for accurate triage assessment. MTS offers various specialized tools, including Emergency Triage, Telephone Triage, Pre-Hospital Pathfinder, Nursing and Residential Triage (NaRT), and Community Triage.
Value: The results of the initial MTS assessment can be used within the hospital to establish standard procedures, such as standard operating procedures, guidelines, or treatment pathways, for patients with specific chart-indicator combinations. This can lead to positive economic effects, increased patient satisfaction, and accelerated treatment. It also supports cooperation and similar actions in networks of smaller rural hospitals.
Table 1: Comparative Analysis of Key Modern Triage Systems
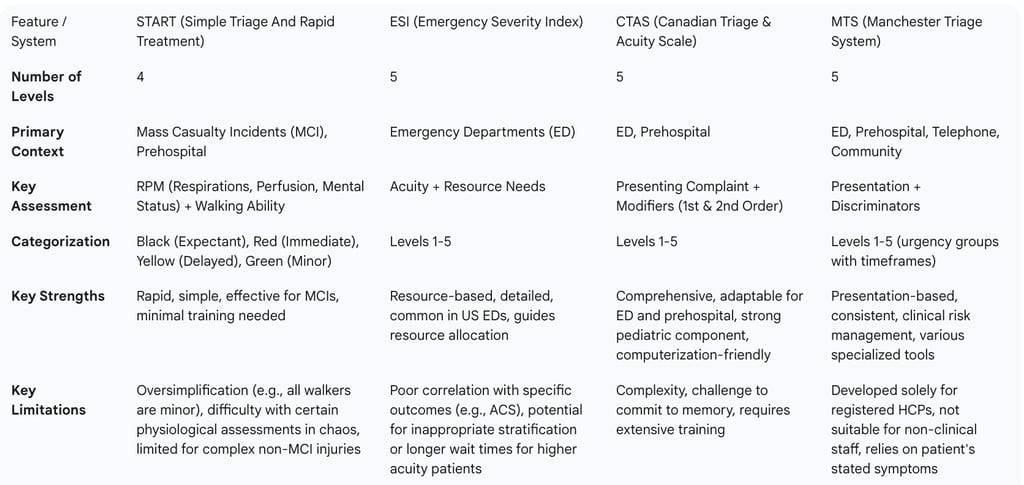
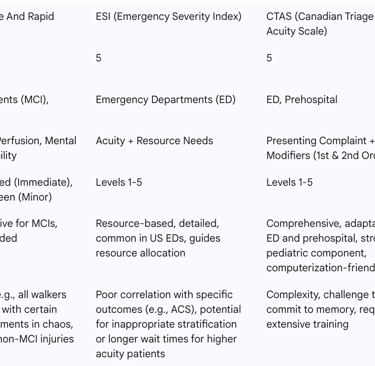
This comparative analysis highlights the distinct focuses and operational environments for which each system is best suited. The transition from simpler (START) to more complex, multi-level systems (ESI, CTAS, MTS) reflects a continuous effort to balance speed of assessment with accuracy and nuance in patient prioritization. While START is highly effective for rapid mass casualty sorting where speed is paramount, its "nuisance" of classifying all walking patients as minor underscores a critical limitation in non-MCI settings where complex or evolving injuries might not immediately present with overt physiological distress. The five-level systems, with their detailed modifiers, resource-based assessments, and presentation-based approaches, aim to capture this nuance but inherently require more training and time per patient, potentially impacting throughput in high-volume, non-MCI settings. This suggests that the "ideal" triage system is context-dependent, necessitating a strategic choice based on the specific operational environment (e.g., disaster field vs. busy urban ED). The ongoing development and adaptation of these systems (e.g., Jump-START for pediatrics ; CTAS revisions ) indicate a continuous refinement process driven by the need to improve diagnostic accuracy and patient safety across diverse clinical scenarios, acknowledging that a "one-size-fits-all" approach is rarely optimal in healthcare. This also implies a need for flexible training that addresses the nuances of each system and its appropriate application.
The Importance and Benefits of Effective Triage
Enhancing Patient Outcomes and Safety
Effective triage serves as a cornerstone of emergency care, as it is essential for appropriately assigning limited resources to meet often unlimited medical needs. It ensures that patients with life-threatening conditions are swiftly identified and prioritized for care. By enabling faster and more accurate initial assessments, triage leads to timely interventions, which in turn significantly improves patient outcomes. This proactive identification of high-risk patients and the subsequent prioritization of their care are critical in preventing adverse events and enhancing overall patient safety. Ultimately, this contributes to a reduction in morbidity and mortality rates. Digitally enabled triage, for example, further facilitates the earlier identification of "red flag symptoms" in the patient journey, allowing for quicker intervention and the prompt redirection of patients to emergency or community services through online consultation tools.
Optimizing Resource Utilization and Operational Efficiency
Triage is fundamental for managing the allocation of limited medical resources, a necessity particularly pronounced during emergencies, pandemics, or natural disasters. It plays a crucial role in optimizing resource allocation within healthcare facilities by providing predictive insights into patient flow and identifying potential bottlenecks. By accurately directing patients to the most appropriate care setting from the outset, effective triage significantly reduces unnecessary appointments and frees up valuable clinician time, allowing them to focus on more complex cases. Advanced triage systems lead to a more efficient use of medical resources, which in turn reduces congestion and wait times. This collectively enhances overall departmental efficiency and contributes to the cost-effectiveness of healthcare delivery.
Improving Patient Flow and Reducing Wait Times
Efficient triage streamlines the entire patient assessment process, directly contributing to a reduction in patient wait times. This not only improves patient satisfaction but also ensures that those with the most critical needs receive prompt attention. Conversely, prolonged waiting periods and extended patient stays in the emergency ward are frequently a consequence of inefficient workflow stemming from the absence of an effective triage unit to prioritize patients. Digitally enabled triage further enhances these efficiencies by allowing for the closure of consultations through written communication, eliminating the need for further telephone or face-to-face contact, and by automating booking flows where such features are available. Moreover, it broadens the variety of access options for patients seeking care, effectively removing existing barriers for certain patient groups.
The benefits of triage extend beyond individual patient care to the entire healthcare system's resilience and capacity. By acting as a "well-oiled machine" , effective triage prevents cascading failures, such as overwhelmed staff, resources tied up in non-critical cases, and delayed care for critical patients, all of which can severely cripple an emergency department or hospital. This systemic contribution is particularly evident during crises like the COVID-19 pandemic, where triage played a critical role in managing patient surges and allocating scarce resources like ventilators and ICU beds. The ability to manage patient flow and allocate resources efficiently directly contributes to the system's capacity to absorb shocks and maintain functionality under stress, thereby preventing system collapse. This highlights a symbiotic relationship between triage efficiency and system resilience, where a robust triage process is not just about individual patient outcomes but about the overall stability and responsiveness of the healthcare infrastructure.
Challenges and Limitations of Modern Triage
Despite its critical importance, modern healthcare triage faces several inherent challenges and limitations that can impact its effectiveness and patient experience.
Inter-Rater Reliability
One significant challenge is achieving consistent inter-rater reliability among healthcare professionals when assigning triage ratings to the same patient. This refers to the degree of variability in assessments made by different nurses or clinicians. Studies on scales like the South African Triage Scale (SATS) in low-resource settings have shown only "moderate" inter-rater agreement, with Intraclass Correlation Coefficient (ICC) values ranging from 0.50–0.60. While intra-rater reliability (consistency of one nurse over time) tends to be higher, variability among different assessors can lead to inconsistencies in patient prioritization. For a triage scale to be truly effective, it must yield the same rating on repeated assessments of the same patient, minimizing variability among different nurses. This variability can stem from factors such as lack of standardized training, subjective interpretation of symptoms, or the inherent pressures of a busy emergency environment.
Patient Perception and Satisfaction
Patient satisfaction with the triage process is a multidimensional concept influenced by several factors, including guiding, informing, psychosocial support, service speed, timing, and the competence of caregivers. Studies indicate that patients are generally satisfied with triage practices and nursing care. However, significant dissatisfaction arises from long waiting times for triage and treatment. Patients who reported not waiting for triage or receiving timely treatment according to their assigned category showed significantly higher satisfaction scores. Conversely, issues such as inadequate information about health conditions, lack of psychological support, and poor hygiene or sanitation can negatively impact patient satisfaction. The perception of unfair prioritization, such as "queue jumping" by others or preferential treatment for "VIP patients," also contributes to patient dissatisfaction and can undermine trust in the system.
Resource Constraints
Resource limitations pose a pervasive challenge, particularly in emergency departments and during public health emergencies. Many healthcare settings, especially in low- and middle-income countries, face severe constraints in human resources, infrastructure, and equipment, compounded by high patient volumes. This often results in an inadequate healthcare worker-to-patient ratio, where a single professional may be responsible for a large number of patients, hindering timely and personalized care. Limited beds and space can compel patients to share beds, particularly in less urgent triage areas, and inadequate waiting areas can create distressing conditions for patients and their companions. Insufficient medical equipment, such as a scarcity of ventilators, further exacerbates the challenge.
During public health emergencies, resource limitations necessitate a shift from individual patient-focused ethics to a population-focused approach, aiming for the greatest good for the greatest number. Critical care resources, like ventilators and beds, are allocated based on a framework designed to save the most lives and life-years. This framework is activated only when critical care capacity is overwhelmed despite all surge efforts, and a regional authority declares an emergency. Triage teams, separate from treating clinicians, are formed to ensure consistent and objective decision-making, applying allocation criteria based on likelihood of survival and life expectancy. The framework explicitly avoids discriminatory exclusions based on personal attributes like age, race, or socioeconomic status, ensuring all patients are assessed individually based on objective medical evidence. Reassessment for ongoing critical care is also crucial, allowing resources to be reallocated from patients with very low chances of survival to those more likely to benefit. For those not receiving critical care, palliative care and psychosocial support are mandated.
Challenges Related to Nursing Personnel and Management
The effectiveness of triage is heavily reliant on the competency and well-being of nursing personnel. A significant challenge is the lack of clinical competency among some triage nurses, who may lack adequate knowledge of disease physiopathology, high-risk emergencies, or the clinical skills to perform quick and accurate assessments of vital signs. This can lead to errors in patient prioritization, overcrowding, and patient dissatisfaction.
Another critical aspect is the lack of psychological capability. Triage nurses operate in a highly stressful and often chaotic environment, requiring emotional stability, high tolerance, and the ability to maintain mental concentration under pressure. Instances where nurses lose control or engage in arguments with patients and their companions negatively impact the quality of triage and patient satisfaction.
From a management perspective, human resource challenges are prominent, including staff shortages and heavy workloads that lead to fatigue and errors.
Structural challenges such as insufficient physical space and inadequate security contribute to overcrowding and disrupt nurses' work. Furthermore, performance challenges include a lack of motivation from administrators, an absence of specific instructions and policies for patient triaging, and insufficient specialized training workshops to empower triage nurses and keep their knowledge updated. These systemic deficiencies can undermine the effectiveness of even well-designed triage protocols.
The Role of Technology in Modern Triage
Technology, particularly Artificial Intelligence (AI), predictive analytics, and Electronic Health Records (EHRs), is rapidly transforming modern triage processes by automating patient assessment, enhancing decision-making, and optimizing hospital workflows.
AI and Predictive Analytics in Triage
AI-powered triage systems are revolutionizing the process by automating patient assessment, enhancing decision-making, and improving overall efficiency in emergency departments (EDs). These systems leverage machine learning (ML) and natural language processing (NLP) to analyze patient symptoms, medical history, and real-time clinical data. By implementing such intelligent systems, hospitals can reduce wait times, effectively allocate resources, and ensure critically ill patients receive timely medical attention. AI-driven triage systems address the limitations of traditional methods, which can be influenced by human variability, by analyzing vast amounts of patient data and identifying subtle clinical patterns that might be overlooked in manual assessments. For instance, AI can detect early signs of sepsis, myocardial infarction, or stroke by analyzing physiological parameters and symptom descriptions in real time.
Predictive analytics, a core component of AI-powered triage, can estimate the severity of incoming cases based on prehospital data, allowing ED teams to prepare for critically ill patients before their arrival. AI, through predictive analytics, can also forecast patient demand and optimize staffing schedules, as well as facilitate early discharge planning for stable patients, contributing to streamlined patient flow and reduced wait times. In primary care, AI triage optimizes patient flow by assessing symptoms and medical history to guide patients to the most appropriate care pathway, reducing unnecessary appointments and freeing up clinician time. This leads to shorter waiting lists and quicker access to care for those who truly need it. AI systems apply consistent rules and algorithms, leading to more standardized and potentially more accurate initial assessments compared to human triage, which can be influenced by subjective factors or workload pressures.
A UCSF-led study in 2024 found that an AI model was as effective as a physician in prioritizing patients in an ED setting. Using anonymized records of 251,000 adult ED visits, the AI correctly identified the patient with a more serious condition in 89% of matched pairs, compared to 86% for a physician in a sub-sample. This suggests AI could free up physician time and offer backup decision-making tools.
Electronic Health Records (EHRs) and Digital Tools
Electronic Health Records (EHRs) serve as the foundational infrastructure that AI systems need to interact with, acting as the primary source of patient data for AI analysis. Seamless integration of AI triage systems into existing hospital workflows is a key challenge, particularly given the variety of EHR systems used across healthcare facilities. The effective integration of AI with EHRs is crucial for AI to access and process patient information, thereby enabling its capabilities in improving triage accuracy, reducing wait times, and optimizing resource allocation.
Digital tools, such as virtual triage platforms, are increasingly prevalent. Clearstep's Smart Access Suite, for instance, is an AI-powered symptom checker and healthcare navigation assistant that allows patients to input symptoms and receive personalized guidance within 1-3 minutes. It offers 24/7 self-service symptom assessments, aims to eliminate long wait times, and routes patients to the most clinically appropriate resources based on evidence-based Schmitt clinical content. TriageGO is another AI-powered tool that optimizes triage by providing acuity-level recommendations based on the risk of various clinical outcomes, demonstrating significant reductions in length-of-stay and time to critical care interventions. These tools capture valuable data, reduce staff workload, and enhance patient access and satisfaction.
Challenges in Technology Adoption
Despite the immense promise of AI and digital tools in triage, their implementation is not without challenges. Data quality and integration are paramount, as AI models are only as effective as the data they are trained on. Ensuring high-quality, unbiased data and seamless integration with existing EHRs is crucial.
Algorithmic bias is a significant concern; if training data contains biases, the AI's recommendations could perpetuate or even amplify existing healthcare disparities, necessitating continuous monitoring and ethical oversight.
Clinician trust and adoption are vital for successful implementation. Healthcare professionals need to perceive AI as a supportive tool rather than a replacement for clinical judgment, requiring comprehensive training and clear communication about AI's role.
Patient acceptance and digital literacy also present hurdles, as not all patients are comfortable with or have access to digital tools, necessitating equitable access and support. Finally,
regulatory and ethical frameworks for accountability, data privacy (e.g., HIPAA compliance), and transparency regarding the "black box" nature of some AI decisions are still evolving. While AI shows promise, further validation and clinical trials are necessary before widespread responsible use in critical settings like the ED.
Conclusions
The evolution of healthcare triage, from its rudimentary origins on Napoleonic battlefields to its sophisticated modern applications, reflects a continuous adaptation to the complex demands of medical care. Initially driven by military necessity to maximize fighting force, triage underwent a profound ethical transformation, shifting towards a humanitarian principle of prioritizing care based on injury severity regardless of rank or nationality. This ethical foundation remains central to modern triage, guiding decisions through principles of utilitarianism, distributive justice, beneficence, non-maleficence, and patient autonomy, even as these principles can present inherent tensions in resource-constrained environments.
Modern triage systems, such as START, ESI, CTAS, and MTS, each offer distinct methodologies tailored to specific contexts, from mass casualty incidents to routine emergency department operations. While simpler systems prioritize speed, more complex multi-level systems aim for greater diagnostic accuracy and nuanced patient prioritization. The choice and effective implementation of these systems are critical for optimizing patient outcomes, enhancing patient safety, and improving the overall efficiency and resilience of healthcare systems. Efficient triage directly contributes to reduced wait times, streamlined patient flow, and optimized resource allocation, preventing systemic overload and improving the cost-effectiveness of care delivery.
However, significant challenges persist, including variability in inter-rater reliability, which can lead to inconsistencies in patient prioritization. Patient satisfaction, while generally positive, is heavily influenced by factors such as waiting times, the quality of information provided, and perceptions of fairness in resource allocation. Resource constraints, particularly in terms of human capital, infrastructure, and equipment, continue to impede optimal triage performance, especially during public health emergencies where difficult ethical decisions regarding resource rationing become unavoidable. Furthermore, issues related to nursing competency, psychological resilience, and management support directly impact the quality and consistency of triage practice.
The advent of technology, particularly Artificial Intelligence and predictive analytics, offers transformative potential for modern triage. These tools can enhance assessment accuracy, predict patient deterioration, reduce wait times, and optimize resource distribution by analyzing vast amounts of patient data from Electronic Health Records. Virtual triage platforms are already improving patient access and streamlining initial patient navigation. Despite these advancements, the successful integration of AI requires careful navigation of challenges such as data quality, algorithmic bias, and the crucial need to foster trust among clinicians and patients.
In conclusion, modern healthcare triage is a dynamic, ethically complex, and indispensable process that continuously evolves to meet the ever-growing demands on healthcare systems. Its ongoing importance lies in its ability to balance individual patient needs with population-level resource management, ensuring equitable and efficient care delivery. The future of triage will undoubtedly be shaped by continued research, refinement of existing methodologies, and the responsible integration of advanced technologies, all aimed at strengthening healthcare system resilience and ultimately improving global health outcomes.
FAQ Section
What is triage in healthcare?
Triage in healthcare is a systematic approach to evaluating and categorizing patients based on the severity of their conditions. This ensures that those with the most urgent needs receive immediate attention, optimizing the use of medical resources and improving patient outcomes.
When was triage first introduced in civilian healthcare?
Triage was formally introduced in civilian healthcare in 1964 when Weinerman et al. published a systematic interpretation of emergency department (ED) triage.
What are the three main phases of triage?
The three main phases of triage are prehospital triage, triage at the scene, and triage upon arrival at the emergency department.
What is the Emergency Severity Index (ESI)?
The Emergency Severity Index (ESI) is a five-level triage system that categorizes patients based on the severity of their condition and the resources they are expected to need. It is widely used in the United States and other countries.
What is the Canadian Triage and Acuity Scale (CTAS)?
The Canadian Triage and Acuity Scale (CTAS) is a five-level system used in Canada that categorizes patients based on the severity of their condition and the urgency of their need for medical intervention.
What is the Manchester Triage System (MTS)?
The Manchester Triage System (MTS) is a system used in the United Kingdom and other countries that categorizes patients based on their presenting complaint and the associated urgency.
What is the Australasian Triage Scale (ATS)?
The Australasian Triage Scale (ATS) is a five-level system used in Australia and New Zealand that categorizes patients based on the maximum waiting time for medical assessment and treatment.
What are some challenges faced in triage?
Some challenges faced in triage include ensuring accuracy and consistency in assessments, balancing resource allocation, and maintaining clear communication and handover between healthcare providers.
How does training and education impact triage accuracy?
Regular training and education on triage systems and protocols can significantly improve triage accuracy. A single presentation explaining the logic and characteristics of triage systems has been shown to increase the likelihood of correct patient triage.
Why is effective triage important in emergency departments?
Effective triage is important in emergency departments because it optimizes patient flow, reduces waiting times, and ensures that critical patients receive timely care. This helps to improve patient outcomes and prevent overcrowding.
