The Environmental Footprint of Healthcare Triage
Healthcare is essential for human well-being, yet it carries a significant environmental footprint. The sector contributes to various pollutants that negatively impact health, creating a paradox where healthcare services indirectly harm the environment and, consequently, public health.


Despite healthcare's mission to heal, its operational model significantly contributes to climate change and environmental degradation. Triage decisions, particularly inaccuracies like overtriage and undertriage, amplify this burden through unnecessary resource consumption, increased waste generation, and prolonged care pathways. The report explores the quantifiable environmental costs associated with these inefficiencies, such as substantial greenhouse gas emissions from diagnostic imaging and laboratory tests. Crucially, it highlights the transformative potential of digital health technologies, including telehealth and AI-driven triage, in mitigating these impacts by optimizing patient flow, reducing travel, and streamlining resource utilization. The report also emphasizes the necessity of integrating triage-specific sustainability efforts within broader healthcare greening initiatives, advocating for systemic changes in procurement, energy management, and waste reduction. The analysis concludes with actionable recommendations for policymakers, administrators, and clinicians, underscoring the imperative for robust measurement methodologies like Life Cycle Assessment (LCA) to guide a more environmentally responsible and resilient healthcare future.
Healthcare's Environmental Imperative
Healthcare, a sector dedicated to human well-being, paradoxically exerts a substantial and growing burden on the natural environment. Understanding this complex relationship is foundational to developing truly sustainable healthcare systems. This section defines the environmental footprint of healthcare, quantifies its global and national contributions to environmental degradation, and introduces the critical role of triage within this context.
1.1 The Global and National Healthcare Environmental Footprint
The Healthcare Environmental Footprint is defined as the total sum of environmental pressures stemming from the entire lifecycle of healthcare activities. This encompasses everything from the manufacturing of medical supplies and pharmaceuticals to the energy consumed by hospitals and the disposal of medical waste. This fundamental definition includes resource depletion, pollution generation, and contributions to climate change directly attributable to medical operations.
Globally, healthcare services are estimated to be responsible for approximately 4.4% of global greenhouse gas (GHG) emissions, a figure that can rise to 10% in high-income countries. If the global healthcare sector were considered a nation, it would rank as the
fifth-largest emitter of greenhouse gases globally. In the United States, the healthcare sector bears an even higher share, accounting for
8.5% of national GHG emissions. This share has been increasing, with emissions rising 6% from 2010 to 2018. Beyond GHGs, the U.S. health care sector is responsible for significant fractions of national air pollution emissions and impacts, including 12% of acid rain, 10% of smog formation, and 9% of criteria air pollutants. In England, the National Health Service (NHS) contributes 3.2% of the country's total CO2 emissions.
The primary drivers of this substantial environmental footprint are multifaceted:
Energy Use: Hospitals operate continuously, demanding massive amounts of energy for heating, cooling, lighting, and specialized medical equipment. A significant portion of this energy originates from non-renewable sources, leading to substantial greenhouse gas emissions. Operating rooms are particularly energy-intensive spaces within hospitals. Furthermore, clinical laboratories exhibit high energy consumption, utilizing 3-6 times more energy than typical office buildings. Energy consumption alone accounts for 22% of NHS CO2 emissions.
Procurement and Supply Chain: The acquisition of goods and services, including pharmaceuticals, medical devices, food, and textiles, represents a large upstream environmental impact. Healthcare supply chains globally account for an estimated 60-80% of the health sector's carbon footprint. For NHS England, medicines, medical equipment, and other purchased goods and services constitute 66% of its total carbon footprint. These are largely indirect, or Scope 3, emissions, generated during the production and transportation phases of supplies.
Waste Management: Healthcare facilities generate millions of tons of waste annually. This includes diverse waste streams, ranging from general trash to regulated medical waste, hazardous chemicals, and radioactive materials. Improper handling and disposal can lead to soil, water, and air contamination. The treatment of healthcare waste, particularly through incineration, is energy-intensive and produces highly hazardous gases and compounds, including hydrochloric acid, dioxins, furans, and toxic metals like lead, cadmium, and mercury. Methane, a greenhouse gas 21 times more potent than carbon dioxide, is also produced from solid waste disposal. For example, tertiary hospitals in South Korea generate an average of 1.2 tons of medical waste per day , while in the U.S., hospitals generate about 33.8 pounds of waste per day, totaling approximately 6 million tons annually.
Transportation: The travel of patients, healthcare workers, and medical supplies to and from care settings contributes significantly to air pollution and carbon emissions. Patient healthcare-related travel in the U.S. alone generates approximately 35.7 megatons of CO2e annually, accounting for about 6% of the nation's total healthcare-related emissions. In England, patient, visitor, and staff travel collectively account for 14% of the health system's total emissions.
A critical observation emerges when examining healthcare's environmental footprint: the sector's core mission to heal human beings stands in stark contrast to its operational impact on planetary health. The very act of providing care contributes to the degradation of the environmental systems upon which collective health ultimately depends. This presents a profound paradox, as healthcare-related pollution can paradoxically worsen many of the diseases healthcare professionals tirelessly work to treat and cure. This inherent tension necessitates a fundamental re-evaluation of healthcare's operational paradigms. Environmental sustainability cannot be viewed as an external obligation but must be inextricably linked to public health and integrated into the core mission of care delivery. Achieving true public health requires addressing the environmental determinants of health, which inherently includes mitigating healthcare's own ecological burden. This implies a shift beyond a purely curative model to one that actively promotes planetary health as a prerequisite for human health.
Furthermore, while visible aspects like energy consumption within facilities and direct waste generation are often the focus of sustainability initiatives, a deeper analysis reveals a critical blind spot: the overwhelming majority of healthcare's environmental burden originates upstream in its supply chain. Procurement and the supply chain account for an estimated 60-80% of the health sector's carbon footprint globally. This substantial proportion, representing the environmental toll of production, packaging, and transport of goods and services before they even reach the hospital, is a large upstream impact. This means that focusing solely on "in-house" operational efficiencies, such as hospital energy consumption or waste segregation, will only address a fraction of the total environmental burden. True decarbonization of the healthcare sector demands a strategic and profound engagement with global supply chains, advocating for verified environmental disclosures from suppliers, prioritizing sustainable sourcing, and exploring opportunities for localized procurement where feasible. This shifts the focus from direct control within healthcare facilities to influencing the broader industrial ecosystem that supports healthcare delivery.
1.2 Understanding Healthcare Triage
Triage is a cornerstone of modern healthcare, particularly in emergency and high-demand settings. Originating from the French word "trier," meaning to sort and organize, triage is the process of categorizing patients based on the severity of their injuries or illnesses to determine the order in which they require care and monitoring.
The universal goal of triage is to supply effective and prioritized care to patients while optimizing resource usage and timing. This involves identifying those who need immediate intervention, those who can wait, and, in some contexts, those for whom nothing can be done. The historical roots of emergency triage trace back to military medicine, developed by French military surgeon Baron Dominique Jean Larrey to quickly evaluate and categorize wounded soldiers during battle. Its first implementation in civilian hospitals occurred in 1964.
In practice, triage systems, such as the Emergency Severity Index (ESI), START (Simple Triage And Rapid Treatment), Jump-START, and SALT (Sort, Assess, Life-saving interventions, Treatment/Transport), utilize various criteria to assign priority levels. These criteria often include vital signs like pulse, respiratory rate, and capillary refill time, as well as the presence of bleeding and the patient's ability to follow commands. It is important to note that triage is a dynamic process, meaning a patient's status can change over time, necessitating re-evaluation. While a human-driven process, triage aims for the optimal allocation of human and physical resources, ensuring that the sickest patients receive care first.
The inherent function of triage as a mechanism for "optimizing resource usage and timing" and for achieving "the best allocation of human and physical resources" highlights its fundamental role beyond mere clinical assessment. This means that triage is not simply a medical decision point but a critical operational lever for managing the flow and consumption of resources within a healthcare system. Given healthcare's substantial environmental footprint, any process that directly influences resource allocation, such as triage, becomes a pivotal point of intervention for sustainability. Accurate and efficient triage can prevent the unnecessary expenditure of resources, thereby directly contributing to a reduced environmental burden. This connection firmly establishes triage as a strategic area where improvements can yield tangible environmental benefits, making it a key focus for "greening" healthcare operations.
2. The Environmental Implications of Triage Decisions
Triage decisions, while essential for patient safety and operational efficiency, carry significant environmental implications that are often overlooked. Inaccuracies in this critical process, specifically overtriage and undertriage, lead to a cascade of events that increase resource consumption, generate excess waste, and ultimately inflate healthcare's environmental footprint.
2.1 Impact of Overtriage
Overtriage occurs when patients are assigned a higher acuity level than their actual condition warrants. This means that mild cases are classified as severe, leading to less critical patients being seen before those with more urgent needs.
The operational consequences of overtriage are significant. It can slow down patient care in the emergency department (ED) and risk the unnecessary use of hospital resources. When patients with more stable conditions occupy resources such as examination rooms, staff time, and diagnostic tests, these resources become unavailable for critical patients who may need them more urgently. This leads to inefficient resource allocation, contributing to overcrowding and work overloads in specific units. In extreme scenarios, such as mass casualty events, overtriage can severely impact patient care and survival by inundating already overwhelmed medical facilities with a large number of non-critical casualties, potentially preventing the timely detection and treatment of those truly critical.
The environmental costs associated with overtriage are quantifiable and substantial:
Unnecessary Diagnostic Imaging: Estimates suggest that excess imaging ranges from 4-30% of all imaging exams. The total yearly estimated greenhouse gas (GHG) emissions from all
inappropriate imaging exams in the Medicare Part B population between 2017 and 2021 were between 3.55 and 129.2 kilotons of CO2e per year. This considerable figure is equivalent to the CO2 emissions from powering a town of over 70,000 people for a year. Unnecessary CT exams contributed approximately half of these excess emissions, with MRI accounting for another quarter. It is important to note that these emissions calculations include not only the energy consumed during an exam but also the energy required when scanners are in stand-by mode or during their production phase between scans.
Unnecessary Laboratory Tests: A study revealed that 76% of evaluated patients underwent unnecessary bloodwork, resulting in a mean of 1.84 phlebotomies, 4.4 blood vials, and 16.5 tests per patient. The environmental cost of these unnecessary activities was 61 kg CO2e (974 g CO2e per person) in the sample study population. The manufacturing of consumables and the processing of laboratory tests accounted for the majority (92%) of GHG emissions from these tests. A single phlebotomy alone was estimated to generate 150 g CO2e, and a common set of investigations (complete blood count, differential, creatinine, urea, sodium, potassium) had a carbon footprint of 332 g CO2e. Given that millions of tests are performed annually, and 12-44% of ordered pathology tests are not clinically indicated, reducing unnecessary testing represents the most effective approach to reducing the carbon footprint of pathology.
Connection to "Low-Value Care": Overtriage directly contributes to "low-value care," which is defined as medical treatments offering minimal or no benefit to patients while potentially posing harm at a high cost. It is estimated that up to 30% of investigations and treatments ordered in the healthcare system are unnecessary. Low-value care generates carbon emissions, waste, and pollution without improving patient or population health. In Australia, for instance, 8,585 kilotonnes of clinical care's carbon footprint are attributed to low-value care. Unnecessary care carries an enormous environmental cost due to the energy and resources required for the entire lifecycle of materials: from extraction and processing to manufacture, packaging, transport, and ultimate disposal.
The analysis of overtriage reveals its role as a direct driver of "low-value" environmental impact. The evidence clearly links overtriage to "unnecessary use of hospital resources" and "patients spending more time in the ED and more hospitalizations". This aligns perfectly with the definition of "low-value care" as interventions offering "minimal or no benefit" but incurring "high cost". Furthermore, the environmental costs of low-value care are explicitly stated to be "enormous" due to the full lifecycle impact of resources. The quantified data on unnecessary imaging (up to 129.2 kT CO2e/year) and lab tests (974 g CO2e/person) directly illustrate this ecological burden. Therefore, overtriage is not merely an operational inefficiency but a significant upstream contributor to healthcare's environmental footprint by generating "low-value" care. By misclassifying patients, it triggers a cascade of unnecessary diagnostic tests, procedures, and prolonged resource utilization, each carrying a substantial carbon and waste burden. Consequently, improving triage accuracy is a crucial, preventative strategy for reducing low-value care and its associated environmental impact, offering a direct pathway to more sustainable healthcare delivery.
Moreover, the environmental impact of overtriage extends beyond the immediate resource consumption of a single unnecessary test or procedure; it initiates a compounding effect of unnecessary diagnostics. The data on excess imaging and unnecessary laboratory tests quantify their individual carbon footprints. However, the literature further explains that "unnecessary testing can lead to false-positive results, further unnecessary interventions, overdiagnosis, anxiety, and overtreatment". These are described as "cascading down-stream investigations". This means that an initial low-value intervention can lead to subsequent, potentially more intensive and resource-demanding, investigations and treatments. This compounding effect significantly amplifies the overall environmental burden, emphasizing that accurate triage acts as a critical gatekeeper, preventing an escalating chain of environmentally costly clinical activities.
2.2 Impact of Undertriage
Undertriage occurs when patients are assigned an inadequately low triage level, underestimating the severity of their illness. This results in patients with more critical conditions waiting longer for care, potentially leading to adverse outcomes.
The operational consequences of undertriage are severe. It increases the patient's risk for health status deterioration while waiting. This can lead to delayed care, prolonged ED stays, and adverse events, such as delaying the transfer of critically ill patients to the intensive care unit. Patients who are undertriaged and placed in lower acuity pods, often distant from the main ED, are particularly at risk of harm. Ultimately, triage errors, including undertriage, contribute to patients spending more time in the ED and requiring more hospitalizations.
While direct quantifiable environmental costs of undertriage in terms of specific CO2e emissions or waste volumes are not extensively detailed in the provided literature, the operational consequences clearly imply significant indirect environmental impacts:
Increased Resource Consumption due to Escalated Care: When a patient's health deteriorates due to undertriage, they often necessitate more intensive, resource-heavy interventions later in their care pathway. This could involve more complex diagnostic procedures, higher-acuity interventions (e.g., surgery, mechanical ventilation), and transfer to specialized units like intensive care units (ICUs), all of which are inherently highly resource-intensive operations.
Prolonged Hospital Stays: Patients experiencing delayed care or deterioration due to undertriage are likely to have longer lengths of stay in the ED and/or require more prolonged hospitalizations. Prolonged hospital stays inherently consume more energy (for lighting, heating, cooling, and operating equipment), more water (for sanitation and medical procedures), and generate significantly more waste (medical waste, food waste, laundry). The literature explicitly states that reducing healthcare's carbon footprint requires radical reform of care pathways so that only patients whose healthcare cannot safely be delivered closer to home are admitted or remain in the hospital.
Increased Waste Generation: More complex and prolonged care directly translates to increased consumption of disposable medical supplies, pharmaceuticals, and other materials, thereby contributing to higher volumes of medical and general waste.
Undertriage, while perhaps not immediately appearing as wasteful as overtriage, can lead to a more severe and prolonged environmental impact by escalating the level of care required. When a patient's condition deteriorates due to an initial underestimation of severity, they often require a higher intensity of care, which is inherently more resource-intensive. A patient who could have been treated with fewer resources if accurately triaged might later require ICU admission, multiple complex procedures, and extended hospitalization, each exponentially increasing the environmental burden in terms of energy, water, and waste. This reality underscores that accurate triage is paramount for sustainability, not solely to prevent over-treatment, but also to prevent the escalation of care needs and their associated environmental costs.
2.3 Overall Impact on Resource Utilization and Waste Generation
Beyond the specific impacts of triage errors, the emergency department (ED) environment and the broader healthcare system's operational characteristics inherently contribute to a significant environmental footprint, which triage decisions directly influence.
Emergency departments are particularly relevant to healthcare's environmental footprint due to their unique operational demands. They typically operate round the clock, utilize energy-intensive diagnostic modalities such as computed tomography (CT), and rely heavily on disposable equipment for rapid turnover and infection control. The average emission intensity in U.S. emergency rooms is 51 Kg CO2 per patient , with electricity consumption consistently emerging as the primary source of emissions across most ERs. More broadly, hospitals demand massive amounts of energy for heating, cooling, lighting, and specialized medical equipment , and operating rooms are among the most energy-intensive spaces. Clinical laboratories also exhibit high energy consumption, using 3-6 times more energy than typical office buildings.
Healthcare facilities contribute significantly to medical waste streams, generating millions of tons of waste annually. This includes diverse waste streams, from general trash to regulated medical waste, hazardous chemicals, and radioactive materials. Improper handling and disposal can lead to soil, water, and air contamination. Waste treatment, particularly incineration, is energy-intensive and produces a range of hazardous gases and compounds, including hydrochloric acid, dioxins, furans, and toxic metals. Methane, a potent GHG, is also produced from solid waste disposal. Over half the world's population is reportedly at risk from the health impacts of healthcare waste. The sheer volume of disposables used in patient care, especially plastics, is a major concern; while research suggests 85% of plastics waste could be recycled, 91% still end up in landfills or natural environments.
Emergency physicians, through their clinical decisions, serve as stewards of resources, including investigations, medications, and patient disposition. Their decisions significantly contribute to healthcare emissions. It is notable that low-value or harmful interventions contribute up to 40% of the carbon footprint associated with clinical care. This highlights that reducing unnecessary care is a critical step physicians can take to reduce GHG emissions.
The unique operational demands and criticality of emergency care create inherent environmental challenges, making the ED an environmental hotspot. The 24/7 operation, reliance on energy-intensive diagnostic modalities like CT, and extensive use of disposable equipment for rapid turnover and infection control all contribute disproportionately to healthcare's environmental footprint. The quantifiable average emission intensity of 51 Kg CO2 per patient in U.S. ERs further solidifies this observation. This suggests that generic hospital-wide sustainability policies may not be sufficient for EDs. Targeted interventions and design considerations specifically for the ED environment, such as optimizing energy use for imaging equipment during low-demand periods and promoting reusable instruments where infection control protocols allow, are crucial for achieving meaningful reductions in the sector's overall footprint.
Furthermore, the environmental impact in healthcare is not a set of isolated problems but a complex, interconnected system. The research demonstrates a clear interplay between waste generation, energy consumption, and clinical decisions. For example, waste treatment, particularly incineration, is energy-intensive and produces pollutants. The choice between single-use and reusable medical items directly impacts waste volume and associated energy and resource use. Similarly, clinical decisions, such as ordering unnecessary tests, directly generate waste from consumables and consume energy for processing. This means that efforts to reduce waste must be linked to energy efficiency, sustainable procurement practices, and fundamental changes in clinical practice. For instance, promoting reusable items not only reduces waste but also lessens the energy associated with manufacturing and disposal, while reducing unnecessary tests decreases consumable waste and the energy required for their processing. This necessitates a shift in mindset from managing separate "environmental issues" to integrating sustainability into every facet of care delivery and operational planning.
3. Strategies for Sustainable Healthcare Triage
Addressing the environmental footprint of healthcare triage requires a multi-pronged approach that encompasses optimizing triage accuracy, leveraging technological innovations, and integrating broader sustainable healthcare practices.
3.1 Optimizing Triage Accuracy and Efficiency
Accurate triage is critical for proper patient assessment and efficient patient flow. However, triage is a complex and error-prone process, with both undertriage and overtriage occurring in practice. Strategies to optimize nursing practices and improve triage accuracy include audit and feedback mechanisms, targeted education, reminder systems, and simulation-based training. Serious games, for instance, can simulate realistic situations to evaluate triage performance in a safe environment.
Streamlining patient flow and reducing overcrowding are also paramount. Overcrowding is a significant challenge in emergency departments , and inaccurate triage contributes to patients spending more time in the ED and requiring more hospitalizations. Optimizing patient flow is essential for timely, high-quality care, and mismanagement can cause disruptions throughout the hospital system. Innovative strategies such as "split flow" and "vertical flow" models can significantly improve throughput for non-critical and ESI 3 patients, reducing physical space limitations within the ED. Additionally, implementing secondary triage systems, especially with the presence of a physician during peak hours, has been shown to reduce the length of stay for non-critical cases and decrease the rate of patients who "left without being seen".
The emphasis on improving human performance and optimizing operational processes within triage directly contributes to environmental sustainability. The literature highlights that triage is "complex and error-prone," with environmental factors like noise and interruptions potentially affecting accuracy. Strategies such as education, reminder systems, and simulation training are proposed to enhance accuracy. Concurrently, operational changes like "split flow" and "secondary triage" are implemented to improve patient flow. By reducing errors in triage (both over- and under-triage) and improving patient flow, these strategies inherently minimize unnecessary resource consumption, reduce prolonged patient stays, and alleviate overall system strain. This indirectly but significantly lowers the environmental footprint of healthcare delivery. This perspective underscores the importance of investing in staff training, workflow redesign, and decision support mechanisms as integral sustainability measures, recognizing that human factors and systemic efficiency are powerful environmental levers.
3.2 Leveraging Digital Health Technologies
Digital health technologies offer transformative potential in mitigating the environmental footprint of healthcare triage.
Telehealth: Telehealth significantly reduces transport-associated carbon emissions, fuel consumption, paper waste, and the consumption of personal protective equipment (PPE). Patients can avoid physical travel to appointments. A UC Davis Health study quantified these benefits, reporting 53.7 million miles saved, 204 years of travel time saved, and $33.5 million in travel costs saved over two years, resulting in a reduction of 21,466 metric tons of CO2e. This CO2e saving is equivalent to a year's emissions from 4,177 U.S. homes. Telehealth also decreases the demand for physical office space, leading to reduced energy use in healthcare facilities. It promotes digital record-keeping, thereby cutting down on paper waste, and reduces the need for disposable medical supplies associated with in-person visits. However, it is crucial that telehealth provision includes careful clinical triaging to ensure its benefits outweigh any potential drawbacks, and it should primarily serve as a medium within longitudinal care rather than for acute care or new patient settings.
Telehealth emerges as a multi-faceted environmental solution. The concrete, quantifiable data demonstrating how telehealth reduces patient travel (53.7 million miles, 21,466 metric tons CO2e) , decreases paper waste, and even lessens the need for physical facility space and disposable supplies is compelling. This means telehealth is not merely a convenience or access solution; it is a powerful environmental sustainability tool. Its benefits extend across multiple domains of healthcare's environmental footprint, from direct emissions (transportation) to indirect impacts (reduced facility energy consumption, less waste from disposables). This positions telehealth as a high-impact intervention for greening healthcare, particularly when integrated into triage processes to divert unnecessary in-person visits.
AI-Driven Triage: The integration of artificial intelligence (AI) into triage systems enhances patient prioritization through data-driven decision-making. AI-driven triage improves consistency, optimizes resource allocation, and reduces waiting times. These systems rapidly analyze multiple data points for quicker, more accurate patient assessment , identifying high-risk patients for early intervention. Studies indicate AI-driven triage can reduce wait times by up to 30%. AI can dynamically adjust patient prioritization based on ED capacity and resource availability, optimizing workflows and minimizing congestion. It supports clinicians by reducing their cognitive burden. AI can predict bed needs and resource allocation, thereby saving resources , and optimize diagnostic tests and predict admission rates, minimizing waste. For example, AI-powered operating theaters have been shown to reduce energy consumption by 25% in a Caresyntax study. However, it is important to consider that training large AI models can consume significant energy, and the environmental benefits must outweigh the energy consumed by the AI systems themselves. Challenges also include data quality, algorithmic bias, and ensuring clinician trust.
AI's application in healthcare triage presents a dual environmental impact, necessitating a "Green AI" approach. While AI can significantly "lower energy consumption and reduce waste" in clinical settings, such as the 25% reduction in operating room energy consumption achieved through AI-powered systems , the underlying digital infrastructure of AI itself has a growing carbon footprint. The question of whether AI utilization has a substantial environmental footprint, particularly from the energy consumed by training large AI models, is a valid concern. The broader ICT footprint, encompassing data centers, computer networks, hardware production, and data storage/transfer, contributes significantly to emissions, with ICT potentially accounting for 14% of GHG emissions by 2040. Therefore, to ensure that the environmental benefits of AI in healthcare are not offset by its own computational demands, a "green AI" approach is essential. This involves focusing on energy-efficient algorithms, developing sustainable data centers, and promoting circular design principles for hardware.
Smart Triage Systems: These autonomous patient triaging systems improve patient access and enhance demand and capacity management. They automate triage and appointment booking, with one system achieving 91% auto-allocation of appointments. Such systems can significantly reduce phone calls (e.g., 47% fewer at peak hours) and decrease patient wait times (e.g., a median reduction of eight days for pre-bookable appointments). They also promote more sustainable staff working patterns and improve the utilization of healthcare professionals. Beyond patient flow, precision triage systems can reduce electronic waste by extending the lifespan of mobile devices through promoting reuse and refurbishment.
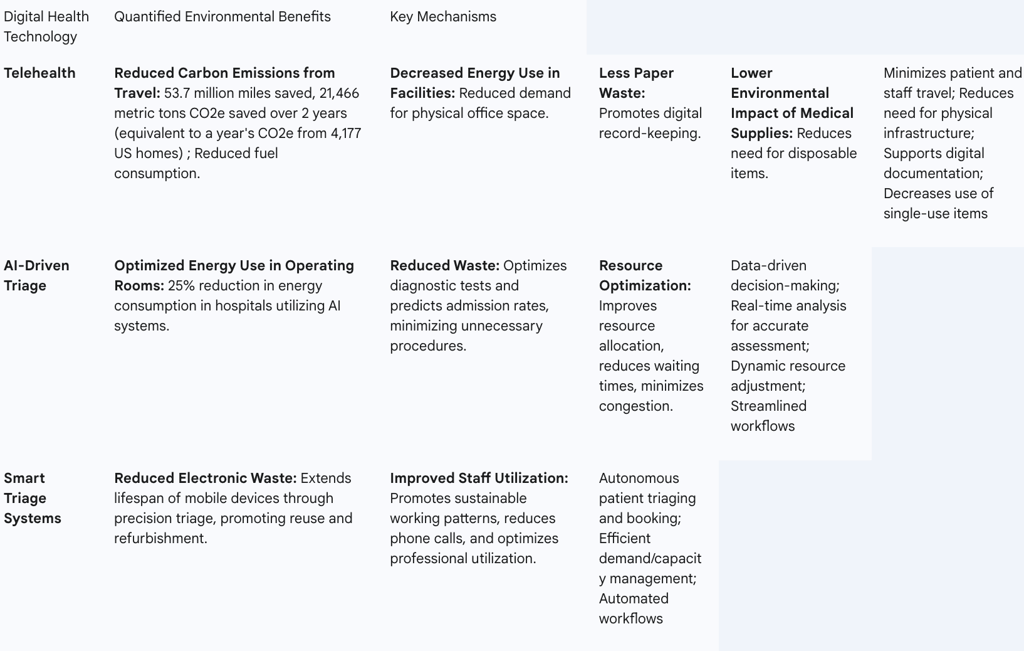
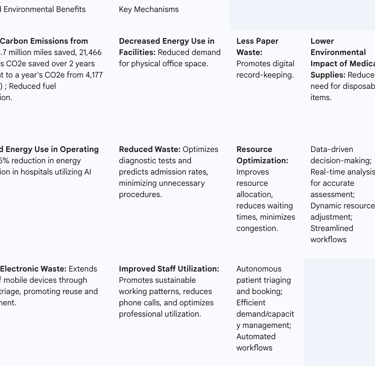
Table 3: Environmental Benefits of Digital Health Technologies in Healthcare
3.3 Broader Sustainable Healthcare Practices Influencing Triage
The environmental footprint of triage is deeply intertwined with broader healthcare sustainability practices. Therefore, improvements in triage must be part of a larger, integrated sustainability strategy.
Green Procurement and Supply Chain Management: Healthcare supply chains account for a significant portion (60-80%) of the sector's carbon footprint globally. Reducing emissions in the supply chain is essential for achieving low-carbon healthcare. This involves prioritizing suppliers who provide verified environmental disclosures and have invested in sustainability initiatives. Purchasing from smaller, local suppliers can also shorten the supply chain and reduce transportation emissions. The NHS in England, for example, has committed to reaching net zero by 2045, including emissions embedded in its supply chain.
Energy Efficiency and Renewable Energy Adoption: Hospitals operate continuously, demanding massive amounts of energy. Improving energy efficiency and shifting to clean, renewable energy sources like wind, solar, and geothermal are highly effective steps to reduce environmental impact and protect community health. These measures can also enhance patient outcomes and minimize costs. Strategic Energy Master Plans (SEMPs) are a key strategy for hospitals to identify reduction goals and implement renewable energy solutions.
Advanced Waste Management and Recycling: Healthcare facilities generate millions of tons of waste annually. Effective strategies involve reducing, treating, and safely disposing of healthcare waste. Non-burn technologies are available for waste disinfection, neutralization, or containment. Implementing practices like composting food scraps can significantly reduce GHG emissions and save on landfill fees, as demonstrated by Providence hospital which reduced GHG emissions by 18,890 kg CO2e in 2022. Utilizing reusable items, such as cloth gowns and dishware, directly reduces waste volumes. Recycling packaging can also lower waste and incineration rates. Despite the potential for recycling (85% of plastics waste could be recycled), a significant portion (91%) still ends up in landfills or natural environments.
Reducing Low-Value Care and Promoting Preventative Health: Low-value care, defined as interventions offering minimal or no benefit, generates carbon emissions, waste, and pollution without improving patient or population health. It is estimated that up to 30% of clinical care is low- or no-value. The most effective way to reduce healthcare's environmental impacts is to limit the need for healthcare activities in the first place. This necessitates a shift from a purely curative model to one that emphasizes preventative care. Empowering patients in self-care can reduce disease incidence and pre-empt complications, thereby lessening the demand for resource-intensive interventions. Initiatives like the "Choosing Wisely" campaign aim to curtail low-value investigations and wasteful interventions.
Sustainable Facility Design: While new construction in healthcare has received relatively little examination regarding sustainability , hospital design, operations, and employee behavior all shape carbon emissions. Incorporating green infrastructure, such as trees, parks, and green roofs, can improve public health by cleaning the air. Similarly, using natural elements like indoor plants within clinics can clean indoor air and enhance patient comfort. A strategic approach to sustainability in facilities can integrate these factors while considering limited funding, accreditation processes, and low-risk tolerance inherent in healthcare.
The systemic nature of sustainable triage becomes apparent when considering its interconnectedness with broader healthcare sustainability practices. Interventions aimed at reducing healthcare's overall environmental footprint, such as green procurement, energy efficiency, and advanced waste management, often yield positive health, economic, and organizational co-benefits. This suggests that "greening the health care sector" requires a comprehensive, sector-wide mobilization, and that triage improvements are not isolated efforts but integral components of a larger, integrated sustainability strategy. This means that achieving environmental sustainability in triage cannot be isolated from the overall greening of the healthcare system. Improvements in procurement, energy, waste management, and preventative care create a more sustainable context that amplifies the environmental benefits of optimized triage. This necessitates a multi-pronged, systemic approach where triage improvements are part of a larger, integrated sustainability framework.
Furthermore, framing sustainability initiatives in healthcare, including those related to triage, through their economic co-benefits can be a powerful driver for adoption. The literature explicitly states that "saving energy leads to savings," and quantifies this by noting that one dollar saved from energy conservation is approximately equivalent to $20 in new revenue for hospitals, based on a typical 5 percent profit margin. Practical examples, such as composting food scraps, have demonstrated significant financial savings (e.g., $22,000 in landfill fees) alongside CO2e reductions. Similarly, sustainable sourcing and procurement practices can reduce waste and generate cost savings. This means that environmental sustainability is not merely an environmental imperative but also a financial opportunity. This shifts the narrative from the "cost of going green" to the "return on investment from sustainability," which can accelerate the adoption of greener practices within triage and across the broader healthcare landscape, especially given prevalent budget constraints.
4. Measuring and Assessing Environmental Impact in Healthcare
Accurately measuring the environmental footprint of healthcare activities, including triage, is crucial for identifying hotspots, tracking progress, and informing strategic decisions.
4.1 Methodologies for Carbon Footprint Analysis
Several methodologies exist for assessing environmental impact in healthcare, each with its strengths and applications:
Life Cycle Assessment (LCA): LCA provides a comprehensive method to evaluate the environmental impact of products, processes, and procedures across their entire lifecycle, from "cradle to grave". This includes the environmental burdens of raw material extraction, manufacturing, transportation, use, and end-of-life disposal. International Organization for Standardization (ISO) standards (e.g., ISO 14040, 14044, 14067) provide a standardized framework for conducting LCAs, which can be applied to various industries, products, or processes to analyze environmental impacts and identify interventions for emission reduction. LCA is used for comparing single-use versus reusable products, evaluating processes, and assessing material efficiency. While frameworks for healthcare LCA often adapt models from other fields, they are then modified for healthcare-specific contexts.
Carbon Footprint Analysis of Clinical Pathways: This methodology specifically estimates the direct and indirect greenhouse gas (GHG) emissions attributable to an individual clinical pathway or service. Unlike an organizational carbon footprint analysis, it provides a focused assessment of the environmental impact of specific activities and resources required for care delivery within that pathway. This analysis can be extended to include social and financial impacts, forming a "triple bottom line" evaluation. Environmentally-extended input-output (EEIO) analysis can also be employed to calculate systemic carbon footprints for healthcare activities, facilitating the comparison of different patient care pathways.
Other Methods: The Healthcare Environmental Impact Factor (HEIF) scheme can be used as a tool for selecting measurable indicators to be applied in quality management. Other approaches to quantify environmental impact include calculations using models such as mass-balance approaches, GHG activity multiplication, and general environmental impact assessments. Quality management (QM) methods also support the integration of sustainability into decision-making and facilitate the implementation of environmental management systems.
4.2 Challenges and Opportunities in Implementation
Despite the availability of methodologies, significant challenges persist in the practical implementation of environmental impact assessments within healthcare. Life Cycle Assessments, for instance, are not yet common in healthcare practice and require substantial expertise, resources, and time. A major barrier is that many healthcare decisions must consider multiple variables not directly related to a product's environmental impact, such as patient safety, clinical risk, and costs. Furthermore, methodological inconsistencies across studies limit their comparability , and there is limited research on sustainability practices and proactive policies in resource-constrained settings, coupled with a lack of standardized reporting frameworks.
However, these challenges also present opportunities. Expanding decision-making frameworks to explicitly include environmental impact is increasingly recognized as necessary. LCA, in particular, quantifies impacts and generates data that can inform and support these decisions. Lessons learned from other industries, such as the building industry, highlight the importance of third-party certification for increased confidence in assessments and the value of comparing impacts across products to support decision-making. Integrating emissions assessment into existing decision-making processes is a promising avenue , and reporting environmental impact outcomes alongside clinical and economic endpoints may incentivize reduced unnecessary resource use.
A significant gap exists between the need for robust environmental data and its practical integration into healthcare decision-making and daily operations. The literature consistently points out that LCAs are "not common in healthcare practice" and face barriers such as "substantial expertise, resources, and time". Additionally, many healthcare decisions are driven by factors not directly related to environmental impact, such as patient safety and costs. The presence of "methodological inconsistencies" and a "need for more standardisation" further exacerbates this issue. This "data-action gap" is rooted in a historical prioritization of clinical and financial outcomes over environmental ones, coupled with resource constraints and a lack of standardized methodologies. Overcoming this requires not just the development of better tools, but also fundamental shifts in policy, comprehensive training programs, and a cultural transformation to embed environmental considerations into core decision-making frameworks.
The adoption of a "triple bottom line" approach can serve as a catalyst for change. The concept of extending carbon footprint evaluation to include "social impacts... and financial impacts" alongside environmental ones provides a more holistic perspective. This aligns with broader movements towards "value-based care, green hospital initiatives, and equity-driven financial models" that support both long-term financial viability and global sustainability goals. This means that measuring environmental impact in isolation may not be sufficient to drive widespread change in healthcare. By explicitly linking environmental performance with economic benefits (e.g., cost savings from waste reduction and energy efficiency) and social outcomes (e.g., improved patient and staff experience, enhanced equity), healthcare organizations can construct a more compelling business case for sustainability initiatives. This integrated reporting framework has the potential to align diverse stakeholder interests and accelerate the adoption of greener practices within triage and across the entire healthcare system.
Conclusion and Recommendations
5.1 Key Findings and Synthesis
The healthcare sector, despite its healing mission, paradoxically contributes significantly to global environmental degradation, with its carbon footprint ranking among the world's largest industrial emitters. This impact is driven predominantly by its vast supply chains, substantial energy consumption, and complex waste management challenges. Within this context, healthcare triage, a critical process for patient prioritization and resource allocation, plays a pivotal role in amplifying or mitigating this environmental burden.
Inaccurate triage decisions, particularly overtriage, lead to a cascade of unnecessary resource consumption. Overtriage directly fuels "low-value care," resulting in superfluous diagnostic imaging and laboratory tests, each carrying a quantifiable carbon footprint. This initial misallocation triggers a compounding effect, where unnecessary interventions lead to further tests and treatments, escalating the environmental cost. Conversely, undertriage, by delaying appropriate care, can lead to patient deterioration, necessitating more intensive, prolonged, and resource-heavy interventions later in the care pathway, thereby indirectly increasing the environmental burden. Emergency departments, with their 24/7 operations, energy-intensive modalities, and reliance on disposables, represent significant environmental hotspots where these dynamics are particularly pronounced. The interconnectedness of waste, energy, and clinical practice underscores the need for holistic solutions.
However, significant opportunities exist for mitigation. Digital health technologies, especially telehealth, offer a multi-faceted environmental solution by reducing patient travel, facility energy use, and waste from disposables. AI-driven triage systems hold immense potential for optimizing resource allocation, streamlining patient flow, and reducing unnecessary procedures, thereby minimizing waste. Yet, the growing environmental footprint of the underlying ICT infrastructure for AI necessitates a "Green AI" approach. Beyond technology, broader sustainable healthcare practices—including green procurement, energy efficiency, advanced waste management, and a shift towards preventative care—are crucial. These systemic changes not only reduce environmental impact but often yield significant economic co-benefits, providing a compelling business case for adoption. Despite the clear imperative, a data-action gap persists, driven by a lack of standardized measurement methodologies and a historical focus on clinical and financial outcomes over environmental ones. Bridging this gap requires robust assessment tools and a "triple bottom line" approach that integrates environmental, social, and economic considerations.
5.2 Actionable Recommendations for Stakeholders
To navigate the complex interplay between healthcare triage and its environmental footprint, a concerted effort across all stakeholder levels is essential.
For Policymakers and Healthcare Administrators:
Integrate Sustainability into Core Strategy: Mandate and integrate environmental sustainability into all strategic planning, facility design, and accreditation processes. This ensures sustainability is not an afterthought but a foundational principle.
Fund Carbon Footprint Assessments: Allocate dedicated funding for comprehensive carbon footprint assessments, including Life Cycle Assessments (LCA) for products and processes, and clinical pathway analyses. Standardized methodologies must be developed and adopted to ensure comparability and effectiveness.
Enforce Green Procurement: Develop and strictly enforce green procurement policies that prioritize suppliers with verified environmental disclosures. Actively encourage suppliers to decarbonize their operations and explore opportunities for local sourcing to shorten supply chains and reduce transportation emissions.
Invest in Green Infrastructure: Prioritize investment in energy-efficient infrastructure upgrades and the adoption of clean, renewable energy sources for healthcare facilities. Implement Strategic Energy Master Plans (SEMPs) to guide this transition.
Promote Responsible Digital Health Adoption: Incentivize the widespread adoption of telehealth and AI-driven triage systems, while simultaneously ensuring their responsible development and deployment. This includes addressing the ICT footprint by supporting sustainable data centers and energy-efficient AI algorithms ("Green AI").
Strengthen Waste Management: Implement robust waste management policies that prioritize reduction, reuse, and recycling over incineration. Invest in non-burn technologies for medical waste treatment and promote the use of reusable medical items where clinically appropriate.
Support Preventative Care: Shift healthcare models towards prevention and health promotion to reduce the overall demand for acute services and associated resource consumption. This includes empowering patient self-care and addressing social determinants of health.
For Clinicians and Frontline Staff:
Prioritize Triage Accuracy: Engage in continuous education and simulation training to enhance triage accuracy. Actively utilize electronic decision-support tools to minimize over- and undertriage, thereby optimizing resource allocation and patient flow.
Reduce Low-Value Care: Actively question and reduce unnecessary tests, procedures, and prescriptions by adhering to "Choosing Wisely" principles. Recognize that every unnecessary intervention carries an environmental cost.
Champion Waste Reduction: Be proactive in waste segregation at the source, promote recycling initiatives, and advocate for the use of reusable medical supplies where infection control and patient safety allow.
Embrace Telehealth: Advocate for and adopt telehealth for suitable patient interactions, recognizing its significant potential to reduce patient travel emissions and facility resource use.
Foster Resource Stewardship: Cultivate a mindset of resource stewardship, understanding that every clinical decision has an environmental consequence. Promote sustainable practices within daily workflows.
5.3 Future Research Directions
To further advance the understanding and mitigation of healthcare's environmental footprint, particularly concerning triage, several key research areas warrant focused attention:
Longitudinal Environmental Impact Studies: Conduct long-term longitudinal studies to comprehensively evaluate the environmental impacts of specific triage interventions and their downstream effects on patient pathways and resource consumption. This will provide more robust evidence for effective strategies.
Standardization of Assessment Methodologies: Develop and validate standardized carbon footprint assessment methodologies specifically tailored for diverse healthcare settings and medical specialties. This will improve the comparability and reliability of environmental impact data across the sector.
Life Cycle Assessments of Patient Pathways: Undertake detailed Life Cycle Assessments (LCAs) of entire emergency department patient journeys and other complex clinical pathways. This will identify specific "hotspots" of environmental impact from patient arrival to discharge and beyond, informing targeted interventions.
Net Environmental Impact of Digital Health: Conduct comprehensive evaluations of the net environmental impact of AI and other digital health technologies. This research must consider their full lifecycle, including the energy consumption and resource demands of their underlying Information and Communication Technology (ICT) infrastructure, to ensure that the benefits outweigh the environmental costs.
Behavioral Change Interventions: Research the effectiveness of behavioral change interventions aimed at promoting sustainable practices among healthcare staff and patients. Understanding how to foster a culture of environmental responsibility is crucial for widespread adoption.
Integrated Economic Modeling: Develop economic models that fully integrate environmental costs and benefits into healthcare decision-making frameworks. This will provide a robust business case for sustainability initiatives and help overcome financial barriers to adoption.
FAQ Section
What is the environmental impact of traditional healthcare triage?
Traditional healthcare triage has a significant environmental impact due to high energy consumption, transportation emissions, and waste generation.
How does digital healthcare triage reduce environmental impact?
Digital healthcare triage reduces environmental impact by lowering transportation emissions, facility energy use, and waste generation.
What are the environmental considerations of digital healthcare triage?
Digital healthcare triage introduces new environmental considerations, such as data centre energy consumption and e-waste from digital devices.
How does energy consumption differ between traditional and digital triage?
Traditional triage consumes about 50 kWh per patient; digital triage consumes around 10 kWh per patient, plus an additional 5 kWh for data centre energy use.
What is the impact of transportation emissions in traditional vs. digital triage?
Traditional triage results in about 20 kg CO2eq of transportation emissions per patient, compared to 2 kg CO2eq per patient for digital triage.
How does waste generation compare between traditional and digital triage?
Traditional triage generates about 1.5 kg of waste per patient, while digital triage generates around 0.5 kg per patient.
What is the impact of e-waste on digital healthcare triage?
Digital healthcare triage results in about 2 kg of e-waste per 1000 patients.
How can the environmental footprint of healthcare triage be further reduced?
Optimising digital tools, improving energy efficiency in healthcare facilities, and promoting sustainable practices can reduce healthcare triage's environmental footprint.
What role do healthcare providers play in reducing the environmental impact of triage?
Healthcare providers play a crucial role in reducing the environmental impact of triage by adopting sustainable practices, utilising energy-efficient technologies, and promoting digital solutions.
How can patients contribute to reducing the environmental footprint of healthcare triage?
Patients can contribute to reducing the environmental footprint of healthcare triage by opting for digital triage tools, reducing unnecessary visits, and following sustainable healthcare practices.
