Pediatric-Specific AI Triage Models
Explore the unique challenges and advancements in AI triage models tailored for paediatric healthcare. Discover how these innovative systems are revolutionising emergency care for children.


The integration of artificial intelligence (AI) into healthcare triage systems presents a transformative opportunity, particularly within pediatric emergency care. This report provides a comprehensive overview of pediatric-specific AI triage models, highlighting their profound potential while addressing critical implementation challenges. A fundamental premise is the recognition that children are not merely "small adults"; their unique physiological and developmental characteristics necessitate specialized AI models. The evidence demonstrates that these tailored AI systems offer significant advancements in diagnostic accuracy, operational efficiency, and patient outcomes, moving beyond the inherent limitations of conventional, often subjective, triage methods. However, the successful and equitable deployment of AI in this sensitive domain requires meticulous attention to data quality, the mitigation of algorithmic biases, the cultivation of clinician trust through transparency, and the establishment of robust, child-centered ethical governance frameworks. This analysis underscores the imperative for continued research, multi-center validation, and collaborative development to fully realize the benefits of AI in safeguarding and improving the health of pediatric patients.
Overview of Triage in Emergency Departments
Triage systems are foundational components of healthcare infrastructure, designed to prioritize patients based on the severity of their medical conditions, thereby ensuring that those in most urgent need receive timely care. Within emergency departments (EDs), this process involves the rapid assessment of incoming patient information, the classification of urgency, and the efficient direction of individuals to appropriate workflows. This systematic approach is indispensable, especially considering the substantial daily volume of patient arrivals and the overwhelming influx of data generated from vital signs, laboratory results, and clinical notes.
AI triage systems represent a technological evolution in this domain. They are defined as software applications engineered to automate medical history-taking and triage functions within primary care settings, while also providing crucial support for clinical decision-making and overall patient management. The foundational role of triage in mitigating mortality risk cannot be overstated. The process is not merely an operational efficiency concern; it directly influences patient survival. For critical conditions such as sepsis or acute myocardial infarction, studies indicate that each hour of delayed intervention can increase mortality risk by up to 7.6%. This quantifiable link between delayed care and increased mortality underscores the high-stakes nature of emergency department triage and establishes the profound importance of developing advanced AI systems to enhance patient outcomes and reduce preventable deaths, particularly in time-sensitive medical emergencies.
Why Children Are Different: Unique Pediatric Physiological and Developmental Considerations
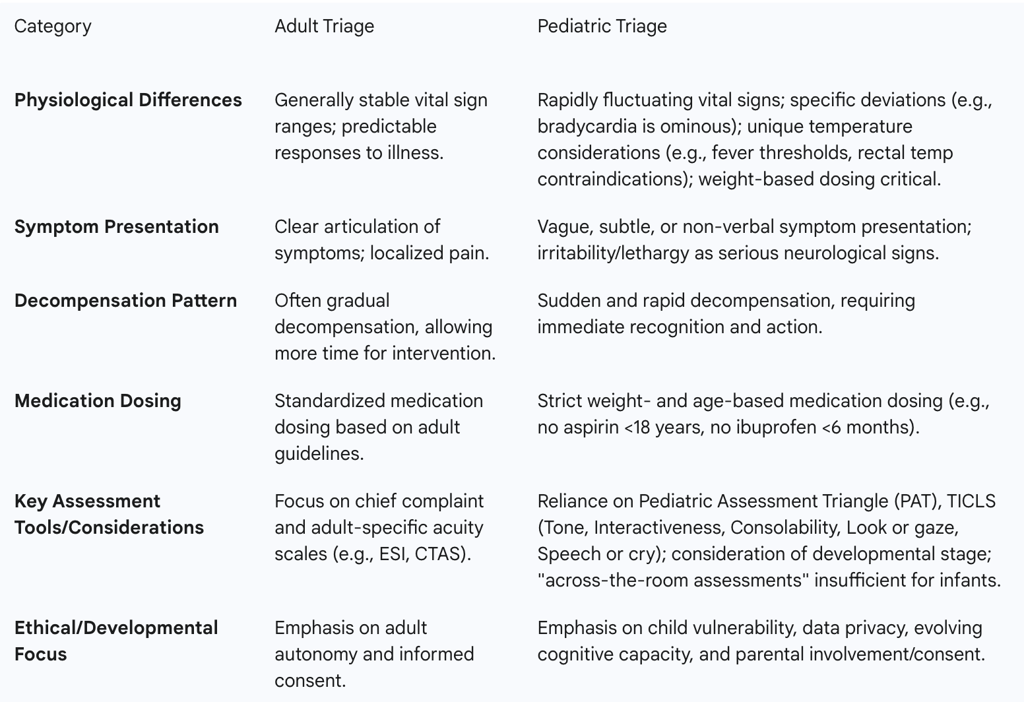
A cornerstone principle in pediatric medicine, frequently emphasized by clinicians, is that "children are not small adults". This fundamental distinction extends across their physiology, anatomy, patterns of injury, and responses to illness, all of which differ significantly from those observed in adults. Consequently, providing safe and effective pediatric emergency care demands specialized knowledge and unique clinical skills.
Pediatric patients frequently present with vague or undefined complaints, and their conditions can decompensate with alarming suddenness. The signs and symptoms of serious illness in children are often subtle and may manifest abruptly, making initial assessment particularly challenging. Specific physiological differences further complicate the triage process:
Bradycardia: A slow heart rate in a child is considered an ominous sign, signaling potential severe underlying issues.
Temperature: A history of high temperature in infants and immunocompromised children prior to arrival can indicate significant illness, even if their temperature appears normal at the time of triage. Furthermore, rectal temperature measurements are contraindicated in immunocompromised children due to the risk of proctitis and sepsis. Specific fever thresholds, such as temperatures above 100.4 °F (38 °C) in neonates younger than three months, are recognized as critical red flags.
Medication Dosing: Healthcare professionals must be acutely aware of age limits for certain medications and meticulously adhere to correct weight-based dosing. For example, aspirin is generally contraindicated for children under 18 years old, and ibuprofen should not be given to infants under six months or when chickenpox is suspected.
Blood Pressure: Obtaining accurate blood pressure readings in small children and infants can be challenging due to crying, movement, and the difficulty in selecting the appropriate cuff size. Conversely, elevated blood pressure in adolescents, especially when accompanied by symptoms like headache, nausea, shortness of breath, or chest pain, warrants careful attention.
Capillary Blood Glucose (CBG): This is a crucial measurement for determining acuity, particularly for patients who may experience delays in accessing a treatment bed or those presenting with altered mental status. Specific high-risk thresholds for low and high blood glucose levels exist for neonates and older children.
Beyond physiological distinctions, developmental considerations are paramount. "Across-the-room assessments" are often insufficient for neonates and infants, who may harbor hidden deficits that are not immediately apparent. Altered mental status in a child, manifesting as irritability (beyond fussiness) or lethargy (beyond drowsiness), indicates a serious neurological event that demands immediate and serious attention. This detailed understanding of pediatric presentation reveals why conventional, often adult-centric, triage methods are inherently inadequate and potentially dangerous for pediatric patients. It underscores the immense cognitive load and specialized training demanded of human clinicians, which traditional subjective systems struggle to standardize. This directly builds the case for AI models specifically designed to process and interpret these unique pediatric complexities, as they can offer a more consistent and objective assessment than human judgment alone.
Table 1: Key Differences: Adult vs. Pediatric Triage Considerations
Limitations of Conventional Pediatric Triage Methods
Conventional pediatric triage systems predominantly rely on subjective evaluations performed by healthcare professionals. This inherent subjectivity is a significant weakness, frequently leading to inconsistencies and inaccuracies in patient categorization. For instance, the Emergency Severity Index (ESI), a widely adopted triage tool, often depends on individual clinicians' opinions rather than objective, factual criteria. This reliance can result in either over-triaging, where a patient is assigned a higher urgency than medically necessary, or, more critically, under-triaging, where a serious condition is overlooked or deprioritized.
The variability in clinicians' experience levels further exacerbates these issues, as different individuals may interpret signs and symptoms distinctly. The inherent difficulty young children face in articulating their feelings or symptoms also complicates accurate evaluations, adding another layer of challenge to human-led assessments. Moreover, a child's health status can change with remarkable speed, rendering an initial assessment inaccurate within a short timeframe. Studies analyzing traditional triage methods have reported a mistriage rate of 1.2% , underscoring the urgent need for more objective and reliable approaches. These collective problems contribute to erroneous triage decisions, prolonged wait times, overcrowded emergency rooms, and pose significant risks to patient safety if critical cases are overlooked.
These observations reveal fundamental systemic vulnerabilities within conventional triage. The inherent subjectivity, when combined with the unique complexities of pediatric patients, creates a high propensity for errors, encompassing both over- and under-triaging. Such errors not only compromise individual patient safety but also lead to broader operational inefficiencies, such as longer wait times and ED overcrowding, and can even result in potential legal liabilities for healthcare providers. This analysis directly sets the stage for AI's value proposition: its capacity to introduce objectivity, consistency, and data-driven precision where human judgment is prone to variability and cognitive overload.
Defining Pediatric AI Triage Models
Core Architecture and Data Flow
AI triage systems are sophisticated software applications designed to automate medical history-taking and triage processes, actively supporting clinical decision-making and patient management in both primary care and emergency settings. These systems function much like highly skilled dispatchers, adeptly assessing incoming information, classifying it by urgency or type, and efficiently directing each item to the appropriate downstream workflow.
The typical operational breakdown of a Triage AI Agent involves several interconnected components that facilitate its functionality :
Data Ingestion: This foundational phase is responsible for capturing and centralizing incoming information from a multitude of diverse sources. These sources include medical devices, electronic health record (EHR) systems, and direct user inputs. The data is then transformed into a consistent, structured format, making it ready for subsequent analysis.
Feature Extractor: In this stage, raw data is transformed into meaningful attributes or "features." This involves the extraction, combination, or summarization of relevant details that enable the downstream models to understand the clinical context and make accurate decisions.
Assessment Engine: This is the central processing unit of the AI triage system. It evaluates the processed data points by applying learned patterns or predefined rules to assign risk levels and categorize patient cases. Integrated decision logic then directs each case to the appropriate workflow; urgent cases trigger immediate action, while lower-priority items follow standard review processes.
Alert Dispatch: This mechanism is responsible for disseminating notifications or directing tasks to the correct recipients and channels. This can include dashboards, messaging applications, or automated workflows, all based on the assigned priority and category of each patient item.
Feedback Loop: This component is crucial for the continuous improvement and refinement of the AI system. It involves the ongoing monitoring of handled cases, meticulous recording of actions taken, and measurement of timeliness and accuracy. These results are then fed back into the system to continuously refine its rules and models. A vital aspect of this loop is an "override" mechanism that allows clinicians to flag misrouted alerts, with these corrections being incorporated back into the training data to enhance future performance.
The operational stages of an AI triage system, particularly the robust feedback loop, underscore that these models are not static, fixed programs. Instead, they are engineered to be dynamic, learning, and continuously improving based on real-world performance and direct human oversight. This iterative and adaptive nature is paramount for building trust and ensuring the system's reliability, especially in a complex and rapidly evolving domain like pediatric emergency medicine, where subtle presentations and swift changes in patient condition are common. Furthermore, it implies that successful AI implementation necessitates not just robust algorithms but also a well-defined infrastructure for continuous data collection, error flagging, and model retraining, emphasizing the necessity of ongoing collaboration between AI developers and clinical staff.
Key Data Inputs for Pediatric AI Triage
AI-driven triage systems achieve patient prioritization by analyzing a comprehensive array of real-time data, including vital signs, extensive medical history, and presenting symptoms. These systems can also integrate demographic information, such as gender and age, to construct a more holistic and nuanced patient profile.
Specific input features commonly utilized within pediatric emergency department (PED) triage environments are critical for accurate assessment. These include the patient's gender and age, their mode of arrival, the frequency of PED visits within the last 72 hours (which can serve as a proxy for acuity), time of arrival, and key physiological parameters such as temperature, systolic blood pressure, and diastolic blood pressure.
The seamless integration of AI triage systems with Electronic Health Records (EHR) is not merely beneficial but crucial for providing real-time advice and ensuring optimal system performance. EHRs serve as comprehensive repositories of patient visits, test results, and scan data, offering rich historical context that is invaluable for AI models. Studies consistently indicate that AI models, when effectively integrated with EHRs, can predict serious outcomes like hospital stays or Intensive Care Unit (ICU) transfers with high accuracy, often achieving scores above 0.80.
Furthermore, emerging technologies, such as wearable devices, are poised to become increasingly important data sources. These devices can capture critical physiological data points like heart rate, respiratory rate, and oxygen saturation, which are vital in identifying patients at risk of deterioration. The synergistic combination of historical health data from EHRs with real-time clinical observations significantly enhances the overall effectiveness and predictive power of AI models, moving beyond simple, snapshot vital sign checks to a truly holistic, multi-modal data approach. This comprehensive data integration is essential for synthesizing vast, disparate datasets that are often siloed or difficult to access in traditional systems, pointing to a significant underlying infrastructure challenge in ensuring seamless, secure, and standardized data flow for comprehensive analysis.
Role of Machine Learning Algorithms
Machine learning (ML) involves the use of algorithms that learn from data to improve their predictions and performance over time. In the context of pediatric emergency care, these algorithms analyze large datasets of past patient information, enabling more accurate and consistent classifications of patient urgency. This data-driven approach is instrumental in reducing misclassification errors and providing objective guidance to clinicians for more timely and accurate treatment decisions.
Unlike conventional triage methods that heavily rely on subjective human judgment, machine learning models are designed to identify complex patterns within vast amounts of historical patient data that human observers might easily miss. This capability is particularly advantageous in pediatric cases, which are inherently complex, characterized by subtle cues, vague symptoms, and rapid changes in condition. Simple rule-based or linear predictive models often struggle to capture these nuanced, non-linear relationships.
Among the various algorithms reviewed, ensemble models, particularly the CatBoost algorithm, have demonstrated exceptionally high effectiveness in pediatric triage. CatBoost is noted for its ability to simultaneously process and utilize a multitude of clinical factors, accurately sort patients into appropriate urgency categories, and significantly lower the incidence of both over-triaging (assigning unnecessarily high urgency) and under-triaging (missing critical cases). Ensemble methods, by combining the predictive power of multiple individual models, are inherently more robust and adept at identifying intricate patterns within diverse data, making them particularly well-suited for the multi-factorial and often ambiguous nature of pediatric presentations. This suggests that future research and development in pediatric AI triage should prioritize the exploration and refinement of such robust, complex algorithmic approaches over simpler AI methodologies.
Performance Metrics and Improved Accuracy
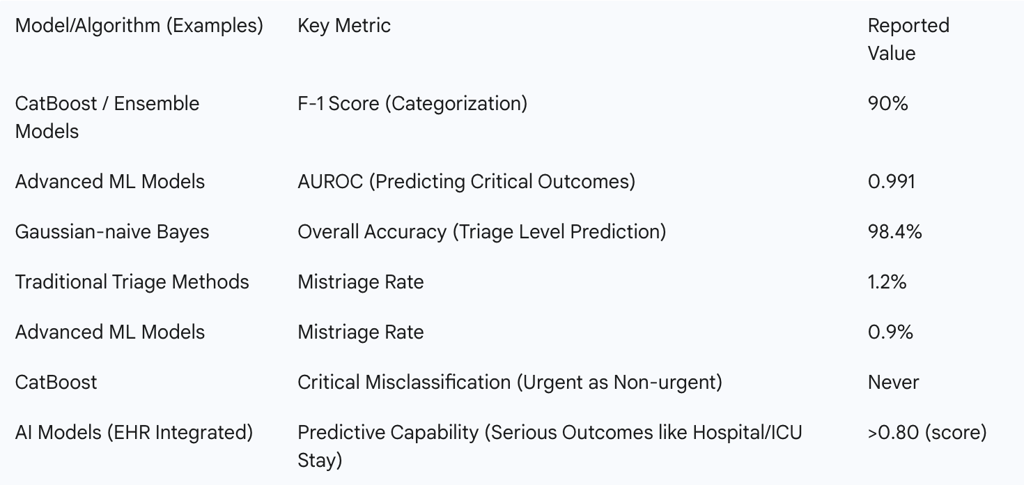
Machine learning models have consistently demonstrated superior discrimination abilities when compared to conventional triage systems. The integration of AI into the triage process yields significant enhancements in predictive accuracy, disease identification, and risk assessment.
Advanced ML models, such as CatBoost, have achieved a remarkable 90% F-1 score in categorizing pediatric patients. This represents a significant improvement over the performance of traditional triage methods. The mistriage rate has been notably reduced to 0.9% with the application of ML models, a decrease from the 1.2% rate reported for traditional triage methods. Crucially, one study highlighted that the developed model "never misclassified an urgent patient as nonurgent or vice versa" , indicating a high degree of safety and reliability in critical classifications.
Furthermore, models have achieved an Area Under the Receiver Operating Characteristic curve (AUROC) of 0.991 in predicting critical outcomes , setting an exceptionally high benchmark for accuracy in patient evaluation. Another study reported a Gaussian-naive Bayes model achieving 98.4% accuracy in predicting triage levels. These models also demonstrate strong predictive capabilities for serious outcomes, such as the need for hospital stays or Intensive Care Unit (ICU) transfers, consistently achieving scores above 0.80. This collection of data points indicates that AI in pediatric triage offers not just marginal improvements but a significant leap in accuracy and, more importantly, safety. The ability to avoid misclassifying urgent cases as non-urgent directly addresses a major patient safety concern in emergency medicine. This robust, quantifiable evidence of superior performance provides a strong empirical foundation for advocating for the widespread adoption of AI, demonstrating its direct potential to reduce adverse events and improve patient outcomes by ensuring that critical cases receive immediate and appropriate attention.
Table 2: Performance Metrics of Advanced Machine Learning Models in Pediatric Triage
Transformative Benefits and Impact on Patient Outcomes
Accelerated Response and Reduced Wait Times
AI triage agents possess the capability to surface critical patient alerts in under 10 seconds, representing a dramatic acceleration compared to typical manual triage times of 3-5 minutes. This rapid assessment ensures that critically ill patients are prioritized significantly faster, thereby reducing dangerous delays in administering life-saving interventions. Real-world use cases in emergency departments have demonstrated a typical impact of a 20% reduction in door-to-treatment time, achieved by automatically ranking incoming ambulances based on projected patient severity. Automated triage systems further contribute to improved operational efficiency and enhanced patient safety within the emergency department by accurately categorizing patients based on their potential for adverse outcomes.
This ability to dramatically compress the critical time window from patient arrival to the initiation of intervention is a profound advantage. In pediatric emergency care, where patient decompensation can be exceptionally rapid and unpredictable, this speed is not merely an efficiency gain but a direct and often life-saving determinant of survival and long-term neurological or physical outcomes. This positions AI as an indispensable tool for optimizing the "golden hour" or "platinum ten minutes" of emergency care, directly translating to improved survival rates and reduced morbidity for pediatric patients.
Optimized Resource Allocation and Reduced Clinician Burnout
AI-driven triage systems are highly effective in optimizing resource allocation. They achieve this by intelligently and automatically adjusting patient prioritization based on real-time conditions and the current availability of resources. This ensures the most efficient deployment of critical resources, including staff, beds, and diagnostic tools.
Beyond immediate triage, AI models can predict bed availability and patient transfer needs, extending this capability across multiple facilities to enhance regional visibility of care capacity and streamline patient transfers. By streamlining patient flow and enabling smarter resource utilization, AI can free up beds more quickly for new emergencies and significantly lower the workload on staff, thereby helping to prevent medical mistakes and reduce clinician burnout. AI also contributes to reduced alert fatigue by ensuring that automated rules apply identical triage criteria consistently, 24/7, effectively eliminating human variability and subjective interpretations. Furthermore, AI can optimize physician shifts based on forecasted patient volume, ensuring appropriate workforce distribution and improving overall hospital staff management. While this potential has been demonstrated, the need for more validated studies in real-world settings is acknowledged.
The multifaceted impact of AI on resource allocation and staff well-being highlights its potential to transform emergency department operations from a reactive, often chaotic environment into a more proactive, strategically managed, and resilient system. By accurately predicting demand and optimizing the deployment of critical resources (staff, beds, equipment), AI can significantly enhance the overall capacity and responsiveness of the healthcare system, particularly in high-volume pediatric EDs. This not only directly improves patient care by reducing wait times and ensuring resource availability but also addresses the critical and growing issue of clinician well-being and retention, which has profound long-term implications for the sustainability and quality of healthcare delivery.
Enhanced Diagnostic Accuracy and Predictive Capabilities
AI models consistently demonstrate superior performance in diagnostic accuracy, with a pooled area under the receiver operating characteristic curve (AUC) of 0.88, and in outcome prediction. For instance, AI models have been shown to predict the onset of sepsis several hours before the appearance of clinical symptoms, enabling significantly earlier intervention. AI can accurately assess the severity of traumatic brain injuries and predict the risk of intra-abdominal injuries, providing critical data that supports timely and accurate decision-making.
AI-powered diagnostic tools are now being utilized to identify diseases such as childhood asthma, congenital heart defects, and even autism spectrum disorders earlier than ever before. In neonatal intensive care units (NICUs), machine learning systems continuously monitor real-time vital signs and can alert clinicians to the early signs of sepsis or respiratory distress before a human eye might detect these subtle changes. A large, prospectively validated study demonstrated that a machine learning-based scoring system for pediatric appendicitis achieved an impressive AUC of 0.996, an accuracy of 0.992, a sensitivity of 0.998, and a specificity of 0.993. This performance significantly outperformed traditional clinical scoring systems, highlighting AI's potential to reduce diagnostic delays and unnecessary imaging.
These observations extend beyond simple triage to highlight AI's capacity for proactive and precision medicine. By identifying subtle patterns and predicting critical outcomes significantly earlier than human clinicians, AI enables a fundamental shift from reactive treatment to proactive intervention. This is especially vital in pediatrics, where rapid deterioration is a constant concern. This capability not only improves individual patient outcomes by allowing for earlier, potentially less invasive, and more effective treatments but also has the broader potential to reduce the burden of severe disease by preventing escalation of conditions.
Navigating the Landscape: Challenges, Limitations, and Ethical Considerations
Data Quality, Scarcity, and Diversity Issues
The efficacy of AI models is fundamentally dependent on the quality and completeness of the data used for their training. Unfortunately, emergency department data often contains missing details, which AI systems must be robust enough to handle. A paramount challenge in deploying AI in pediatric emergency medicine (PEM) is ensuring the availability of high-quality, diverse, and representative data for training AI models. The effectiveness and generalizability of AI systems are directly correlated with the data used during their development.
If training data lacks diversity, for example, across different demographics, socioeconomic backgrounds, or clinical settings, it can lead to biased outcomes and potentially exacerbate existing healthcare disparities. Models predominantly trained on data from specific populations may not perform well across different patient groups or environments, significantly reducing their applicability and generalizability. This limitation is particularly acute in PEM, where patient conditions and responses can vary significantly across age groups and backgrounds. Most current research on AI triage in U.S. children's hospitals originates from single institutions or relies on retrospective data. To ensure that AI solutions are broadly applicable and effective across diverse patient populations and hospital systems, larger, multi-center, and prospective validation studies are critically needed.
The observation that "conclusions can only be as reliable (but also as neutral) as the data they are based on" points to a foundational limitation that can severely undermine the entire promise of AI in healthcare. If the training data is of poor quality, incomplete, or unrepresentative (e.g., lacking diverse pediatric populations, socioeconomic backgrounds, or complete historical records), the AI model will inevitably inherit and perpetuate these flaws, leading to inaccurate, biased, and potentially harmful predictions. This necessitates not just technical solutions for data cleaning and imputation but also significant strategic investment in data infrastructure, standardization across institutions, and collaborative data-sharing initiatives across multiple centers to build truly robust, equitable, and generalizable pediatric AI models. It also highlights the critical need for rigorous data governance and continuous auditing throughout the AI lifecycle.
Addressing Bias in AI Models (Age, Socioeconomic Status)
Children remain significantly overlooked in the development of medical AI, with only 17% of FDA-approved medical AI devices specifically labeled for pediatric use. This exclusion largely stems from a fundamental data gap: children represent less than 1% of available public medical imaging datasets, despite the majority of machine learning imaging conference papers utilizing publicly available data for method development. This lack of pediatric representation leads to demonstrable age bias. For instance, adult-trained chest radiograph models exhibit significant age bias when applied to pediatric populations, resulting in higher false positive rates in younger children. This gap in representation translates directly to biased predictions across medical image foundation models, with the youngest patients facing the highest risk of misdiagnosis.
Socioeconomic status (SES) is another critical dimension along which AI models can exhibit bias, leading to disparate performance across different demographic subgroups. Evidence suggests that a lack of healthcare access among individuals of lower SES can lead to lower-quality healthcare data for these patients. This, in turn, provides less valid signal for AI models to pick up, ultimately resulting in lower performance and accuracy for those of lower SES. Furthermore, algorithmic actions can be discriminatory solely based on their effect on a protected class, even if the underlying evidence seems sound.
This is a critical ethical and practical challenge that extends beyond technical fixes. The existing data landscape is inherently biased against vulnerable pediatric populations and underserved communities. Deploying AI models trained on such skewed data risks not only perpetuating but actively amplifying existing health disparities, leading to inequitable and potentially harmful care. Addressing this requires not just technical solutions (e.g., collecting more diverse data, bias detection algorithms) but also significant policy interventions, the development of robust ethical frameworks, and a conscious, unwavering commitment from AI developers, healthcare institutions, and policymakers to prioritize equity, fairness, and inclusion in every stage of AI design, development, and deployment, especially given the inherent vulnerability of children.
Integration into Clinical Workflows, Clinician Trust, and Transparency
Despite promising results in research, the successful implementation of AI solutions into existing clinical workflows remains a challenging task that currently hinders their widespread real-world application. Healthcare professionals frequently express concerns about AI potentially replacing human judgment or diminishing the human element of patient care, which can lead to significant resistance to adoption. Ensuring that AI technologies are perceived as tools that complement, rather than replace, human judgment and that they align seamlessly with established clinical environments is crucial for successful integration.
A major barrier to the effective use of AI in pediatric emergency medicine is the pervasive lack of transparency in many AI systems, particularly those often referred to as "black box" models, where the decision-making process is opaque. To mitigate this, tools like SHapley Additive exPlanations (SHAP) and LIME (Local Interpretable Model-Agnostic Explanations) are being utilized to help explain how AI models arrive at their decisions, thereby fostering trust among clinicians and encouraging their use in patient care. Clinicians require specific training to understand and properly utilize AI tools. Developing "AI literacy"—understanding the fundamental functions of AI and how to use these applications effectively and responsibly—is key for all medical professionals. A significant knowledge gap currently exists between clinicians, engineers, and data scientists, which impacts effective collaboration and adoption.
The observations regarding AI integration, clinician trust, and transparency underscore that technological sophistication and algorithmic accuracy alone are insufficient for successful AI adoption in clinical settings. The human element—specifically, clinician trust, understanding, and willingness to integrate AI into their daily workflows—is paramount. This necessitates not only the development of robust and accurate AI models but also significant investment in designing user-friendly interfaces, implementing explainable AI (XAI) tools, and providing comprehensive, ongoing education and training for healthcare professionals. AI should be strategically positioned and communicated as an augmentative tool that enhances human capabilities, rather than a replacement, to foster acceptance and ensure that human oversight, critical thinking, and ethical judgment remain central to patient care.
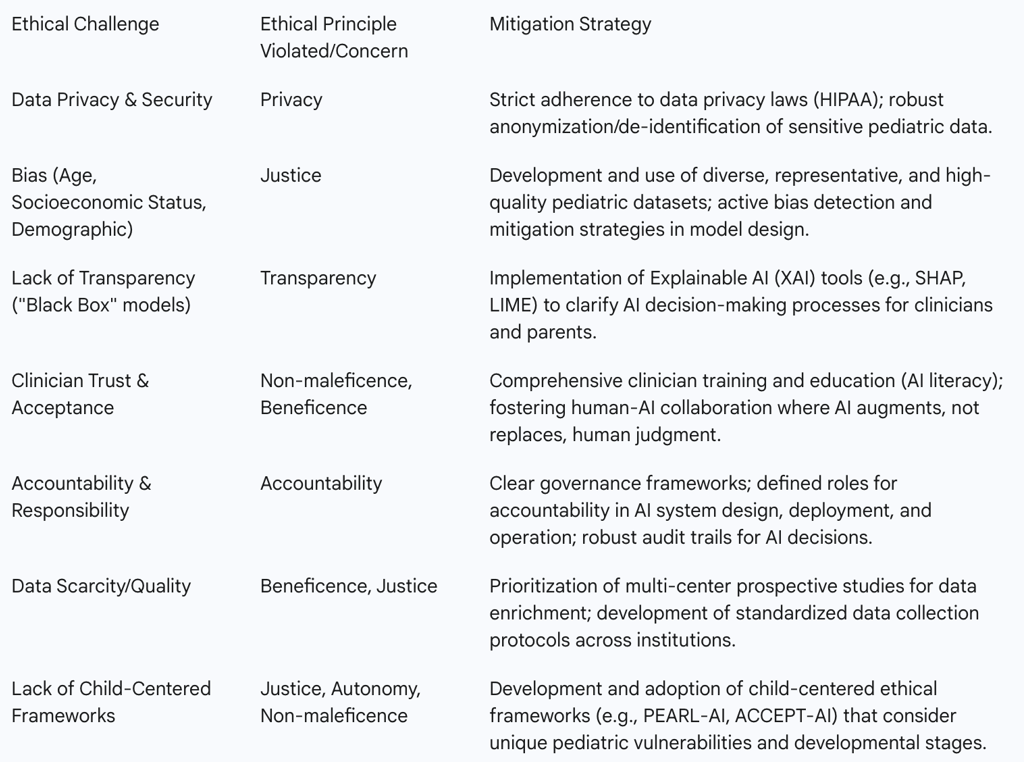
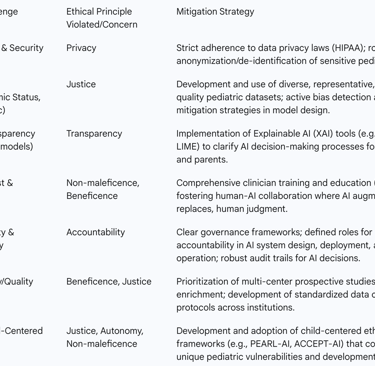
Ethical Principles and Child-Centered AI Governance
Children's health data is exceptionally sensitive, requiring strict adherence to privacy laws such as HIPAA. AI systems must be designed to keep patient data safe and anonymous whenever possible. Healthcare institutions must carefully consider ethical implications to maintain patient trust and actively avoid algorithmic bias.
A significant gap exists in the current landscape: there is a notable lack of comprehensive reviews or specific guidelines on AI ethics tailored for child health, unlike the more established frameworks in adult medicine. This is particularly problematic given that children are not merely miniature adults; they undergo unique age-associated changes in organ function and neurodevelopment, necessitating a distinct, child-centered approach to medical AI. Recognizing this gap, frameworks such as the "Recommendations for the Safe Inclusion of Pediatric Data in Artificial Intelligence and Machine Learning Research" (ACCEPT-AI) have been proposed. This framework aims to guide the creation of secure and reliable pediatric-tailored AI applications, explicitly taking into account the anatomical and physiological distinctions between adults and children.
Key ethical principles that must be meticulously considered for child-centered AI include non-maleficence (do no harm), beneficence (do good), autonomy (respect for decision-making, considering evolving capacity), justice and transferability (equitable access and performance across diverse populations), transparency and explainability, privacy, dependability, auditability, knowledge management, accountability, and fostering trust. The absence of specific pediatric AI guidelines, coupled with the explicit need for child-centered AI development, reveals a significant regulatory and ethical vacuum. Given children's inherent vulnerability, their evolving cognitive abilities (which impact their capacity for autonomy), and the extreme sensitivity of their health data, a generic "adult" AI ethics framework is demonstrably insufficient. This calls for proactive policy development, robust interdisciplinary collaboration (involving ethicists, pediatricians, legal experts, and AI developers), and continuous ethical oversight to safeguard children's rights and ensure their well-being in the age of AI.
Table 3: Ethical Challenges and Mitigation Strategies in Pediatric AI Triage
Current Landscape: Prototypes, Pilot Programs, and Real-World Applications
While the progression of AI models beyond the prototype phase into widespread real-world clinical application remains limited, with less than 2% of AI models progressing beyond this stage , several notable examples and pilot programs demonstrate the significant potential of pediatric-specific AI triage and broader AI applications in emergency care.
Case Studies and Implementation Examples
AIIMS Raipur (India): In a collaboration with IIT Bhilai, AIIMS Raipur developed an Intelligent Emergency Care System (iECS) designed to provide real-time guidance to emergency care providers for faster and more accurate decisions. While the pilot project on heart attack patients (using an algorithm trained on over 14,000 ECGs) was not pediatric-specific, it achieved a 73% thrombolysis success rate, demonstrating the core principle of AI-enabled decision support in acute care. They also developed an Automated Triage in ER system that uses predictive models to categorize patients based on potential adverse outcomes, improving operational efficiency and patient safety.
York University (UK): Researchers are developing a prototype Diagnostic AI System for Robot-Assisted A&E Triage (DAISY). This system integrates AI software to collect patient data (including symptoms and vital signs) with a 'social robot' that guides patients (who consent) to measure their own vital signs. The underlying hypothesis is that this interaction will enhance communication effectiveness, reduce patient waiting times, and alleviate clinician workload. A 'test-bed,' which is a reproduction of an ED triage space, has been created to simulate DAISY's operation in a controlled environment.
Sheffield Children's NHS Foundation Trust (UK): This trust has been piloting an AI tool developed by Alder Hey Innovation. The tool utilizes a range of markers, including those related to health inequalities, to predict and identify children most at risk of missing their appointments (a common issue known as "was not brought" in pediatric care). By focusing on addressing barriers such as forgotten reminders or lack of travel money, the pilot successfully reduced missed appointments from a benchmark rate of 19.27% to just under 6,500 patients annually. This initiative not only improves patient safety by ensuring care delivery but also frees up valuable appointment spaces for other patients in need.
King Faisal Specialist Hospital & Research Centre (KFSH&RC): A significant study at this institution utilized a dataset of 38,891 pediatric emergency records, which were meticulously cleaned to 18,237 records. Machine learning models were then developed to classify patient urgency into three groups: nonurgent, urgent, and emergency. The CatBoost model achieved an impressive 90% F-1 score and, critically, "never misclassified an urgent patient as nonurgent or vice versa". This demonstrates a high level of accuracy and safety in pediatric triage categorization.
Ann & Robert H. Lurie Children's Hospital of Chicago: A survey conducted here revealed that parents are generally receptive to the use of AI tools for managing children with respiratory illnesses in the ED (e.g., determining antibiotic need, interpreting radiographs). Perceived benefits included AI's ability to identify details a human might miss and provide a more rapid diagnosis. However, the study also found that certain demographic subgroups, such as non-Hispanic Black and younger parents, expressed greater reservations. This finding underscores the critical importance of involving a broad representation of parents and stakeholders from the earliest stages of AI system development for pediatric healthcare to ensure comfort and acceptance.
These concrete examples of AI prototypes and pilot programs in pediatric settings are particularly significant given that a very small percentage of AI models progress beyond the prototype phase. The observations regarding parental receptiveness, coupled with reservations among specific demographic subgroups, highlight that the transition from research to pilot implementation is not solely a technical hurdle. It also critically depends on stakeholder acceptance. This emphasizes the importance of involving a broad representation of parents and other stakeholders early in the development process to ensure that AI tools are designed with user comfort, cultural sensitivity, and equitable access in mind. Such engagement is crucial for successful integration into real-world clinical practice.
Conclusions
The analysis of pediatric-specific AI triage models reveals a compelling and urgent need for their widespread adoption, driven by the unique physiological and developmental characteristics of children that render conventional triage methods inherently limited. Children are not simply smaller versions of adults; their subtle symptom presentations, rapid decompensation, and specific physiological responses necessitate a specialized approach that traditional, subjective triage systems often fail to provide consistently. This inadequacy leads to quantifiable mistriage rates and compromised patient safety.
AI triage models, particularly those leveraging advanced machine learning algorithms like CatBoost, demonstrate a significant leap forward in accuracy and efficiency. They can process vast amounts of multi-modal data, including real-time vital signs and comprehensive EHR information, to categorize patients with high precision, dramatically reduce response times, and, crucially, minimize critical misclassifications. Beyond immediate triage, these systems offer transformative benefits in optimizing resource allocation, reducing clinician burnout, and enhancing diagnostic and predictive capabilities, shifting care towards a more proactive and personalized model.
However, the path to full implementation is fraught with challenges. The effectiveness and equity of AI models are fundamentally tied to the quality, diversity, and representativeness of their training data. Existing data gaps and biases, particularly concerning pediatric and socioeconomically diverse populations, pose significant ethical and practical hurdles that, if unaddressed, could exacerbate healthcare disparities. Furthermore, successful integration into clinical workflows hinges on fostering clinician trust and ensuring transparency in AI's decision-making processes, necessitating robust training and explainable AI tools. The current lack of comprehensive, child-centered ethical guidelines for AI in healthcare represents a critical vacuum that must be proactively filled to safeguard the rights and well-being of vulnerable pediatric patients.
In conclusion, pediatric-specific AI triage models hold immense promise to revolutionize emergency care for children, offering the potential for faster, more accurate, and more equitable interventions. Realizing this potential requires a concerted, multi-faceted effort: strategic investments in diverse data infrastructure, rigorous validation through multi-center prospective studies, a steadfast commitment to addressing and mitigating algorithmic biases, proactive development of child-centered ethical frameworks, and continuous education and collaborative engagement with healthcare professionals. Only through such comprehensive and ethically grounded approaches can AI truly serve as a powerful force for improving pediatric health outcomes.
FAQ Section
What is a pediatric-specific AI triage model?
A pediatric-specific AI triage model is an artificial intelligence system designed to prioritise and manage the treatment of pediatric patients in emergency settings based on their medical needs.
How does AI improve pediatric triage?
AI improves pediatric triage by analysing vast amounts of data quickly and accurately, identifying patterns and predicting outcomes to ensure that the most critical cases are attended to promptly.
What are the ethical considerations in using AI for pediatric triage?
Ethical considerations include ensuring data privacy, avoiding algorithm bias, and ensuring the AI system is transparent and accountable.
How can AI help in remote pediatric triage?
AI can facilitate remote pediatric triage through telemedicine, allowing healthcare providers to assess and monitor patients in rural or underserved areas.
What role does natural language processing play in AI triage?
Natural language processing (NLP) enables AI systems to understand and respond to natural language inputs, making the triage process more intuitive and user-friendly.
What are the benefits of integrating wearable devices with AI triage?
Integrating wearable devices with AI triage allows for real-time monitoring of vital signs and symptoms, providing a more comprehensive assessment of the patient's condition.
How does AI address communication barriers in pediatric triage?
AI can analyse non-verbal cues and integrate data from various sources to provide a more accurate assessment, even when younger children cannot articulate their symptoms clearly.
What regulatory challenges are associated with AI in pediatric triage?
Regulatory challenges include complying with data protection laws such as GDPR and HIPAA and ensuring the AI system meets healthcare standards and guidelines.
How does AI impact pediatric emergency department wait times?
AI can significantly reduce pediatric emergency department wait times by prioritising patients based on real-time data analysis and ensuring efficient resource allocation.
How can AI help in reducing misdiagnosis rates in pediatric triage?
AI can help reduce misdiagnosis rates by providing more accurate and consistent triage decisions and identifying patterns and anomalies that human providers might miss.
