The Dutch Triage Standard (NTS): Its Design, Performance, and Evolution
The Nederlandse Triage Standaard (NTS) is a nationally mandated, computer-aided triage system established in the Netherlands. Its development, initiated by the Dutch Ministry of Health, Welfare and Sport in 2007, was a direct response to the need for a more standardized, safe, and efficient approach to acute care triage.


The Nederlandse Triage Standaard (NTS) is a nationally mandated, computer-aided triage system established in the Netherlands. Its development, initiated by the Dutch Ministry of Health, Welfare and Sport in 2007, was a direct response to the need for a more standardized, safe, and efficient approach to acute care triage. The NTS serves as a crucial component of the Dutch healthcare infrastructure, providing a unified methodology for prioritizing patients across out-of-hours general practitioner (GP) cooperatives, hospital emergency departments (EDs), and ambulance dispatch centers.
The NTS is built upon a foundation of structured protocols, guiding medical staff through a five-step process that culminates in one of six urgency levels. Its key strengths lie in its ability to provide a uniform language and consistent work method across the acute care chain, which has been scientifically validated through studies demonstrating good inter-rater reliability and high sensitivity for adult patients. The system is not static; it is a living standard maintained and continuously updated by the dedicated Stichting Nederlandse Triage Standaard (NTS Foundation).
Despite its robust framework, the NTS faces acknowledged challenges. Research indicates it has limitations when applied to specific patient populations, particularly pediatrics and the elderly, leading to notable rates of undertriage and overtriage. Empirical comparisons with other triage systems, such as the Emergency Severity Index (ESI), suggest that the NTS's lowest urgency levels may not adequately discriminate against patients who ultimately require hospitalization or have adverse outcomes.
In response to these identified limitations and the projected demographic shifts—including the doubling of the Dutch population aged 75 and older by 2050—the NTS Foundation is actively pursuing strategic evolution. The development of specialized standards, such as NTS GZ (for disability care) and NTS V&V (for nursing and care), represents a proactive effort to tailor triage protocols for vulnerable patient groups, promising to improve both the safety and efficiency of care for these complex populations. This forward-thinking adaptation reinforces the NTS's role as a cornerstone of the Dutch emergency care system.
Foundational Principles of the NTS
The acronym NTS can refer to a variety of entities. It is essential to first clarify that within the context of this report, NTS refers exclusively to the Nederlandse Triage Standaard (Dutch Triage Standard). This must be distinguished from the Nederlandse Omroep Stichting (NOS), a Dutch public broadcaster , the NTS-Group, a mechatronics company , or the National Technology Strategy, a governmental policy framework. In the medical domain, NTS also refers to Nanopore targeted sequencing, a diagnostic technique. The focus of this analysis is the healthcare triage system.
The NTS was formally developed in 2007 under the auspices of the Dutch Ministry of Health, Welfare and Sport. Its central mission was to enhance patient safety and optimize the efficiency of triage within the acute care sector. The system's design is fundamentally that of a standardized, computer-supported decision-making tool. Its purpose is not to render a definitive medical diagnosis, but rather to rapidly determine the urgency of a patient's condition and the appropriate subsequent action.
A critical aspect of the NTS's historical context is its derivation from the Manchester Triage System (MTS). The NTS is officially a "modified version of the Manchester Triage System," supplemented with existing Dutch telephone triage protocols used in primary care. This is more than a simple borrowing of ideas; it represents a deliberate adaptation of an internationally recognized framework to the unique structure of the Dutch healthcare system, which features a robust out-of-hours primary care network. One study, in fact, noted that the NTS and MTS were "not comparable" after the implementation of the NTS in an emergency department. This observation underscores the fact that the modifications were not minor, but rather significant enough to create a distinct and separate system. The NTS's design, therefore, reflects a strategic effort to tailor a global model to local clinical practices and organizational structures.
A comparison of the urgency levels in both systems highlights these adaptations. The NTS expands upon the four-level MTS scale by adding two additional categories, U0 and U5, which are vital for managing the full spectrum of patient presentations in the Dutch system.
Table 1: NTS vs. MTS Urgency Level Comparison
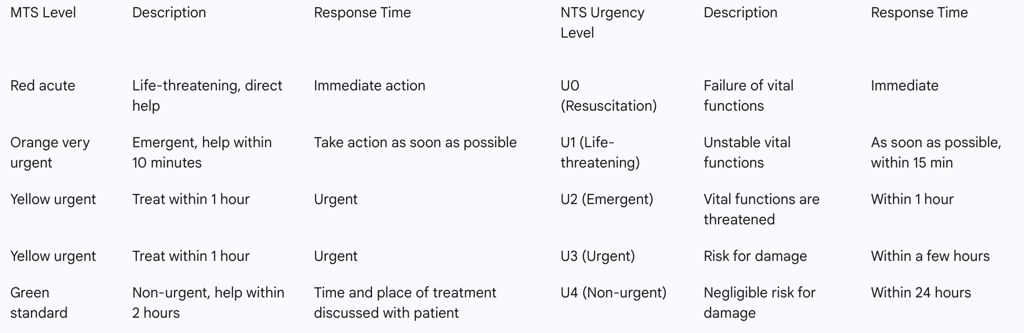
This comparison reveals that the NTS has a more granular and distinct scale. The addition of U0, "Resuscitation," and U5, "Advice," allows the system to clearly define actions for the most critical patients at one end and to provide a formal protocol for low-acuity cases that may only require telephone advice at the other. This structure is particularly well-suited for a national system that encompasses both high-acuity hospital EDs and low-acuity primary care centers.
Operational Mechanics and Triage Methodology
The NTS employs a structured, five-step process that a triagist follows to determine a patient's urgency level. This protocol-driven approach ensures consistency and is applicable for both telephone and physical triage.
The first step is a critical safety check known as the "ABCDE-veilig" (ABCDE-safe) assessment. The triagist evaluates the patient's vital functions—Airway, Breathing, Circulation, Disability, and Environment—to immediately identify and address any life-threatening conditions. If the patient's condition is assessed as "unsafe," such as being hemodynamically unstable, an ambulance is immediately dispatched. This initial step is designed to prevent delayed care for the most critical cases.
Following the ABCDE-veilig check, the triagist proceeds to the second step: selecting an "entrance complaint" from a list of 55 standardized categories. This selection guides the remainder of the triage process.
Table 2: Sample NTS Entrance Complaints
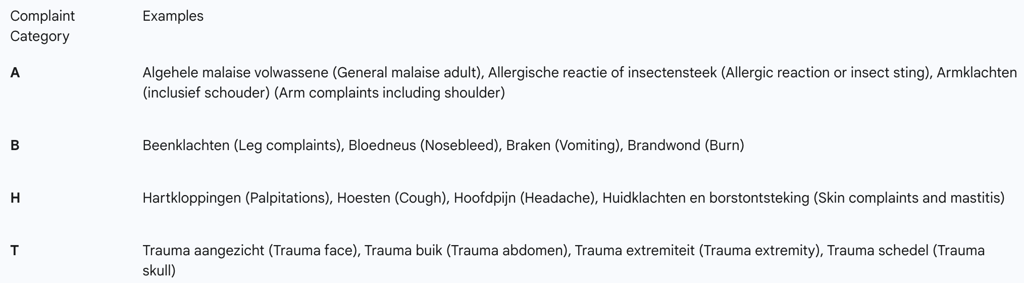
Once an entrance complaint is chosen, the system, which is computer-supported, presents a series of specific triage criteria, or discriminators. Based on the triagist's responses to these questions, the NTS algorithm proposes an urgency level from U0 to U5. The triagist then determines the appropriate follow-up action based on this urgency level and the triagist's assessment of the case. Finally, the triagist provides patient-specific advice tailored to the situation.
The six-level urgency scale is the central pillar of the NTS, each level corresponding to a specific response time and description of the patient's condition:
U0 (Resuscitation): This level is for cases involving the failure of vital functions, such as no breathing, and necessitates immediate action.
U1 (Life-threatening): For patients with unstable vital functions, demanding action as soon as possible. Examples include a high suspicion of myocardial infarction or stroke.
U2 (Emergent): This level is for cases where vital functions are threatened, requiring care within one hour. A low suspicion of myocardial infarction or severe dyspnea are examples.
U3 (Urgent): Indicates a real risk for damage and calls for care within a few hours. A kidney stone with significant pain is a classic example.
U4 (Non-urgent): For conditions with negligible risk for damage, with a response time of up to 24 hours. A urinary tract infection or severe itching are examples.
U5 (Advice): This level applies to cases with no risk of damage, where the appropriate course of action is telephone advice or an appointment on the next working day, such as a fever without other symptoms.
Systemic Integration and Implementation
The NTS is not confined to a single clinical setting; it is designed as a unified standard for the entire acute care chain in the Netherlands. It is actively used by out-of-hours GP cooperatives, hospital emergency departments, and ambulance dispatching centers, ensuring a consistent approach to triage regardless of where a patient first seeks care. This "unity of language and work method" is a core policy objective that aims to create a more integrated and less fragmented healthcare system.
The triagist is the linchpin of this system. Triagists are typically medical staff with backgrounds as GP nurses or hospital nurses, and they are trained to use the NTS for both telephone and physical triage. A crucial aspect of their role is that it is not purely mechanical. While the NTS provides a recommended urgency level, the triagist has the professional authority to overrule the system's suggestion based on their clinical judgment. This human element is a critical layer of safety and efficiency, allowing for a nuanced assessment of factors not captured by the computer algorithm.
This capability for human override is not merely a theoretical option; it is an essential part of the system's function. Research shows that external factors, such as the COVID-19 pandemic, can influence triage decisions, leading triagists to make more frequent adjustments to the assigned urgency. Similarly, studies on shortness of breath complaints have found that a triagist's subjective, "uncanny feeling" about a patient's condition can be predictive of a potential life-threatening event, even when explicit symptoms do not indicate a high urgency. Furthermore, an analysis of surrogate calls (when someone calls on behalf of a patient) found that these calls more often received a high urgency level, indicating that the triagist's interpretation of the caller's distress or specific circumstances can significantly influence the outcome. These findings highlight that the NTS is a hybrid system, combining the rigor of a protocol-driven tool with the indispensable interpretive skills of the trained triagist. The effectiveness of the system, therefore, is directly linked to the triagist's competence and ability to synthesize protocol and intuition.
Performance Analysis: Empirical Evidence and Critical Review
The NTS has been the subject of numerous studies evaluating its effectiveness, particularly concerning its reliability and validity. Reliability, which measures the consistency of the system's application across different triagists, is generally considered good. For adult cases, the intraclass correlation coefficient (ICC) is 0.88, indicating high agreement, while for pediatric cases, it is 0.73, suggesting moderate reliability. The NTS also demonstrates good construct validity, meaning its urgency levels correlate well with clinical outcomes such as hospitalization and resource use. A study found that the urgency level assigned by the NTS was significantly associated with increased resource use, hospitalization rates, and length of stay.
When evaluating the NTS's performance, it is crucial to examine its sensitivity and specificity—the two key metrics for a diagnostic-like tool.
Adult Cases: The NTS has a high sensitivity of 94.5% for identifying highly urgent cases, meaning it is very effective at correctly flagging patients who need immediate attention. Its specificity is 83.3%, which indicates a low rate of over-triaging low-urgency patients.
Pediatric Cases: The system's performance is slightly lower but still robust, with a sensitivity of 85.2% and a specificity of 89.7% for high-urgency cases.
Despite these positive metrics, a consistent limitation of the NTS is the prevalence of under- and overtriage. This refers to the misclassification of patients, either by underestimating the severity of their condition or by overestimating it. The system shows an underestimation rate of 13.7% for adult cases and 17.4% for pediatric cases. Overtriage rates are similar, at 18.0% for adults and 20.2% for children.
The potential for undertriage poses a significant safety concern. This is best illustrated by a study on patients calling with shortness of breath (SOB), where 46% of patients with a life-threatening event (LTE) were undertriaged, meaning they did not receive a high urgency classification. This finding suggests that for certain critical complaints, the NTS protocols may not fully capture the clinical risk, leading to potentially delayed care. This limitation is further underscored by a comparative study showing that the NTS's lowest urgency level (U5) was associated with a mortality rate of 12.4%, which was significantly higher than the 0.8% mortality rate in the lowest urgency level of the ESI system. The fact that the NTS's low-urgency categories still carry a high risk of adverse outcomes indicates a fundamental weakness in its ability to effectively distinguish between genuinely low-risk and high-risk patients.
Table 3: NTS Performance Metrics (Reliability and Validity)
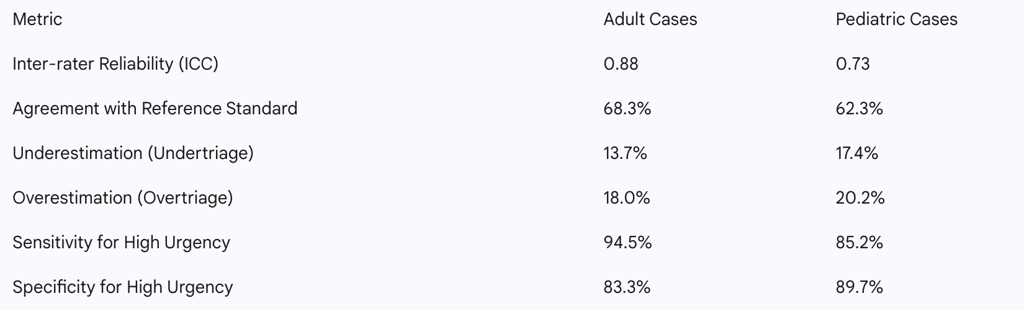
The data above shows that while the NTS is a reliable and generally valid tool, its performance is not flawless. The rates of under- and overtriage, along with the notable mortality rate in low-urgency categories, point to a persistent safety gap. This problem is particularly acute for vulnerable groups, as there is currently no specific data on the NTS's applicability for infants under one year of age. The current system, designed for a general population, may not adequately account for the distinct needs and clinical presentations of these complex patient groups.
The NTS Foundation: Governance, Training, and Dissemination
The NTS is not a static document but a dynamic system, continuously overseen and improved by a dedicated governing body: the Stichting Nederlandse Triage Standaard (NTS Foundation). The Foundation acts as the national standard-bearer for acute care triage and plays a vital role in commissioning scientific studies to validate and refine the standard. This is demonstrated by the ongoing cycle of updates, such as the
NTS Update V 11.10, which includes user consultations to incorporate feedback from the field. The Foundation’s structure provides a formal mechanism for self-correction, ensuring the standard remains current and responsive to new evidence and changing needs.
Training and education are integral to the effective use of the NTS. All GPC and ED nurses receive standardized training on how to apply the system. The NTS Foundation collaborates with a variety of organizations to create educational resources. A key tool in this ecosystem is the
NHG-TriageWijzer, which serves as both a reference guide and a training tool, with its content updated in accordance with the latest NTS changes. This ensures that medical professionals, from triage assistants to general practitioners, have access to a consistent, up-to-date source of information.
In a move to modernize and expand training, the NTS Foundation also supports the Triage Game. This free, online game provides a playful yet realistic simulation for triagists and GPs to practice their skills in a low-stakes environment. The development and promotion of such a gamified learning tool illustrate a commitment to innovative educational methods and underscore the recognition that a well-trained human triagist is a critical component of the NTS's success. This institutional support for ongoing professional development is a distinguishing feature of the NTS ecosystem, showcasing its evolution beyond a simple set of protocols into a comprehensive, self-sustaining system.
Future Directions: The Evolution of NTS
The NTS is undergoing a significant strategic evolution, driven by the need to address its limitations and adapt to future demographic pressures. The central challenge is a growing and increasingly complex patient population, particularly the elderly and individuals with disabilities. Projections indicate that the number of Dutch people aged 75 and older is set to double by 2050, while the healthcare workforce is projected to shrink. The current, one-size-fits-all NTS, designed for the general population, is proving insufficient for these vulnerable groups, leading to "inefficiencies and unnecessary escalations, such as over- or undertreatment".
In response to this urgent need, the NTS Foundation is developing two new, specialized triage standards:
NTS V&V (Verpleging en Verzorging): A standard for nursing and care, designed for the elderly.
NTS GZ (Gehandicaptenzorg): A standard for disability care.
The development of these standards is a direct response to the documented clinical reality that "communication with these patient groups is often different, treatment plans can vary, and some symptoms may present differently". The project involves a multi-disciplinary expert team, including geriatric specialists, doctors for the intellectually disabled, GPs, emergency room doctors, and nurses. This collaborative approach ensures the new standards will be clinically relevant and tailored to the unique needs of these patients.
This strategic shift from a monolithic standard to a suite of tailored standards represents a profound acknowledgement of the NTS's limitations. It is a proactive move that aims to improve care outcomes for the most complex patients while also reducing unnecessary referrals and freeing up resources in the wider healthcare system. The NTS Foundation's decision to embark on this project demonstrates a forward-thinking approach to managing demographic change and optimizing acute care for a more complex future. The new standards are expected to provide faster clarity and more appropriate care at the right time and place, benefiting patients, professionals, and the entire healthcare chain.
Conclusion: A Dual Perspective on the NTS
The Dutch Triage Standard (NTS) stands as a notable achievement in the national standardization of acute care. Its strengths are rooted in a clear, protocol-driven methodology that provides a unified language and process across the diverse settings of the Dutch emergency care system. The system has been empirically validated, demonstrating good reliability and high sensitivity for the general adult population, which attests to its effectiveness as a tool for a rapid, initial assessment. The NTS is also supported by a robust institutional framework, with the NTS Foundation and its network of training partners ensuring continuous improvement and broad adoption.
However, the analysis also reveals persistent challenges. The NTS's generalist design leads to rates of under- and overtriage that, while sometimes acceptable in a broad context, can be critically unsafe in specific high-risk scenarios, such as for patients with shortness of breath. The system's documented failure to fully discriminate between low-urgency and high-risk patients, particularly when compared to other systems like ESI, is a significant concern that highlights a persistent safety gap at the lower end of the triage scale. Furthermore, the lack of a tailored approach for vulnerable populations like infants, the elderly, and the disabled points to a critical area for improvement.
The future trajectory of the NTS lies in its ability to address these documented limitations. The ongoing development of the specialized NTS GZ and NTS V&V standards is a powerful testament to the system's capacity for evolution and a pragmatic response to both clinical evidence and demographic shifts. The success of the NTS going forward will depend on two key factors: first, its continued refinement through targeted, evidence-based updates; and second, a sustained investment in the training and professional judgment of the triagists who serve as the critical human layer, bridging the gap between a standardized protocol and the nuanced realities of patient care.
