South African Triage Scale (SATS): An Overview
Discover the South African Triage Scale (SATS) - a validated four-level emergency triage system. Learn about implementation, validation studies, benefits, and challenges in emergency departments worldwide.


The South African Triage Scale (SATS) stands as a nationally validated and indispensable clinical tool, introduced in 2006, specifically engineered to augment the efficiency of emergency centers by systematically prioritizing patients based on their physiological state and presenting symptoms. Distinguished as one of the few triage systems purpose-designed for low- and middle-income countries (LMICs), SATS directly addresses prevalent challenges such as staff shortages and limited resources within emergency departments, while simultaneously guiding clinical decision-making and offering prognostic indicators for mortality.
Its core methodology integrates a five-step patient classification process, a quantitative Triage Early Warning Score (TEWS), and a critical discriminator list that allows for the immediate identification of high-risk conditions. Patients are categorized into five color-coded priority levels—Red, Orange, Yellow, Green, and Blue—each associated with a specific target time for clinical intervention, thereby standardizing urgency and facilitating resource allocation.
While SATS has demonstrated good predictive validity in various trauma and mixed emergency department settings, particularly in identifying patients at risk of hospitalization and mortality, its real-world implementation faces notable challenges. Studies reveal significant rates of under-triage, especially in pre-hospital environments and for specific complex injuries like penetrating neck injuries, alongside inconsistencies in the application of TEWS and discriminators. These discrepancies underscore a critical gap between the tool's intended design and its practical execution.
The ongoing importance of SATS in resource-constrained settings is undeniable. However, realizing its full potential necessitates continuous, targeted training, potential adaptations of the tool for specific contexts, and a commitment to ongoing quality improvement initiatives to enhance accuracy, minimize under-triage, and ultimately optimize patient outcomes and emergency department flow.
1. Introduction
Defining the South African Triage Scale (SATS)
The South African Triage Scale (SATS) is a nationally validated clinical tool, formally introduced in 2006, with the explicit aim of enhancing the operational efficiency of emergency centers through the systematic prioritization of severely ill patients. This robust system employs a physiology and symptom-based approach, categorizing individuals into distinct triage classifications denoted by colors: green, yellow, orange, red, and blue. This color-coded stratification is fundamental to directing immediate and appropriate care.
A distinguishing characteristic of SATS is its deliberate design for use in low- and middle-income countries (LMICs). This foundational design choice is strategic, as it directly confronts the unique challenges prevalent in these settings, such as chronic staff shortages and limited material resources within emergency departments. By providing a structured framework, SATS guides clinical decision-making, streamlines patient flow, and offers valuable insights into predicting patient mortality, thereby serving as a cornerstone for emergency care in environments where demand often outstrips supply. The inherent strengths and weaknesses of SATS are thus deeply intertwined with its intended LMIC context. Its performance, whether successful or challenging in different settings (e.g., pre-hospital versus in-hospital, well-resourced versus under-resourced facilities), often depends on how effectively these contextual factors are managed during its application. Therefore, assessing SATS solely by metrics or standards derived from high-income, resource-rich settings may not fully capture its primary utility, which lies in its adaptability to constrained environments.
Crucial Disambiguation
It is imperative to clarify that this report focuses exclusively on the South African Triage Scale (SATS), a medical emergency assessment and prioritization tool. The acronym "SATS" is also associated with other distinct concepts, such as the Scholastic Assessment Test (SAT), a standardized college admissions exam ; the Systematic Approach to Training (SAT) in organizational development ; and Site Acceptance Test (SAT) in equipment qualification processes. These unrelated uses of the acronym appear in various research materials but are entirely outside the scope of this medical overview and will not be discussed further. This precise distinction is vital for maintaining the accuracy and focus of an expert-level medical report.
Purpose and Scope of the Report
This report aims to deliver a comprehensive, expert-level overview of the South African Triage Scale. It delves into the tool's historical development, elucidates its methodological components, describes its application settings and target populations, and critically evaluates its reported effectiveness, advantages, and limitations. The objective is to provide a holistic and evidence-based understanding of SATS for healthcare professionals, policymakers, and researchers engaged in emergency medicine and public health, thereby informing practice, research, and strategic planning.
2. Historical Development and Evolution of SATS
Genesis and National Introduction
The South African Triage Scale (SATS) was officially introduced for national implementation across South Africa in 2006. Its inception was the result of a concerted and collaborative endeavor by the South African Triage Group (SATG). This multidisciplinary consortium brought together a diverse group of medical professionals, including doctors, nurses, and paramedics, reflecting a commitment to developing a practical and widely applicable tool. The primary objective driving this collaborative effort was to establish a standardized triage scale that could be uniformly applied across the entirety of South Africa’s varied healthcare landscape, ensuring consistency in patient assessment and prioritization regardless of the specific facility or region.
Key Milestones and Validation
SATS is widely recognized as a validated tool, a designation earned through a rigorous and extensive evidence-based development process. Its validation has spanned diverse healthcare environments, encompassing public sector facilities, private healthcare settings, and the crucial pre-hospital environment. This broad validation underscores the tool's adaptability and suitability for a wide array of clinical contexts.
The validation process has included substantial academic research, such as a Masters in Philosophy (MPhil) study involving 700 patients from the public sector, another MPhil study with 2000 patients from the private sector, and a doctoral (PhD) investigation. Furthermore, feedback derived from publications in four major scientific journals has also contributed significantly to its refinement.
The current availability of Edition 3 of the SATS training manual serves as a clear indicator of an ongoing process of research, refinement, and adaptation. This iterative approach is crucial for maintaining the tool's accuracy and appropriateness in the dynamic and evolving landscape of emergency medicine. The continuous cycle of research, validation, and revision, as evidenced by successive manual editions, demonstrates a commitment to scientific rigor and ongoing quality improvement. This also implies that the developers are responsive to new evidence and real-world performance data. However, this continuous refinement process also presents a subtle challenge: inconsistent adoption of updates or continued reliance on older versions of the manual could lead to variations in the tool's application and performance across different facilities or regions, potentially undermining the overarching goal of standardization. This highlights the critical importance of effective dissemination and implementation strategies alongside the development of the tool itself.
Beyond the adult population, the Paediatric Triage Working Group (PTWG) of the Western Cape Government has played a pivotal role in developing specialized pediatric triage protocols. This development was informed by integrating principles from existing international tools, specifically the Emergency Triage Assessment and Treatment (ETAT) of the World Health Organization (WHO), with the established framework of SATS. This adaptive evolution demonstrates a commitment to tailoring SATS to cater to the unique needs of specific patient populations and to leverage global best practices in emergency care.
3. Methodology and Core Components of SATS
The South African Triage Scale employs a structured, systematic approach to patient classification, designed to ensure comprehensive and efficient assessment in emergency settings. This methodology is broken down into a five-step process, complemented by a quantitative Triage Early Warning Score (TEWS), a critical discriminator list, and the allowance for senior clinical judgment.
The Five-Step Patient Classification Process
SATS utilizes a systematic, five-step approach to patient classification, ensuring a structured and comprehensive assessment:
Look for emergency signs and ask for the presenting complaint: The triage process begins by eliciting the patient's chief complaint and conducting a rapid assessment for immediate emergency clinical signs. For pediatric patients, a specialized ABC-c-c-DO approach (Airway, Breathing, Circulation, Coma, Convulsion, Dehydration, Other) is utilized. If any emergency clinical signs are identified, the patient is immediately assigned a Red priority level and promptly moved to the resuscitation area, bypassing any further delay or the need for a full Triage Early Warning Score (TEWS) calculation.
Look for very urgent OR urgent signs: If no emergency clinical signs are present, the triage provider proceeds to check for any very urgent or urgent clinical signs that may indicate a need for prompt, though not immediate, intervention.
Measure the vital signs and calculate the TEWS (Triage Early Warning Score): Irrespective of the presence of very urgent or urgent signs (unless emergency signs are already present, which bypasses this step), vital signs are meticulously measured, and the TEWS is calculated. This step introduces a quantitative element to the assessment.
Check key additional investigations: Following vital sign measurement and TEWS calculation, immediate additional investigations are performed. These may include measuring oxygen saturation or blood glucose concentration, as their findings can critically refine or alter the patient's initial triage priority.
Assign final triage priority level: Based on the comprehensive findings from the preceding steps, the final color-coded triage priority level is assigned. Importantly, a senior healthcare professional retains the discretion to override the assigned triage priority, allowing for nuanced clinical judgment.
This multi-layered methodological design represents a deliberate attempt to strike a balance between the desired objectivity and standardization provided by numerical scoring and the critical importance of recognizing specific high-risk clinical presentations that might not be fully captured by vital signs alone. The inclusion of professional discretion acts as a crucial fail-safe, acknowledging that no algorithmic tool can perfectly account for all the complexities and nuances of real-world clinical scenarios. While this sophisticated design aims for comprehensiveness and patient safety, it inherently introduces potential points of variability and error. Subjectivity in interpreting and applying discriminators, or inconsistencies in the exercise of professional discretion, could lead to deviations from optimal triage, as suggested by later findings on suboptimal application. Therefore, the overall effectiveness of SATS relies not only on the robustness of the tool itself but also heavily on the consistent training, accumulated experience, and sound clinical judgment of the healthcare professionals who implement it.
Triage Early Warning Score (TEWS)
The TEWS is a crucial composite score derived from a systematic assessment and scoring of the patient's vital signs, presence of injuries, and mobility status. Each vital sign parameter is assigned a score, typically between 0 and 2, with a higher cumulative score indicating greater clinical urgency.
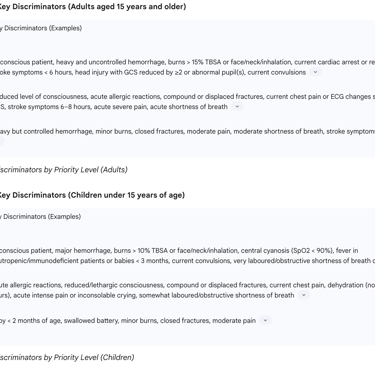
Pediatric TEWS Parameters (for children under 15 years)
Due to significant physiological differences in vital signs across developmental stages, pediatric TEWS tables are meticulously divided into six distinct age categories: Newborn (< 1 month), 1–12 months, 1–3 years, 4–6 years, 7–12 years, and 13–14 years. This high level of age-stratification and parameter customization is a profound acknowledgment of the significant physiological differences and unique vulnerabilities that characterize various pediatric age groups. A vital sign reading considered "normal" for an adult could signify severe pathology in an infant, and certain conditions (e.g., fever in a neonate or a very young baby) carry an inherently higher risk of rapid deterioration. This granularity in the pediatric methodology is absolutely crucial for achieving accurate and safe pediatric triage, where misclassification can lead to extremely rapid and severe adverse outcomes. It underscores the sophistication and clinical foresight embedded within SATS, demonstrating its adaptability to diverse and highly vulnerable patient populations within LMICs, where the burden of pediatric disease is often disproportionately high. However, this added complexity also implies a greater training burden and potential for computational errors if not meticulously followed, a challenge observed in implementation studies.
The specific parameters assessed for children's TEWS include Respiratory rate, SpO2, Heart rate, AVPU, Temperature, and Mobility. A notable difference in pediatric TEWS is the use of Capillary refill time for most child age groups, while Systolic Blood Pressure is specifically utilized for the 13-14 years age group.
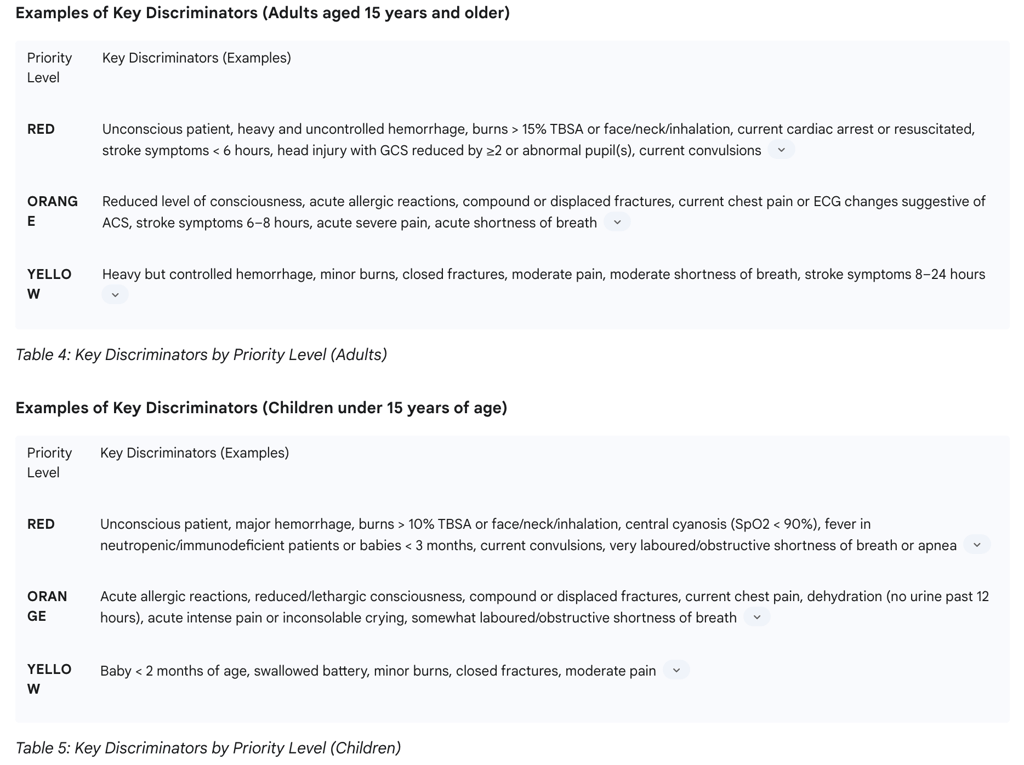
The Discriminator List
The discriminator list is a critical component of SATS, comprising specific symptoms and high-risk clinical conditions that can override the calculated TEWS score and directly guide the assignment of a patient to a Red, Orange, or Yellow priority level. This ensures that conditions requiring immediate attention are not missed, even if vital signs are not yet severely deranged. Footnotes accompanying the discriminator list provide further specification of medical terms and offer guidelines on when to upgrade a patient to a higher priority level, aiding in consistent application.
Additional Investigations and Tasks
Beyond the core TEWS and discriminator assessment, SATS incorporates immediate additional investigations that can further refine triage priority and prompt beneficial actions. These include measuring oxygen saturation (especially if respiratory rate is concerning or child appears cyanotic), performing a finger prick glucotest (for altered consciousness, diabetes history, or severe malnutrition), urine dipstick for ketones (for diabetes with hyperglycemia) or pregnancy (for adult females with abdominal pain), finger prick hemoglobin (for bleeding), and immediate ECG for adult chest pain.
Additionally, SATS outlines "additional tasks" that are beneficial to the patient if initiated at triage but do not alter the assigned priority. Examples include starting Oral Rehydration Therapy (ORT) for dehydrated children, cooling recent burns with water, removing excessive clothing for high temperatures, warming patients with low temperatures, immobilizing closed fractures with a simple splint, and applying direct pressure to active bleeding.
Senior Healthcare Professional Discretion
The final step of the SATS process explicitly allows for a senior healthcare professional to exercise their discretion and override the assigned triage priority. This acknowledges that while the tool provides a structured framework, complex clinical scenarios or unique patient factors may necessitate adjustments based on expert judgment. This provision ensures that the system remains flexible enough to accommodate the nuances of individual patient presentations that might not be fully captured by algorithmic scoring alone.
4. SATS Triage Categories and Urgency Levels
The South African Triage Scale systematically categorizes patients into five distinct color-coded priority levels. This classification is based on a comprehensive assessment of their physiological state, presenting symptoms, and the urgency of their condition. These categories are arranged from the lowest to the highest acuity, each with an associated target time for clinical intervention, which is a defining feature of SATS.
Color-Coded Priority Levels
Green: This color denotes the lowest acuity level, categorized as "routine".
Yellow: This color indicates an "urgent" acuity level, requiring attention within a specific timeframe.
Orange: This color signifies a "very urgent" acuity level, demanding prompt intervention.
Red: This color represents the highest acuity level, categorized as "life-threatening" or an "emergency," requiring immediate action.
Blue: This color is specifically designated for patients who do not show signs of life, indicating they are "deceased". It is important to note that SATS-N, a Norwegian adaptation, may use the Blue category for patients with simple problems where TEWS calculation is deemed unnecessary, based on local guidelines, indicating a slight contextual variation.
Associated Target Times for Clinical Intervention
A defining feature of SATS is the allocation of a specific timeframe within which a patient assigned to a particular priority level should be seen by a medical doctor. These target times are crucial for operational efficiency and patient safety. This explicit time-to-treatment framework elevates triage from a simple patient classification system into a critical operational directive. It provides a clear, actionable mandate for emergency department staff, enabling the efficient and rapid allocation of often-limited human and material resources in high-demand environments. This transforms patient acuity into an operational imperative.
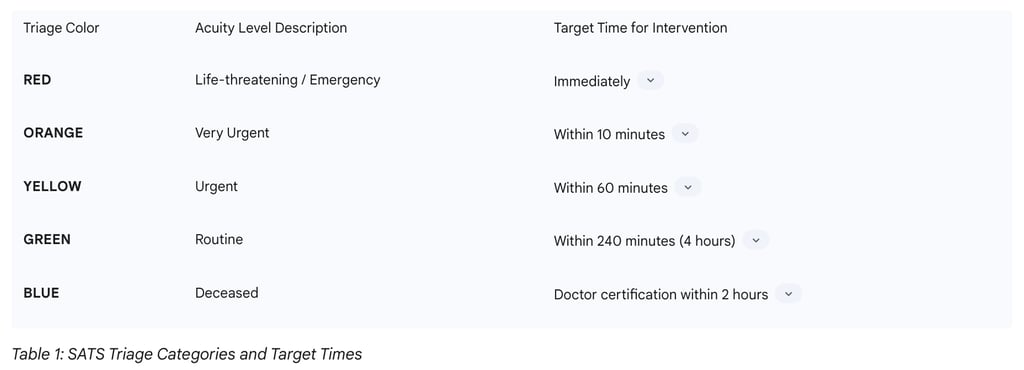
The effectiveness and ultimate success of this system are heavily contingent upon the consistent adherence to these defined target times. Failure to meet these benchmarks, as indicated by some studies , suggests underlying systemic issues. These issues could include chronic overcrowding, persistent staff shortages, or bottlenecks in patient flow, which effectively undermine the very purpose of the triage scale. Such failures can lead to adverse patient outcomes despite accurate initial classification. This direct linkage also establishes these target times as measurable Key Performance Indicators (KPIs) for emergency department efficiency and quality of care.
Upgrade Mechanism
The SATS framework allows for the assigned triage color to be upgraded to a higher acuity level. This is achieved through the identification of specific high-risk clinical discriminators, of which there is a list of 32. These discriminators can critically override the initial TEWS score, ensuring that rapidly deteriorating or inherently high-risk conditions are immediately prioritized, even if the patient's vital signs do not yet fully reflect the severity of their condition.
5. Application Settings and Target Populations
The South African Triage Scale (SATS) is a versatile, physiology and symptom-based scale specifically designed for broad application across various healthcare environments. Its utility extends from the initial point of patient contact through to hospital arrival, serving diverse populations.
Broad Applicability Across Healthcare Settings
SATS is effectively utilized in both hospital Emergency Centres and pre-hospital settings, demonstrating its utility across the continuum of emergency care. This dual application highlights its foundational role in standardizing initial patient assessment regardless of the environment. Its robust validation across diverse healthcare sectors, including public healthcare settings, private healthcare settings, and the pre-hospital environment, further underscores its broad applicability and suitability for a wide range of clinical contexts within South Africa and, by extension, other low- and middle-income countries. This widespread validation indicates that the tool is designed to function effectively despite variations in resource availability and patient demographics across these different settings.
Integration into Clinical Practice
The multi-disciplinary composition of the South African Triage Group (SATG), which developed SATS—including doctors, nurses, and paramedics—inherently signifies its intended integration as a standardized approach across different medical professions. This collaborative development ensures a consistent framework for initial patient assessment regardless of the healthcare provider's specific discipline, fostering inter-professional coherence in emergency care.
The comprehensive SATS training manual serves as a foundational guide, providing healthcare professionals with detailed instructions on its implementation and utilization. This manual emphasizes the core purpose and numerous benefits of standardized triage within emergency care, aiming to equip practitioners with the necessary knowledge and skills for effective application.
Effective SATS implementation is also contingent upon adequate infrastructural support. This includes ensuring patient privacy, maintaining security, and providing necessary equipment such as pulse oximeters, thermometers, and blood glucose monitors, which are essential for accurate TEWS calculation and discriminator assessment. The availability of these basic resources is critical for the tool's proper functioning, particularly in environments where such equipment may be scarce.
The tool's design is noted to be "simple, easy to use and can be used effectively by nursing assistants in emergency centres". This characteristic is particularly significant in resource-constrained LMICs, as it suggests that SATS can facilitate broad adoption and consistent application even among healthcare personnel with varying levels of clinical training and experience. However, this perceived simplicity might inadvertently lead to an underestimation of the training, cognitive load, and ongoing supervision required for accurate triage. While the basic mechanics of the tool may be straightforward, achieving accurate and optimal application appears to demand a deeper understanding, consistent training, and nuanced clinical judgment, especially when dealing with the discriminator list and precise TEWS calculations. This highlights a critical gap between the theoretical design of the tool and its real-world execution, particularly under the high-pressure conditions of emergency care. This necessitates continuous, high-quality professional development and potentially the integration of technological aids (e.g., digital calculators for TEWS) to bridge this implementation gap and ensure that the tool's intended benefits are fully realized.
6. Effectiveness and Impact of SATS
The South African Triage Scale (SATS) was developed with a clear mandate to improve emergency care efficiency. An evaluation of its effectiveness reveals a nuanced picture, demonstrating both significant benefits and notable challenges in its real-world application.
Overall Purpose and Efficiency Claims
The fundamental objective of SATS is to enhance the efficiency of emergency centers by systematically prioritizing severely ill patients. It is scientifically proven to contribute to improved waiting times and the streamlining of emergency center operations, which are critical metrics in high-volume environments. General benefits attributed to SATS include overall improved efficiency, a reduction in patient waiting times, enhanced patient flow through the emergency department, and even improved job satisfaction among staff due to a more organized workflow. These improvements are particularly vital in LMICs where resource limitations often lead to overcrowding and prolonged wait times.
Impact on Patient Outcomes
Predictive Validity
SATS has demonstrated varying degrees of predictive validity across different settings. In diverse trauma settings, specifically in Haiti and Afghanistan, the tool exhibited good predictive validity, accurately forecasting an incremental increase in the likelihood of both mortality and hospitalization across ascending acuity levels (p<0.001). This indicates its utility in identifying patients at higher risk. For patients triaged as 'green' (routine) and 'red' (emergency) in trauma settings, the predicted emergency department outcomes aligned with actual outcomes in a high proportion of cases (84%–99%). In mixed emergency department settings (handling both trauma and non-trauma cases), SATS successfully predicted an incremental increase in hospitalization rates (p<0.001) across both patient categories. Similarly, in pediatric-only settings, SATS demonstrated its ability to predict an incremental increase in hospitalization specifically for non-trauma cases (p<0.001). A study further indicated that only patients initially coded as 'red' had statistically significant odds of being admitted to the hospital, while patients coded as 'green' had significant odds of not being admitted, suggesting a reasonable predictive power for hospital admission.
Specific Study on Penetrating Neck Injuries (PNIs)
A focused study conducted at Tygerberg Hospital (TBH), a high-level trauma center in South Africa, assessed the suitability of SATS for triaging patients with Penetrating Neck Injuries (PNIs). Crucially, this study found no significant association between the SATS categories (both the original recorded categories and recalculated categories) and critical patient outcomes such as the need for resuscitation, urgent surgical intervention, or 7-day mortality (p > 0.05). This specific finding suggests that, in the highly specialized and complex context of PNIs, the SATS colors did not reliably predict these critical patient outcomes, indicating a potential limitation in its specificity for certain trauma types.
This pattern strongly indicates that SATS's effectiveness and validity are not universal but are highly context-dependent. A tool that performs adequately for general trauma or mixed patient populations might not be optimally suited for highly specific, complex injury types (like PNIs) or when applied in distinct operational environments (e.g., the diagnostically limited pre-hospital setting compared to a hospital ED). The inherent difficulty in establishing a definitive "gold standard" for triage further complicates objective assessment, forcing reliance on surrogate markers like mortality or hospitalization, which may not always capture the full spectrum of triage accuracy. This variability means that blanket statements about SATS's effectiveness are insufficient. Its successful implementation requires careful consideration of the specific patient population, the type of injury or illness, and the operational environment. This also points to a continuous need for context-specific validation studies and potentially the development of specialized triage tools or modules for certain high-risk conditions or settings to complement the general SATS framework.
Impact on Emergency Department Flow and Resource Allocation
While SATS is designed with the explicit goals of reducing patient waiting times, streamlining bed occupancy, and improving staff utilization , its actual effectiveness in achieving these outcomes is highly contingent upon its correct and consistent implementation. The finding from the PNI study that SATS was "not optimally applied at TBH" carries significant implications for resource allocation and ED flow. Suboptimal application can lead to under-triaged patients not receiving timely attention or being directed to appropriate, higher-acuity resources, potentially resulting in overcrowding in less critical areas or dangerous delays in life-saving interventions. More broadly, proper triage (a general principle applicable to SATS) is recognized to increase the overall quality of patient care services, enhance patient satisfaction, reduce waiting times and length of stay, and improve the efficiency of emergency departments by strategically prioritizing patients, especially when demand outweighs available resources.
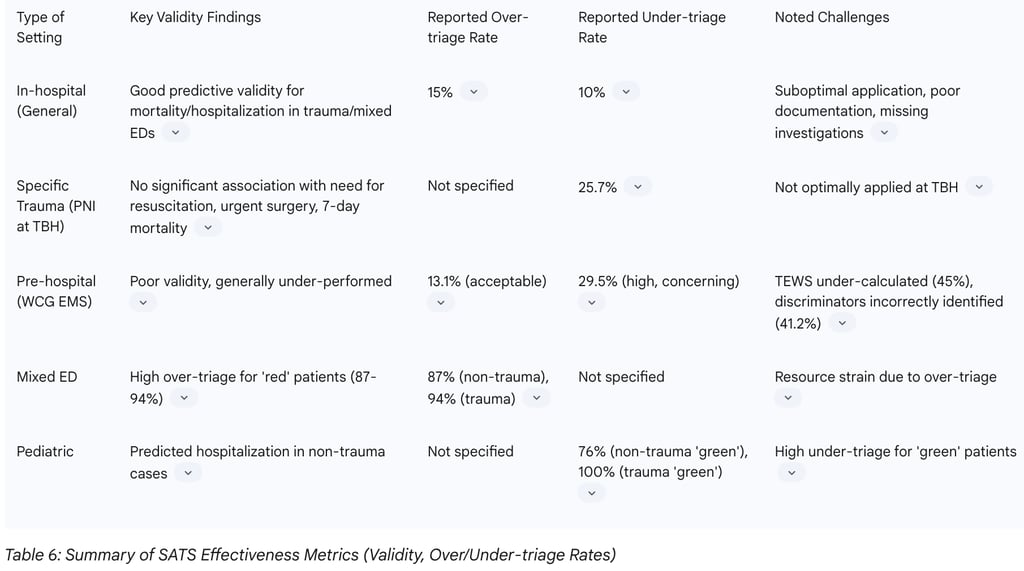
Validity, Over-triage, and Under-triage Rates
The accuracy of SATS application is often evaluated through over-triage and under-triage rates. Over-triage occurs when a patient is assigned a higher acuity level than their true condition warrants, potentially leading to unnecessary resource consumption. Under-triage, conversely, assigns a lower acuity level than warranted, which can dangerously delay critical care.
In-hospital settings: Previous research in South African emergency centers reported SATS having an over-triage rate of 15% and an under-triage rate of 10%.
Pre-hospital settings (Western Cape Government EMS study): A study evaluating SATS use by Western Cape Government Emergency Medical Services (EMS) providers in a pre-hospital setting revealed significant challenges. The final SATS triage color was accurately determined in only 56.5% of clinical vignette responses. A significant and concerning finding was the
under-triage rate of 29.5%, which is notably higher than previously reported in-hospital rates (10%). This is a critical limitation, as under-triage can lead to acute patients being transported to hospitals with lower levels of care, not receiving necessary pre-hospital ambulance care, or experiencing medically harmful delays in definitive care. The over-triage rate in this pre-hospital context was 13.1%, which was considered acceptable, as over-triage, while potentially leading to wasteful interventions, is generally viewed as less detrimental than under-triage. Further analysis revealed that the TEWS was calculated correctly in only 42.6% of vignettes, and notably, it was
under-calculated in 45.0% of responses. Discriminators, a critical component, were correctly identified in only 58.8% of vignettes, with significant errors observed particularly in trauma and neurologic discriminators. The study concluded that SATS generally under-performed as a pre-hospital triage tool, primarily due to issues with clinical discriminators, and demonstrated poor validity despite good inter-rater reliability.
Mixed ED settings: Some studies reported high over-triage rates for 'red' patients (87% for non-trauma and 94% for trauma cases), suggesting potential for resource strain if these patients do not truly require immediate, high-level intervention.
Paediatric settings: A concerning finding indicated that 76% of 'green' non-trauma patients and 100% of 'green' trauma patients in pediatric settings were undertriaged.
The consistently significant rates of under-triage, especially in pre-hospital environments, represent a critical and potentially dangerous flaw in the practical application of SATS. This directly compromises patient safety by delaying critical, time-sensitive interventions for those who are most in need. The explicit mention of "medically harmful" consequences underscores the severity of this issue. The higher under-triage rates in pre-hospital settings strongly suggest a fundamental mismatch between the tool's original design (primarily for in-hospital use) and the inherent diagnostic limitations, environmental challenges, and operational pressures of the pre-hospital environment. This necessitates urgent and targeted interventions, which may include intensive re-training, significant adaptation of the tool for pre-hospital use, or even the exploration of entirely alternative triage strategies specifically for these challenging contexts, to mitigate preventable harm and ensure equitable access to timely, appropriate care.
The table below summarizes key effectiveness metrics for SATS across various settings:
7. Conclusion
The South African Triage Scale (SATS) represents a vital and strategically designed tool for emergency care, particularly within the challenging contexts of low- and middle-income countries. Its development by a multidisciplinary team and subsequent iterative refinement, evidenced by successive training manual editions and extensive validation studies, underscore a commitment to providing an evidence-based, adaptable framework for patient prioritization. The structured five-step methodology, integrating objective physiological scoring via the Triage Early Warning Score (TEWS) with a critical discriminator list, and allowing for senior clinical discretion, reflects a sophisticated attempt to balance standardization with the nuanced complexities of clinical presentation. The explicit linkage of color-coded priority levels to specific target times for intervention transforms triage into a crucial operational directive, essential for efficient resource allocation in high-demand environments.
Despite these inherent strengths and its demonstrated predictive validity in general trauma and mixed emergency department settings, the real-world application of SATS reveals significant challenges. The most critical concern centers on consistently high rates of under-triage, particularly in pre-hospital environments and for specific, complex injury types such as penetrating neck injuries. This under-triage, which can lead to delayed or inappropriate care, poses a direct and medically harmful threat to patient safety. Furthermore, observed inconsistencies in the accurate calculation of TEWS and the correct identification and application of discriminators, especially in pre-hospital settings, suggest a gap between the tool's intended "simple and easy to use" design and the cognitive demands of its precise execution under pressure. This disparity points to a fundamental need for continuous, high-quality training and potentially a re-evaluation or adaptation of certain aspects of the tool to better suit the diagnostic limitations and operational realities of diverse clinical environments.
In conclusion, while SATS provides a robust and essential framework for emergency care triage in resource-constrained settings, its full potential is realized only through meticulous and consistent application. Moving forward, efforts must focus on targeted professional development, particularly emphasizing the accurate use of discriminators and TEWS calculation. Consideration should also be given to adapting the tool or developing complementary modules for specialized contexts, such as pre-hospital care and specific trauma presentations, to mitigate the risks of under-triage. Continuous quality improvement initiatives, informed by ongoing performance data, are paramount to ensuring that SATS remains an effective instrument for optimizing patient outcomes and enhancing the efficiency of emergency departments across South Africa and beyond.
Additional Resources
Emergency Medicine Society of South Africa (EMSSA) SATS Resources Comprehensive training materials, implementation guides, and ongoing support for SATS adoption. Available at: https://emssa.org.za/special-interest-groups/the-south-african-triage-scale-sats/
World Health Organization Emergency Care Systems Framework International guidelines for emergency care development with specific sections on triage system implementation in low- and middle-income countries.
Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine Regular publications of SATS validation studies and implementation research from diverse international settings.
BMC Emergency Medicine Triage Collection Comprehensive academic research collection focusing on triage system development, validation, and implementation across different healthcare contexts.
International Association for Healthcare Social and Medical Innovation Resources for implementing evidence-based healthcare innovations, including systematic triage programs in resource-limited settings.
