Patient Pathways in the NHS: Navigating Care and Optimizing Services
Explore the intricacies of patient pathways in the NHS, from initial assessment to specialised care. Discover how streamlined processes and digital innovations enhance patient outcomes and transform healthcare delivery in the UK.


Patient pathways within the National Health Service (NHS) represent the structured sequence of care a patient receives, from initial symptom presentation through diagnosis, treatment, and follow-up. This report provides a comprehensive analysis of these pathways, distinguishing them from the specific NHS Pathways clinical triage tool, and examines their evolution, current state, and the critical role they play in healthcare delivery. It identifies significant challenges impeding optimal patient flow and outlines strategic approaches for service optimization.
Key Findings:
Structured Care Frameworks: Patient pathways are essential frameworks that standardize care, reduce unwarranted variation, and improve outcomes by guiding patients through sequential steps of their healthcare journey. This structured approach is a direct response to the inherent complexity of a large, multi-provider health system, serving as an intervention to ensure consistent, high-quality care.
Digital Transformation as a Core Enabler: Digital tools such as the NHS e-Referral Service (e-RS) and the Booking and Referral Standard (BaRS) are pivotal in modernizing referral processes, enhancing information sharing, and empowering patients with greater choice and control. These systems act as a central nervous system for referral flow, though their reliance on patient engagement necessitates careful consideration of digital equity.
Persistent Systemic and Operational Bottlenecks: The NHS grapples with multifaceted challenges, including chronic workforce shortages, underfunding leading to bed crises and backlogs, and operational inefficiencies such as fragmented assessments, diagnostic delays, and suboptimal patient flow. These issues are often interconnected, with short-term solutions sometimes proving unsustainable.
Patient-Centric Barriers: Beyond systemic issues, patients face significant non-clinical barriers, including transport difficulties, accessibility challenges, and communication gaps. These external factors can profoundly impede a patient's ability to navigate their care journey, highlighting the need for holistic solutions that address social determinants of health.
Proven Optimization Strategies: Successful pathway redesign initiatives across various clinical areas (e.g., cancer, diagnostics, acute and chronic disease management) demonstrate tangible benefits. These include improved clinical outcomes, reduced costs, shorter waiting times, and enhanced patient satisfaction, often achieved through multidisciplinary collaboration, data-driven management, and patient co-design.
Recommendations:
To achieve optimal patient pathways, the NHS must prioritize strategic workforce planning and investment, accelerate and deepen digital transformation with an equity lens, implement system-wide patient flow management, embed patient and public co-design into pathway development, and foster a culture of continuous quality improvement and learning. These integrated efforts are crucial for building a more resilient, efficient, and patient-centered healthcare system.
1. Introduction: Defining Patient Pathways in the NHS
1.1 Understanding "Patient Pathways" and their Purpose
The term 'patient pathway' within the NHS broadly describes the sequential steps and services involved in a patient's journey through the healthcare system. This encompasses the specific route an individual takes from the initial referral request or emergency activity through diagnosis, treatment, and subsequent follow-up. These pathways are not merely descriptive; they are structured frameworks designed to guide patients through their healthcare experience, from the first presentation of symptoms to appropriate treatment and eventual discharge.
The conceptualization of care pathways emerged in the 1990s as healthcare professionals and policymakers recognized the imperative for a more structured approach to patient care. The primary objective was to enhance the quality, efficiency, and consistency of care across diverse healthcare settings. The aim is to ensure that patients consistently receive the right care, at the right time, and in the right place. This structured approach is particularly vital in a complex adaptive system like the NHS, where achieving consistent, high-quality care without explicit guidelines can be challenging. The very existence of these structured pathways suggests a historical or inherent difficulty in maintaining uniform standards across a vast, multi-provider network, thus necessitating these frameworks as deliberate interventions to enforce best practice and standardize care.
The scope of patient pathways is extensive, covering a wide array of specialties and conditions, ranging from acute to long-term conditions, surgical procedures, and preventative care. For individuals managing chronic or recurrent conditions, a patient pathway is designed to continue even if the patient initially declines treatment, as they may require care for the same condition at a later date. This continuity underscores the long-term commitment to patient care inherent in pathway design.
Furthermore, these pathways serve as a foundational infrastructure for continuous improvement and innovation. They are crucial for measuring the quality and effectiveness of care, facilitating the implementation of changes, and enhancing patient safety. This dynamic aspect positions pathways not as static routes but as evolving frameworks that enable data collection, performance monitoring, and the adoption of new technologies and practices. By defining clear sequences, deviations or inefficiencies become measurable, allowing for targeted interventions and the integration of new clinical knowledge. This makes pathways a critical element in ongoing quality improvement cycles within the NHS.
1.2 Differentiating "Patient Pathways" from "NHS Pathways"
A common area of confusion, even among healthcare users, is the distinction between the broad concept of "patient pathways" and the specific tool known as "NHS Pathways". Understanding this differentiation is crucial for clear communication and effective navigation of NHS services.
Patient Pathways (Broad Concept): As previously established, this term refers to the overarching journey a patient undertakes through the healthcare system for a specific health condition or need. It encompasses all stages, from the patient's initial contact with a healthcare provider, through diagnosis, various treatments, and subsequent follow-up care, often involving transitions between multiple services and care settings. This is the conceptual "journey of care" that guides the patient's entire experience.
NHS Pathways (Specific Clinical Tool): In contrast, NHS Pathways is a distinct clinical decision support system (CDSS) specifically designed for assessing, triaging, and directing the public to urgent and emergency care services. It supports the remote assessment of callers to services such as NHS 111, 999, Integrated Urgent Care Clinical Assessment Services, and NHS 111 Online. The system also plays a role in managing patients who present directly to urgent care or emergency departments.
The primary distinction lies in their scope and nature. While "NHS Pathways" is a particular software system used for initial triage and direction within urgent care, "patient pathways" is a broader conceptual term describing the entire, often complex, "journey of care" a patient undertakes across the NHS system. The former is a component or a tool that may initiate or direct a patient onto a broader patient pathway, particularly in urgent care scenarios.
The specific focus of "NHS Pathways" on urgent and emergency care highlights the critical role of initial access points in managing overall patient flow. Its function as a clinical decision support system indicates a strategic attempt to standardize and optimize the entry point into the healthcare system, aiming to direct patients to the most appropriate service from the outset. This suggests that the "front door" of the NHS, particularly urgent and emergency care, is recognized as an area of high demand and potential for misdirection. An efficient and accurate initial triage is paramount to prevent downstream bottlenecks and ensure appropriate resource allocation, as misdirection at this initial contact can lead to inefficiencies and potential harm later in a patient's journey.
The public's confusion between the general term "patient pathway" and the specific tool "NHS Pathways" underscores a significant communication gap. This lack of clarity can impede patient understanding, engagement, and their ability to effectively navigate their own care, despite efforts to promote patient choice. If patients do not comprehend the terminology used to describe their care journey, their capacity to make informed choices or participate meaningfully in co-design initiatives may be limited. This highlights a need for the NHS to translate its internal operational language into more accessible, patient-friendly terms, which can in turn improve patient satisfaction and adherence to care plans.
1.3 The Evolution and Importance of Structured Care Journeys
The adoption of care pathways within the NHS can be traced back to the 1990s, driven by a growing recognition of the need for a more structured approach to patient care. The initial impetus was to enhance the quality, efficiency, and consistency of care delivery across various healthcare settings. The term "pathway" was adopted as a fitting metaphor, depicting the sequential steps or stages involved in delivering care, akin to following a predefined route.
The implementation of care pathways has been propelled by several factors, including the imperative for quality improvement, the optimization of resources, and the enhancement of patient experiences. These structured approaches are designed to ensure that patients receive the right care at the right time, which demonstrably leads to improved patient outcomes and a better patient experience. Evidence suggests that clinical pathways are associated with a reduction in in-hospital complications and improved documentation, contributing to safer and more effective care.
Furthermore, pathways contribute significantly to increased efficiency and reduced costs. By minimizing the duplication of services and fostering improved communication among different healthcare professionals, pathways facilitate a more efficient utilization of resources and can lead to overall cost reductions. Studies have consistently reported significant reductions in the length of hospital stays and associated costs where pathways are effectively implemented.
Beyond efficiency, pathways are vital tools for evaluation and innovation. They provide a framework for measuring the quality and effectiveness of care, enabling necessary changes and continuous improvements. They are also indispensable for designing, testing, evaluating, and implementing new technologies and innovations in healthcare, as well as for conducting research activities. This capacity for measurement and adaptation positions pathways as dynamic instruments for systemic learning and evolution.
Finally, pathways promote standardization by providing a consistent set of processes or management guidelines. This fosters shared documentation and ensures consistent care delivery across the system. The historical context of pathways emerging in the 1990s to address issues of quality, efficiency, and consistency suggests that the NHS, as it expanded, faced growing challenges in standardizing care across its vast and diverse network. Pathways, therefore, serve as a fundamental tool for managing complexity and reducing unwarranted variation in clinical practice, ensuring a common, evidence-based standard across the system.
While pathways aim to standardize care, their development through close collaboration among healthcare professionals and reliance on expert consensus indicates a delicate balance between imposing guidelines and respecting clinical autonomy. Successful pathway implementation requires significant buy-in from clinicians, which is often achieved through their active involvement in the design and continuous adaptation of these frameworks. This collaborative approach ensures that pathways are not merely top-down mandates but are practical, clinically relevant, and supported by those who deliver care. This highlights the socio-technical aspect of pathway implementation, where human factors are as crucial as the technical design.
The Patient Journey: Stages, Processes, and Digital Enablers
2.1 Overview of the Typical Patient Journey (Referral to Follow-up)
The patient journey within the NHS typically commences with an individual presenting with symptoms, often leading to an initial consultation with a General Practitioner (GP). If specialist care is deemed necessary, the GP initiates a referral.In urgent or emergency scenarios, the journey might begin with contact via services like NHS 111 or 999, where the specific "NHS Pathways" clinical tool is employed for initial assessment and direction to the most appropriate urgent care service.
Following a referral, patients frequently enter a period of waiting. This can involve waiting for a new outpatient appointment (designated as Stage 1 in pathway tracking) or waiting for a diagnostic test, an Allied Health Professional (AHP) intervention, or the results thereof (Stage 2). This diagnostic phase is a critical juncture for establishing an accurate diagnosis and determining the most suitable treatment trajectory. The detailed breakdown of the "Stage of Pathway" heavily emphasizes these "waiting" periods, highlighting that waiting is not merely an unfortunate side effect but a formally defined stage within the patient journey. This perspective is crucial for identifying bottlenecks and understanding the patient experience, as prolonged waiting directly impacts patient satisfaction and can potentially influence clinical outcomes. Therefore, any effort to optimize pathways must directly address these "waiting" stages as active areas for intervention.
Once a diagnosis is established, a comprehensive treatment plan is developed and implemented. This involves delivering appropriate treatment tailored to the patient's condition. For complex conditions, such as cancer, the pathway encompasses detailed clinical investigations, patient diagnosis, and subsequent treatment, with clinicians carefully considering the most suitable treatment options, their sequence, and the optimal location for delivery.
The journey then progresses through follow-up appointments (Stage 3) or periods of waiting for clinical decisions.Ultimately, the patient reaches a point of discharge from active treatment. However, for individuals with chronic or recurrent conditions, the patient pathway is understood to continue even after initial treatment completion, acknowledging the ongoing nature of their care needs. The discharge process itself is a critical component of effective patient flow, requiring careful management to ensure smooth transitions and prevent delays.
While pathways are often described as sequential steps , clinical practice frequently introduces variations, meaning that patients do not always progress linearly from one stage to the next. This inherent non-linearity and adaptability are necessary to accommodate individual patient needs and evolving clinical knowledge, rather than adhering to rigid, one-size-fits-all routes. This flexibility, while essential for delivering high-quality, personalized care, adds a layer of complexity to system-wide optimization efforts, as it makes "perfect" flow harder to achieve and measure consistently. Consequently, data collection and analysis must account for these variations to accurately assess pathway performance and identify areas for improvement.
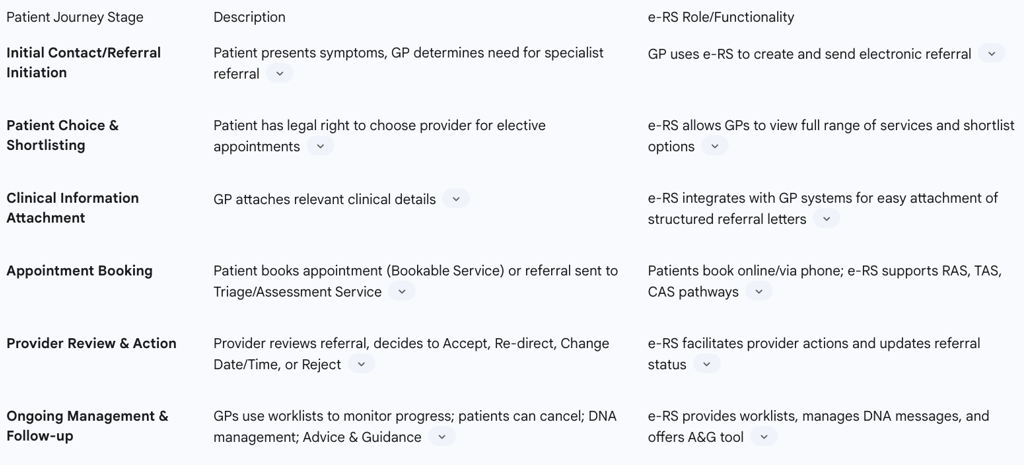
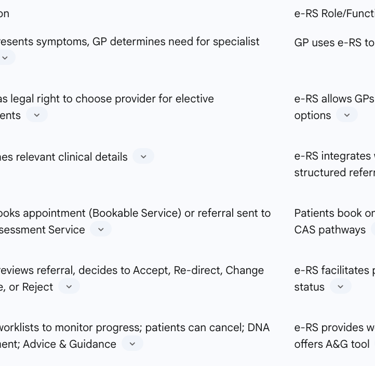
2.2 The Role of the NHS e-Referral Service (e-RS) in Streamlining Access
The NHS e-Referral Service (e-RS) serves as a pivotal electronic referral-support tool, specifically designed to streamline the referral process for patients requiring onward care within the NHS. Its overarching objectives are to enhance efficiency, improve clinical communication, and empower patients by providing them with greater choice, certainty, and control over their healthcare journey.
The patient's engagement with e-RS typically commences when a GP determines the need for specialist referral. The GP utilizes the e-RS professional application to create and dispatch an electronic referral, which can be directed to consultant-led outpatient clinics or other services such as community, diagnostic, assessment, and GPwSI (GP with Special Interest) services. A significant feature for elective (non-emergency) consultant-led appointments is the patient's legal right to choose their provider. e-RS is the sole platform enabling GPs to view the comprehensive range of available consultant-led outpatient services across England, facilitating the shortlisting of options based on factors such as location, date, and time.
Crucially, relevant clinical referral information, such as a referral letter or pro-forma, is securely attached to the electronic referral within e-RS. The system integrates with accredited GP Clinical systems, allowing for the seamless conversion and electronic attachment of clinical information from the patient's GP record, ensuring data security and full auditability.
For "bookable services," a key procedural step is that the patient must book an appointment before the clinical referral information becomes visible to the provider. Patients are provided with clear instructions on how to select a clinic and schedule their appointment, typically through a printed letter, with future enhancements aiming for electronic instructions. Patients can book their appointments online via the 'Manage Your Referral' website or by contacting a national telephone booking service. This patient-led booking mechanism has been shown to contribute to a reduction in hospital Did Not Attend (DNA) rates.
Alternatively, e-RS supports "triage/assessment service" pathways, where the referral information is assessed first, without a pre-booked appointment. These include Referral Assessment Services (RAS), Telephone Assessment Services (TAS), and Clinical Assessment Services (CAS). These services review the clinical information to determine the most appropriate onward pathway or provide advice back to the referring clinician.
Upon a referral to a bookable service and the patient's appointment booking, the provider clinician reviews the referral information promptly to ascertain if the patient has been booked into the correct service with appropriate urgency. The provider can then choose to:
Accept (the usual outcome if clinically appropriate); Re-direct (to a more suitable alternative service within e-RS, with the patient re-booked by the provider); Change Date/Time (adjusting appointment details); or Reject (if alternative management is clinically more effective without a face-to-face appointment, returning the referral to the GP's worklist for action).
GPs and their practice teams actively manage four worklists within the e-RS application. These worklists serve as a central mailbox, enabling them to monitor referral progress, check outstanding actions, and view responses to advice and guidance queries. This system also addresses Appointment Slot Issues (ASIs), where, if no appointments are available, the referral can still be sent, appearing on a provider worklist for direct patient contact and booking. Patients are responsible for following booking instructions and can cancel their referrals via e-RS, which informs their referring practice. Providers manage missed appointments by re-booking patients or cancelling the referral with a recorded reason.
Clinical responsibility within e-RS generally mirrors that of traditional paper referrals. The referring organization is accountable for the decision to refer, service selection, clinical information, and appointment booking. The provider organization is responsible for assessing referral information, redirection, arranging appointments for RAS and deferred referrals, and managing cancelled referrals. The Advice and Guidance (A&G) tool within e-RS further facilitates multi-way conversations between GPs and consultants, strengthening professional relationships and fostering knowledge sharing.
While e-RS aims to empower patients with choice and control , it also shifts significant responsibility onto them for booking and managing appointments. The requirement that patients must book an appointment before clinical referral information is visible to the provider, coupled with reminder letters for unbooked appointments, suggests that digital empowerment necessitates active patient engagement and digital literacy. This approach could inadvertently create new barriers for digitally excluded or less engaged patients, potentially impacting equitable access to care.
The comprehensive functionality of e-RS, from GP initiation and patient choice to provider action, worklist management, and the A&G tool, positions it as a critical digital backbone for managing referral flow across the NHS. Its capacity to integrate with GP systems and provide auditable information indicates that it is not merely a booking tool but a vital component for data-driven management and accountability within the referral process. This makes e-RS akin to a central nervous system for referral flow, crucial for identifying and addressing bottlenecks at a macro level.
Table 2: Stages of the NHS Patient Journey and e-RS Functionality
2.3 Interoperability and Information Sharing: The Booking and Referral Standard (BaRS)
The Booking and Referral Standard (BaRS) represents a significant advancement in the NHS's digital strategy, serving as an interoperability standard designed to enable seamless digital patient journeys and operational processes for patients, healthcare workers, and carers. The core function of BaRS is to ensure that relevant information is shared quickly, safely, and in a useful format across different care providers.
BaRS is fundamentally about fostering seamless information flow. It is designed to ensure that booking, clinical, and administrative information consistently follows the patient at all stages of their journey. By adopting a common interoperability standard, the process of moving patients through their care journey becomes easier, faster, and safer. This directly addresses a core challenge identified in patient flow: fragmented assessment, where patients often have to see multiple teams and repeatedly provide the same information. BaRS is a strategic attempt to create a unified digital thread through the patient journey, ensuring that information collected earlier is accessible and prevents unnecessary repetition.
The standard is being strategically deployed at key interfaces within the urgent and emergency care system, specifically between NHS 111 and emergency departments, and between 999 and Clinical Assessment Services, with a target implementation by March 2025. This standardization significantly benefits healthcare workers by enabling them to receive the necessary information in sufficient detail to undertake patient care activities effectively. It also allows them to triage patients without requiring them to unnecessarily repeat information already collected earlier in their journey, thereby integrating booking and referral data into existing healthcare IT systems, avoiding the need to work across multiple applications, and ultimately saving time.
Patients also derive substantial benefits from BaRS, including the ability to efficiently book appointments and time slots with the most appropriate service, and to receive the right advice and treatment when most needed, safely and easily.BaRS is not a standalone solution but connects with other crucial digital services, including the NHS App, NHS e-Referral Service (e-RS), NHS 111 Online, and GP Connect. These interconnected services collectively aim to provide secure access to a wide range of NHS services and patient records, further enhancing the digital patient experience.
The listing of BaRS alongside other key digital services such as the NHS App, e-RS, NHS 111 Online, and GP Connect indicates a broader vision for a fully integrated digital ecosystem within the NHS. This suggests a strategic move towards a future where patient information is fluidly accessible across all touchpoints, enabling truly coordinated and patient-centric care. This ambition extends beyond just referrals, with the potential to unlock further efficiencies and improve the overall quality and safety of care by providing a holistic view of the patient and reducing administrative burdens across the entire healthcare continuum.
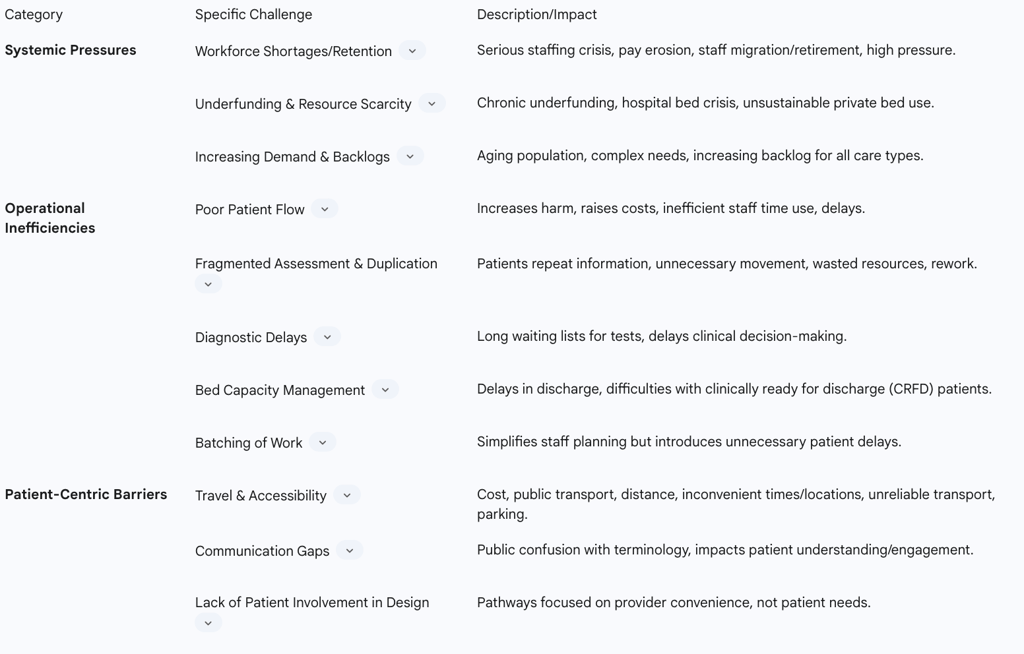
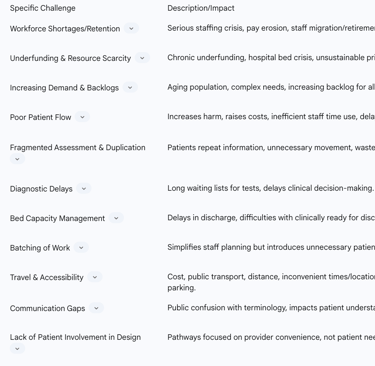
3. Challenges and Bottlenecks in NHS Patient Pathways
Despite significant advancements in pathway design and digital integration, the NHS continues to face substantial challenges and bottlenecks that impede optimal patient flow and service delivery. These issues can be broadly categorized into systemic pressures, operational inefficiencies, and patient-centric barriers.
3.1 Systemic Pressures: Staffing, Funding, and Backlogs
The NHS is currently navigating immense systemic pressures, primarily stemming from chronic workforce shortages, persistent underfunding, and a burgeoning backlog of care. The health service faces a serious staffing crisis, a consequence of years of poor workforce planning, weak policies, and fragmented responsibilities. This crisis is exacerbated by issues such as staffing retention difficulties, erosion of pay, and unfavorable pension policies, which collectively contribute to the migration of staff overseas or early retirement. Even with increased medical school placements, new graduates often face immense pressure during training, which can lead them to seek opportunities abroad or take gap years, further compounding the workforce deficit.
Underfunding over the past decade, intensified by current inflation, has significantly contributed to the prevailing challenges. This financial constraint manifests as a pervasive lack of resources and a critical hospital bed crisis. The reliance on costly private beds, averaging £680 per day, to create additional capacity is a clear indicator of this resource scarcity and is recognized as an unsustainable measure. These financial and resource limitations have led to significant failings for patients and service providers across the system.
The combined effect of an aging population and an increasing number of patients with complex health needs places immense and growing demand on NHS services. This escalating demand, coupled with resource limitations, has resulted in a substantial and increasing backlog of care and appointments, causing significant delays in providing care, even for emergency cases and serious illnesses like cancer.
The interconnectedness of these systemic challenges is evident: chronic underfunding and inadequate workforce planning directly contribute to staff shortages and diminished morale, which in turn exacerbate care backlogs and delay patient treatment. This pattern indicates that addressing patient pathway bottlenecks cannot be achieved solely through process optimization; it necessitates fundamental, strategic investments in workforce development and infrastructure. Furthermore, the reliance on expensive, short-term solutions, such as using private beds to alleviate immediate capacity issues, highlights a broader pattern of reactive measures in the face of chronic underinvestment. While these provide temporary relief, they are unsustainable and divert funds that could otherwise be allocated to more enduring improvements, such as digital transformation or long-term workforce development, thereby hindering genuine pathway optimization and financial sustainability in the long run.
3.2 Operational Inefficiencies: Patient Flow, Bed Capacity, and Diagnostic Delays
Operational inefficiencies within the NHS significantly contribute to bottlenecks in patient pathways. Poor patient flow, a pervasive issue, increases the likelihood of harm to patients and inflates healthcare costs by preventing the optimal utilization of skilled staff time. When patients do not move through the system appropriately, delays become inevitable, impacting the quality and timeliness of care.
A common operational challenge is fragmented assessment and duplication of effort. Patients often experience a disjointed journey, requiring them to interact with multiple teams sequentially, frequently repeating information already provided. This leads to unnecessary movement and delays within the system. There is often a duplication of services and considerable waste, including unnecessary waiting and redundant checks.
Diagnostic delays represent a critical bottleneck within the patient journey, leading to extended waiting lists. Examples include a 19-week wait for a barium enema and an average of 22 days for cervical screening results. A lack of timely access to diagnostics can significantly impede clinical decision-making, further prolonging the pathway.
Effective bed capacity management has become an increasingly prominent concern. Delays in patient discharge, even for those who are clinically ready for discharge (CRFD), can cause significant disruptions to patient flow throughout hospitals. The broader hospital bed crisis directly impacts patient flow and overall outcomes. Dedicated Patient Flow teams are tasked with managing bed availability and proactively addressing issues related to CRFD patients to resolve delays swiftly.
Another operational inefficiency stems from the practice of "batching" work. While grouping similar tasks together may simplify planning for individual clinical staff, it often introduces unnecessary delays for patients across the system.Examples include weekly note and letter writing or scheduling all discharges for Fridays, which can lead to extended patient waits. This highlights a fundamental tension between optimizing local departmental productivity and achieving optimal system-wide patient flow. A siloed approach to efficiency can inadvertently create bottlenecks elsewhere in the pathway, meaning that true patient pathway optimization requires a holistic, system-level perspective rather than isolated departmental improvements.
Beyond direct financial costs, these operational inefficiencies carry a significant "hidden" cost. Fragmented assessments, diagnostic delays, and poor patient flow result in extensive rework, unnecessary patient movements, wasted resources, and increased staff time spent on administrative tasks rather than direct patient care. This not only raises healthcare costs by failing to maximize skilled staff time but also contributes to staff morale issues, burnout, and reduced overall capacity, profoundly impacting the quality and sustainability of service delivery.
3.3 Patient-Centric Barriers: Accessibility, Transport, and Communication Gaps
Even when systemic and operational issues are addressed, patients often encounter significant barriers related to their personal circumstances, which can severely impede their ability to navigate NHS pathways effectively.
Travel and accessibility issues are a major concern. Patients frequently report difficulties related to the cost of travel, problems with public transport availability, and the sheer distance to their appointments. Inconvenient appointment times and locations, unreliable or limited transport options, and the availability and cost of parking at healthcare facilities are frequently cited as major concerns. Specific examples include patients waiting over 13 hours for patient transport or facing parking costs of £18 for a 9-hour stay. This extensive list of travel and accessibility issues reveals that factors outside the direct clinical pathway significantly impede patient access and engagement. This indicates that pathway optimization cannot solely focus on clinical processes; it must also consider and address broader social determinants of health that impact a patient's ability to complete their journey. If a patient cannot physically get to an appointment, the most efficiently designed clinical pathway becomes ineffective.
Communication gaps also pose a considerable challenge. The public's confusion regarding healthcare terminology, such as the distinction between "patient pathway" and "NHS Pathways," highlights existing communication deficits. The need for co-developed healthcare communications, where language aligns with the audience's understanding, is crucial. While digital tools like e-RS aim to improve communication , the responsibility placed on patients to book appointments and follow up on rejected referrals means that clear and effective communication of these responsibilities is vital for successful pathway progression.
Furthermore, a lack of meaningful patient involvement in pathway design can lead to services that are primarily "focused around provider, rather than patient, convenience". This can result in pathways that do not fully align with patient needs, preferences, or lived experiences, potentially reducing their effectiveness and acceptability.
While digital tools like e-RS and BaRS are designed to streamline processes , the increasing reliance on patients to book appointments online and the broader push for digitalization within the NHS could inadvertently exacerbate health inequalities. This is particularly true for individuals with limited digital access or literacy. This suggests a critical need for parallel non-digital support channels and inclusive design to ensure equitable access to care for all patient demographics. If a significant portion of the population lacks reliable internet access, devices, or digital skills, these "optimizations" can become new barriers to accessing necessary healthcare services.
Table 3: Summary of Major Challenges and Bottlenecks in NHS Patient Pathways
Strategies for Optimizing Patient Pathways and Services
Optimizing patient pathways within the NHS requires a multi-pronged approach that addresses systemic, operational, and patient-centric challenges. Effective strategies draw upon established principles of flow management, leverage digital advancements, foster collaborative approaches, and adhere to guiding policy frameworks.
4.1 Principles of Patient Flow Management and Pathway Redesign
Effective patient flow management is central to optimizing pathways. Strategies often involve implementing structured approaches, such as 'Lean' methodologies, to reduce variation in processes. For instance, Lean processes were successfully applied in cervical screening services, significantly reducing turnaround times and errors.
A critical component of effective flow is management based on real-time data and the meticulous matching of demand with available capacity, including workforce adjustments. This ensures the timely availability of senior staff, adequate access to diagnostics, and sufficient hospital beds. A fundamental operational principle is that improvements before a bottleneck are likely to result in increased waiting just before the bottleneck, while improvements directly at the bottleneck should result in increased throughput. This highlights that pathway optimization is not about improving every step equally but strategically targeting the most restrictive points to maximize system-wide flow. This necessitates sophisticated diagnostic work to accurately identify true bottlenecks before implementing solutions, as otherwise efforts might be wasted or even counterproductive.
Proactive discharge planning is another crucial, though often overlooked, aspect of patient flow. Identifying potential barriers to discharge upon admission and swiftly resolving issues for patients who are clinically ready for discharge is essential. This signifies a shift from reactive bed management to a more predictive and preventative approach to patient flow. By planning for discharge at the point of admission, the system aims to anticipate and mitigate potential issues, thereby improving overall bed turnover and reducing costly delays.
Addressing flow issues effectively requires a system-wide perspective, extending beyond individual departments to encompass processes across an entire hospital or a wider system, including primary care, ambulance services, social care, and community services. This holistic view helps to avoid merely shifting bottlenecks from one area to another. Strategies also focus on reducing unnecessary delays and the practice of batching work. This involves re-organizing work processes, minimizing paperwork, ensuring frequent decision-making, and reducing batch sizes. It can also entail reducing the number of steps within a pathway to streamline the patient's journey.
Finally, extensive staff engagement and comprehensive training are paramount for the successful implementation of redesign initiatives, as new processes require time to embed effectively within the organizational culture.
4.2 Leveraging Digital Technology and Data for Enhanced Efficiency
Digital technology and data analytics are increasingly recognized as indispensable tools for enhancing efficiency and optimizing patient pathways. Modern software solutions are essential, moving beyond temporary fixes like spreadsheets, which were once the best available option but are now outdated. These advanced programs provide live updates and role-based access to patient notes, making patient monitoring and information management significantly easier.
Access to real-time data is a key requirement for improving patient flow. This involves analyzing routinely collected data on service usage, undertaking capacity and workflow planning, and employing sophisticated methods such as simulation, modelling, and queuing theory. Advanced analytics can pinpoint key drivers of variation within pathways, enabling targeted interventions. The repeated emphasis on real-time data, data analysis, and software solutions indicates that data has evolved from a mere record-keeping necessity into a critical operational asset for understanding, predicting, and optimizing patient flow. This signifies a fundamental shift towards a data-driven decision-making culture within the NHS.
Electronic work management systems enable smarter organization and reduce the time staff spend chasing or updating information, allowing them to plan and coordinate patient care more easily. Interoperability standards, such as the Booking and Referral Standard (BaRS), ensure that booking, clinical, and administrative information consistently follows the patient throughout their journey, making patient movement through the care pathway easier, faster, and safer.
Beyond improving patient flow, digital tools that reduce unnecessary repetition of information and save staff time indirectly address the systemic challenge of workforce capacity. By automating administrative tasks and improving access to information, digital technology can free up skilled staff to focus on direct patient care, thereby enhancing productivity and potentially improving staff morale. This establishes a crucial link between digital investment and workforce optimization, especially pertinent in a context of staff shortages.
Innovative technology can also actively engage patients in their care journey , potentially through platforms like the NHS App, which allows for managing appointments and accessing health records.
4.3 Collaborative and Multidisciplinary Approaches to Care Coordination
Effective patient pathway optimization heavily relies on collaborative and multidisciplinary approaches to care coordination. Forming interdisciplinary teams is crucial for driving quality improvements in patient flow. Clinical pathways are typically developed through close collaboration between healthcare professionals who refer or request care and those who provide specialist advice and patient reviews, ensuring that pathways reflect collective expertise.
Addressing complex flow issues often requires cross-organizational collaboration, necessitating an exploration of processes across an entire hospital or a wider system that includes primary care, ambulance services, social care, and community services. Successful examples include integrated respiratory services that involve seamless working between hospital, community, and primary care providers. This repeated call for cross-organizational collaboration and the documented success of integrated services indicate a fundamental shift from a departmental or organizational siloed approach to a networked, system-wide model of care delivery. This suggests that many current bottlenecks stem from a lack of coordination between different parts of the NHS and social care, making inter-agency collaboration a prerequisite for significant pathway optimization.
The involvement of patients and carers, through co-design, is increasingly prevalent and highly effective in service and pathway design. Their perspectives should be actively sought during the preparation phase for flow improvements. This ensures that terminology and language are aligned with the audience's understanding and that services are genuinely patient-centered. Beyond simply improving patient experience, involving patients in pathway design serves as a critical quality assurance mechanism. Patients can identify unwarranted variation and provide unique insights into the root causes of problems from a lived experience perspective that professionals might overlook. This indicates that patient involvement is not merely a beneficial addition but a strategic imperative for designing effective, equitable, and acceptable services.
Pathway redesign also offers opportunities to maximize effective shared decision-making between patients and clinicians.Furthermore, tools like the Advice and Guidance (A&G) feature within e-RS facilitate multi-way conversations between GPs and consultants, strengthening professional relationships and fostering knowledge sharing across the system.
4.4 Guiding Frameworks and Policies for Pathway Improvement
The optimization of patient pathways within the NHS is guided by a robust set of frameworks and policies that ensure adherence to best practices and continuous improvement.
National Institute for Health and Care Excellence (NICE) guidelines provide evidence-based recommendations for health and care across England. These guidelines are integral to the clinical care provided by healthcare professionals, outlining the appropriate care and services for most people with specific conditions or needs. Their integration with other frameworks, such as the Patient Experience Improvement Framework, highlights a dual mandate for pathway design: it must be clinically effective and patient-centric. This implies that "optimization" encompasses not only efficiency but also adherence to best practice and the delivery of a positive patient experience.
The Patient Experience Improvement Framework itself recommends implementation using quality improvement methodologies and embracing the principle of continual learning. This framework supports self-assessment and organizational diagnostics to embed patient experience within leadership, culture, and operational processes.
Business Process Re-engineering (BPRE) offers a valuable framework for transformative process change, aiming to enhance "consumer experience" and efficiency. This approach can be effectively complemented by experience-based co-design, ensuring that operational changes are informed by patient perspectives.
A structured approach to pathway design and implementation is further supported by toolkits that outline key components such as identifying client populations, assembling interdisciplinary quality improvement teams, researching evidence-based guidelines, mapping current service provision, developing revised protocols, rigorous testing (e.g., Plan-Do-Study-Act cycles), and continuous monitoring after implementation. This methodology emphasizes measurement-based care anchored in evidence-based and best practices.
Finally, the role of leadership and organizational culture is paramount. Visible and accessible leadership sets the tone for staff, fostering an environment conducive to improvement. Organizations where boards regularly hear patient stories and executives champion a positive learning culture demonstrate momentum for quality, patient experience, and safety. An open and transparent organizational culture has a profoundly positive impact on both staff and patients. This emphasis on leadership, culture, and staff engagement as critical factors for successful implementation indicates that even the most meticulously designed pathways and advanced digital tools may falter without the right organizational environment. "Soft" factors like leadership commitment and an open learning culture are as important as "hard" factors like technology and process maps in driving sustainable change.
5. Impact and Outcomes of Optimized Pathways
The strategic implementation of optimized patient pathways yields significant benefits across multiple dimensions, including clinical outcomes, operational efficiency, and patient experience.
5.1 Improving Clinical Outcomes and Patient Safety
Optimized clinical pathways are consistently associated with improved clinical outcomes and enhanced patient safety. Evidence demonstrates a reduction in in-hospital complications and errors. Studies have frequently reported a positive effect on overall clinical outcomes, ensuring that patients receive the right care at the right time. This consistent finding directly links pathways to the effective translation of evidence-based practice into routine care. Pathways serve as a crucial bridge between clinical research and real-world patient benefits, ensuring that best practices are systematically applied at the point of care, thereby improving the quality and safety of healthcare delivered.
Furthermore, pathways lead to improved documentation of treatment goals and communication among patients, carers, and healthcare professionals. This enhanced documentation fosters greater accountability and ensures continuity of care, reducing the likelihood of oversights or miscommunications.
Beyond managing existing conditions, optimized pathways contribute significantly to prevention and early diagnosis. For example, the nationwide stroke prevention initiative in Atrial Fibrillation (AF) utilized the GRASP-AF tool in primary care. This led to a substantial increase in the percentage of at-risk patients prescribed anticoagulants, resulting in significant opportunities for stroke reduction. Similarly, promoting the use of simple blood tests (serum natriuretic peptide or NP) in primary care for the early diagnosis of heart failure has reduced acute admissions and minimized unnecessary investigations, thereby preventing disease progression and reducing the burden of more costly, downstream interventions.This signifies a strategic shift towards more proactive and preventative models of care within the NHS, aligning with long-term goals of sustainability and population health.
5.2 Enhancing Efficiency, Reducing Costs, and Shortening Waiting Times
A primary objective of pathway optimization is to enhance efficiency, reduce healthcare costs, and shorten patient waiting times. Optimized pathways are strongly associated with significant reductions in the length of hospital stay (LOS). For instance, breast surgery pathways successfully reduced the mean LOS from 2.4 days to 1.4 days.
These efficiency gains translate directly into substantial cost savings. Studies report a positive effect on reducing overall healthcare costs. Specific examples include a 27% reduction in costs per patient for post-operative head and neck surgery, potential savings of £7.89 million from reduced breast surgery bed days, and annual savings of £30,000 in dermatology due to faster histopathology results.
Optimization efforts consistently lead to shorter waiting times for patients. Notable improvements include reducing barium enema waiting times from 19 weeks to 2 weeks, decreasing cervical screening results turnaround from an average of 22 days to within 14 days (with 95% delivered within 7 days), and cutting tinnitus service waiting times from 28 weeks to less than 4 weeks.
Improved patient flow enhances throughput and continuity of care. By streamlining processes and eliminating waste, departments can maximize the number of patients treated within existing resources. For example, cardiac surgery pathway redesign at St George’s Healthcare NHS Trust led to an increased activity valued at £103,000 due to improved productivity.
Pathways also contribute to more efficient resource utilization by reducing the duplication of services and improving communication, leading to a more effective use of resources. This includes better bed utilization and a reduction in staff time spent on administrative tasks, allowing them to focus more on direct patient care. The data consistently demonstrates that reducing length of stay often correlates with reduced costs and increased throughput. This highlights that these efficiency metrics are not isolated but are deeply interconnected, where improving one often has a cascading positive effect on others, reinforcing the value of holistic pathway optimization. Furthermore, the documented cost savings, such as the £85,000-£100,000 annual return on a £30,000 investment for cervical screening improvements , illustrate a clear return on investment for pathway redesign and digital solutions. This indicates that initial investments in process analysis, technology, and staff training are not merely expenses but strategic capital expenditures that yield significant financial and operational benefits over time, thereby justifying further investment.
5.3 Boosting Patient Experience and Satisfaction
Beyond clinical and operational metrics, a crucial outcome of optimized pathways is a significant boost in patient experience and satisfaction. Good experience is now recognized as an essential component of excellent health and social care, on par with clinical effectiveness and safety. Care pathways are explicitly designed with the aim of enhancing patient experiences.
Studies consistently report a positive effect on patient satisfaction. Specific examples include 100% positive feedback for cancer survivorship courses, patients reporting an early psychological boost from same-day discharge after breast surgery, and increased satisfaction with audiology services. This emphasis on patient experience as "essential" and its positive correlation with satisfaction suggests that patient perception is a critical quality indicator, not merely a subjective outcome. Moreover, positive experiences, coupled with greater choice and control, can drive enhanced patient engagement and adherence, which in turn contributes to improved clinical outcomes.
Patients gain greater control and choice over their care. They have a legal right to choose where they receive NHS treatment , and digital tools like e-RS provide choice, certainty, and control over their healthcare journey, enabling them to book appointments that suit their needs, which has been shown to reduce DNA rates.
Improved communication and the provision of clear information are also key benefits. Patients receive the right advice and treatment when they most need it, safely and easily. Enhanced coordination and the provision of comprehensive treatment summaries and care plans further improve communication and patient understanding.
The psychological impact of efficient pathways is also noteworthy. Eliminating unnecessary waits and procedures demonstrably reduces patient anxiety. Faster, more predictable diagnostic results contribute significantly to improved patient experience by alleviating stress and uncertainty. The mention of an "early psychological boost" and reduced patient anxiety highlights the significant psychological impact of efficient pathways. This indicates that optimizing pathways extends beyond purely logistical improvements; it directly contributes to patients' mental well-being and sense of control during a vulnerable time, reinforcing the "caring" aspect of NHS services and underscoring that a well-designed pathway contributes to holistic patient well-being, not just clinical recovery.
Finally, embedding patient-centered design, through the active involvement of patients, families, and carers in shaping services, ensures that their experiences are at the heart of service redesign. This leads to the development of more personalized and holistic care models.
6. Case Studies: Successful Pathway Redesign Initiatives
This section presents specific examples of successful patient pathway redesign projects within the NHS, illustrating the practical application of optimization strategies and their tangible benefits across diverse clinical areas.
6.1 Innovations in Cancer Care Pathways
Helping Youngsters Cope with Cancer (Children and Young People - CYP Survivorship): The challenge identified was the increasing unviability and inappropriateness of long-term hospital-based follow-up for the exponentially growing population of childhood cancer survivors. The redesign involved developing national, safe, risk-stratified pathways. These new pathways emphasize patient choice, individualized care, the provision of treatment summaries and care plans, risk stratification, coordinated care, automated surveillance/remote monitoring, and robust primary care support. The benefits realized include ensuring high-quality, individualized care for all child and young person cancer survivors, irrespective of their treatment location or time. It empowers survivors with relevant, sufficient, and timely information, leading to 100% patient satisfaction with associated courses and motivating further learning. The initiative aims to achieve a 20% reduction in hospital-based outpatient appointments for CYP cancer survivors and ensure that 100% of survivors receive a treatment summary and care plan, directly addressing the complex physical, social, educational, and transitional challenges faced by young cancer survivors.
Transforming Inpatient Care (Breast Surgery Pathway): This initiative addressed lengthy inpatient stays for breast surgery, variations in clinical practice, and unnecessary waits and procedures that caused significant patient anxiety. The redesign applied 'Quality Winning Principles' to streamline the breast surgery pathway, focusing on enabling day case or one-night stays for major breast surgery without reconstruction. This involved a comprehensive review of clinical procedures, integration of pathways between acute hospitals and community services, and a willingness to challenge established preconceptions. The benefits were substantial: the mean length of stay for mastectomies and wide local excisions (without reconstruction) was reduced from 2.4 days (2006/7) to 1.4 days (2010/11 provisional). This achieved a 30% reduction in bed days from the 2006/7 baseline, with a potential saving of £7.89 million if released locally, without a significant increase in readmissions. Over 2,000 patients positively evaluated the improved experience, many reporting an early psychological boost from same-day discharge and stating they would choose this approach again. The project eliminated unnecessary waits and procedures, reducing patient anxiety, increasing efficiency, and optimizing bed utilization. This pathway has been acknowledged as best practice by NHS Evidence.
Improving Quality for Patients with Lung Cancer in Sussex: The problem identified was inadequate time for patient assessments, a lack of access to support services, and coordination issues between different care sites. The redesign involved establishing a weekly multidisciplinary Combined Cancer Clinic (CCC) at the Sussex Cancer Centre. This clinic offers holistic assessments at any stage post-diagnosis and is designed to be flexible, allowing patients to initiate or cancel appointments as needed. Patients and their GPs are provided with a comprehensive treatment record summary and a detailed assessment and care plan. Initial feedback from both patients and staff has been positive, with benefits including a reduction in non-elective emergencies and the ability to perform certain procedures within the cancer center, thereby avoiding emergency admissions or later outpatient procedures. This initiative significantly improved coordination and access to crucial support services.
These cancer pathway examples demonstrate that while cancer pathways are inherently complex , optimization often involves both specialization (e.g., dedicated CCC for lung cancer) and integration across care settings (e.g., acute to community for breast surgery, primary care support for CYP). This indicates that for complex diseases, a generic "pathway" is insufficient; it requires highly tailored sub-pathways that are nonetheless coordinated across the entire patient journey. This balance between specialization and integration is crucial for managing complexity and delivering high-quality, patient-centered care for conditions with often unpredictable trajectories.
6.2 Improvements in Diagnostic Services
Achieving a Seven-Day Turnaround in Histopathology (Whipps Cross University Hospital NHS Trust): The problem was lengthy delays in histopathology reporting, with a mean turnaround time of 11 days and some cases extending to 40 days, leading to risks of breaching cancer diagnosis targets and wasted resources. The redesign focused on eliminating bottlenecks through meticulous process analysis and problem-solving cycles. Cases are now prioritized by clinical need, and all samples are processed on a first-in-first-out basis. The benefits were significant: the overall turnaround time was reduced from 11 to 4 days, with 95% of results available within 7 days. This enabled colposcopy services to dispatch results letters within two weeks, ensured smoother operation of nurse-led telephone clinics with 100% of results available at the outset, and streamlined the referral of gynecological malignancies to regional cancer centers. The project also eliminated unnecessary telephone calls and administrative waste, improving patient experience through faster, predictable, and guaranteed results, and yielding annual cost savings of £30,000 from reduced follow-up appointments in dermatology.
Using Lean Processes for Cervical Screening Results (Somerset and West Dorset Cervical Screening Service): This initiative addressed an average turnaround time of 22 days for cervical screening results and the imperative to meet the 14-day target. The redesign implemented Lean processes, including stockpiling samples upon receipt and handling them on a 'first in, first out' basis, prioritizing urgent cases for same-day processing, and enhancing communication across the pathway. The results were impressive: all results were returned within 14 calendar days, a standard maintained for over a year, with 95% of results returned within 7 days. There was a 90% reduction in major and minor errors in request details and clinical incident reports. The project achieved a return of between £85,000 and £100,000 per year on an initial investment of £30,000, demonstrating improved patient safety and productivity.
Improving Access and Quality of Care (Audiology - Tinnitus Management Clinic): The problem was lengthy waiting times for tinnitus services (up to 28 weeks), inconsistent information from professionals, and a high proportion of GP referrals to ENT clinics that could be managed directly by audiology. The redesign introduced new guidelines allowing GPs to refer directly to audiology clinics or via an agreed pathway to ENT. Audiologists and hearing therapists now provide services with appropriate access to ENT consultants and MRI scans. Process improvements included simplifying tasks, combining appointments, and implementing telephone follow-up and partial booking. The benefits included a dramatic reduction in waiting times from up to 28 weeks to less than 4 weeks, reduced follow-up appointments, improved patient satisfaction and reassurance, and a potential national saving of £5.9 million per annum by implementing direct access to a tinnitus audiologist for 65,761 patients annually. This also facilitated more effective access for other patients requiring ENT opinions.
Improving Access to Patient Care in the Community (Audiology - Reassessment Service): This project aimed to address the need for more accessible reassessment services for hearing aid assessments and simple repairs, given a growing demand due to an aging population. The redesign involved introducing a 'screening' appointment to reduce clinic time and increasingly providing services in community locations. The model successfully tested the safe and effective delivery of services by associate practitioners. The benefits included maintained clinical quality, with 97% of patients preferring a local service, indicating increased patient satisfaction. There was a 46% reduction in patient visits and a 43% reduction in time spent in clinics, allowing a greater number of patients to be seen within existing resources. The project demonstrated no detrimental impact on patient care, and patients did not return more frequently for reassessment at a local service. This initiative showed a potential national saving of £5.3 million per annum by providing community access via associate practitioners for 205,000 annual reassessments.
The repeated focus on diagnostic services as areas for significant improvement highlights that delays in this stage are major bottlenecks that cascade throughout the entire patient pathway, impacting treatment initiation and overall patient flow. Optimizing diagnostics is therefore a high-impact lever for system-wide efficiency. Furthermore, the audiology case studies demonstrate the successful use of "screening" appointments, community locations, and "associate practitioners" to deliver services. This indicates a strategic approach to capacity management that involves task shifting to appropriate skill levels and decentralizing care closer to patients, thereby reducing pressure on specialist clinics and improving accessibility.
6.3 Enhancements in Acute and Chronic Disease Management (e.g., Heart, Respiratory, Stroke)
Nationwide Stroke Prevention in Atrial Fibrillation: The problem was that many individuals with Atrial Fibrillation (AF) and associated risk factors were not receiving anticoagulant treatment, leading to preventable strokes. The redesign involved implementing the Guidance on Risk Assessment for Stroke Prevention in Atrial Fibrillation (GRASP-AF) tool in primary care. This tool identifies patients at risk and optimizes the use of anticoagulant drugs like warfarin. Benefits included an increased percentage of over 65s on AF registers prescribed warfarin. The initiative identified over 17,500 patients with AF in one network, leading to significant opportunities for stroke reduction. An estimated cost saving of £220,000 return on investment was achieved from pulse checks at flu clinics, which identified 189 new AF cases from 34,201 screened patients. The project aimed to increase GRASP-AF tool use from 830 to 2,000 GP practices by April 2012, ultimately improving quality of care and preventing strokes.
The Advisory Role of NHS Improvement in Implementing Primary Angioplasty (PPCI): This initiative addressed the need to implement Primary Percutaneous Coronary Intervention (PPCI) as the treatment of choice for ST segment elevation myocardial infarction (STEMI) across England. NHS Improvement provided guidance, bespoke support, co-produced publications, acted as an independent expert, and developed a clinical advisory group to facilitate PPCI implementation. The benefits were widespread: an increase in the percentage of STEMIs treated by PPCI from 10% (at the start of the National Infarct Angioplasty Programme) to over 70% in 18 months. Population access to primary angioplasty increased from 27% in 2008 to 88% by February 2011, with a target of 97% by October 2011, ensuring equity of access to PPCI services within 60 minutes for the population. This provided a truly patient-centered approach, benefiting patients in the long term.
Driving Up Quality and Productivity in Cardiac Surgery (St George’s Healthcare NHS Trust, London): The problem was long delays in elective and non-elective cardiac surgery pathways, low pre-assessment attendance, theatre overruns, lack of beds, and mislaid paper referrals. The redesign involved developing a new cardiac surgery pathway that included pre-assessment for all elective patients, a theatre scheduling policy, monitoring of theatre cancellations, implementation of electronic referrals, admission on the day as normal practice, and recruitment of additional staff. The benefits included an increased activity valued at £103,000 to date due to improved productivity. The project improved theatre scheduling, increased pre-assessment and admission on the day, and reduced cancellations and length of stay. It was also cost-neutral due to savings gained by each workstream and encouraged similar improvement projects in cardiology.
Early Diagnosis of Heart Failure: This initiative addressed the complex diagnosis of heart failure and the associated costly outpatient referrals. The redesign promoted the use of a simple blood test (serum natriuretic peptide or NP) in primary care to rule out heart failure and reduce the need for further investigations. The benefits included potential national savings of £13.7 million if all Primary Care Trusts (PCTs) implemented the serum NP test. It improved clinical effectiveness and sped up heart failure diagnosis, reducing the likelihood of acute admissions and unnecessary tests and anxiety for patients without heart failure.
Improving Home Oxygen Services (Hull): The problem identified was the lack of a formal oxygen service, with patients often prescribed long-term oxygen without adequate review, and GPs issuing oxygen based on perceived want rather than clinical need. The redesign involved commissioning a new home oxygen assessment and follow-up service, establishing a multidisciplinary project team, and integrating this with wider COPD pathway service development. The benefits included a reduction in monthly oxygen invoices by £11,378 through reduced therapies and removal of unnecessary oxygen. 428 patients were assessed or reviewed, leading to a reduction in oxygen therapies and flow rates, and 24 patients on oxygen successfully stopped smoking. The initiative provided improved clarity, structure, and focus for the project team, contributing to a 30% reduction in unscheduled hospital admissions and optimization of COPD patient care.
Improving Acute Care in West Sussex (COPD): This project aimed to address avoidable hospital admissions for acute exacerbations of COPD and a lack of clear follow-up pathways after admission. The redesign involved developing a discharge summary for timely and accurate information sharing between secondary and primary care. It identified options for patient follow-up based on clinical need and established mechanisms to ensure these follow-ups occurred. A monthly COPD multidisciplinary meeting was also instigated. The benefits included potential for quality improvements and productivity gains in admissions, readmissions, and hospital bed days used. It improved communication and information quality at discharge, ensured specialist advice was always available through a network of 'respiratory lead nurses,' and facilitated systematic discussion of patients with multiple admissions to avoid future unnecessary hospitalizations.
Integrated Respiratory Service to Improve Outcomes for Patients with Long-Term Respiratory Conditions in West London: The problem was over 5,000 undiagnosed COPD patients, high costs associated with COPD admissions (over £1 million per year), significantly higher death rates due to COPD in the region, and limited joint working between hospital, community, and primary care. The redesign established a multidisciplinary team approach emphasizing engagement and enhanced coordination across all organizations. An integrated COPD patient pathway was agreed upon, introducing community-based respiratory consultant clinics, consultant-led open access respiratory MDT, pulmonary rehabilitation, early supported discharge, and a rapid response telephone service. The benefits were substantial: acute admissions reduced by 19% and readmissions by 66% (2010/11 compared with 2009/10). First and follow-up outpatient appointments were reduced, equating to approximately £170,000 in savings. There was a dramatic reduction in patients presenting without a previous COPD or asthma diagnosis, improved quality of diagnosis, and enhanced patient self-management. This led to better patient outcomes and value for money through shared resources and reduced duplication.
Speeding Up Nottingham Referrals via the ‘Bat Phone’ (Stroke): The problem was delays in admitting suspected stroke patients directly to the hyper acute unit, with many transferred from A&E or emergency admissions units, and poor recording of telephone calls and triage. The redesign implemented a 'direct access into the stroke hyper acute unit' (DASH) project. A direct phone line to the stroke unit, famously dubbed the 'bat phone,' was publicized with a new ring tone and flashing light to alert staff immediately. Information was also disseminated to GPs encouraging direct contact.The benefits included rapid and equitable access to the stroke service, reduced delays in transfer, and decreased admissions via A&E. It also significantly increased awareness of the direct access project within the acute trust and community, ensuring engagement of executive teams and commissioners.
Lewisham Integrated Stroke Project: Stroke patients in Lewisham faced a fragmented journey, often passing through up to seven different teams, with variations in service quality. This resulted in long hospital stays (average 22.5 days) and extended waits for community rehabilitation (often exceeding 12 weeks). The redesign involved re-designing the stroke pathway with a strong focus on joint working and integrated communication systems. The workforce was reconfigured to include new therapy posts and integrate rehabilitation from several teams into a single, cohesive unit. Discharge processes were simplified, coding inaccuracies addressed, and a key worker system implemented. The benefits were significant: the average length of hospital stay was reduced to 19 days (by March 2010), and the proportion of stroke patients spending 90% of their stay on the stroke unit increased to over 80%. Community waiting times for therapy were reduced by 10 days or more for some therapies. The project improved coordination of care and provided a more personalized, holistic service. Patients praised the rapid response, motivating and caring staff, and quick access to equipment and adaptations, realizing better patient outcomes and value for money through shared resources and reduced duplication.
Involving Stroke Patients in Dorset: This initiative addressed the need to actively involve patients, families, and carers in shaping stroke services. The redesign involved the Dorset Cardiac and Stroke Network actively seeking views through various approaches, including focus groups and Discovery Interviews, to directly influence service design and delivery.The benefits included ensuring that patient and carer experiences were at the heart of service redesign, improving patient and public involvement in line with national requirements, and contributing to a more patient-centered approach to care.
These case studies demonstrate that "integration" in patient pathways is not a single concept but encompasses various dimensions: integration of services (e.g., community-based consultant clinics), integration of information (e.g., discharge summaries), integration of teams (e.g., multidisciplinary meetings, single integrated teams), and integration of patient perspectives (e.g., Dorset Stroke Project). This indicates that successful pathway optimization requires a layered approach to integration across clinical, operational, and patient engagement domains. Furthermore, the success of initiatives like the "bat phone" for stroke referrals (a simple communication tool) and the emphasis on "patient praise" and "psychological boost" alongside quantifiable metrics, suggests that seemingly "soft" interventions (e.g., improved communication, patient reassurance) can have a significant impact on "hard" outcomes like reduced delays, improved flow, and ultimately, clinical effectiveness. This indicates that human-centered design and communication strategies are as vital as technological and process changes.
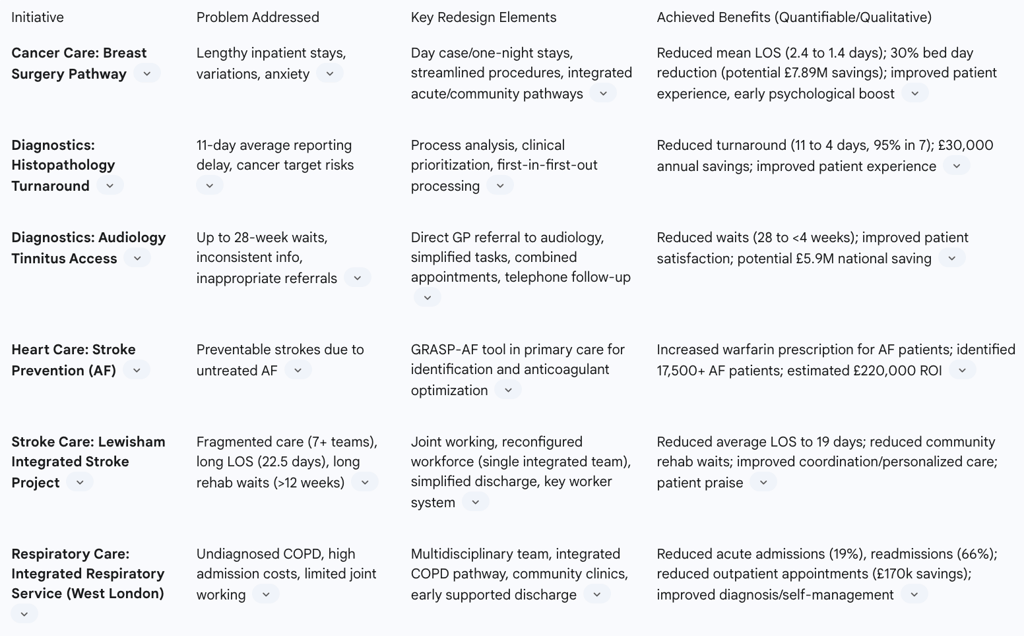
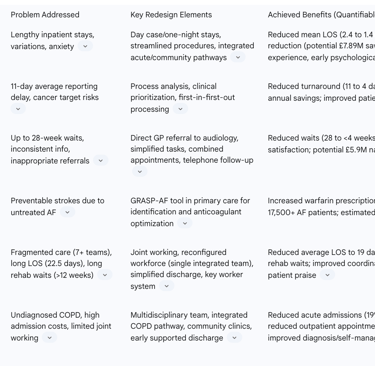
Table 4: Selected Successful Pathway Redesign Initiatives and Achieved Benefits
Conclusion and Recommendations
7.1 Key Strategic Imperatives
The comprehensive analysis of patient pathways within the NHS reveals several strategic imperatives for navigating care and optimizing services. Firstly, patient pathways are not merely descriptive; they serve as the fundamental blueprint for standardizing care, reducing unwarranted variation, and ultimately improving clinical outcomes across the vast and complex NHS system. Their existence underscores the necessity of structured frameworks to ensure consistent, high-quality care.
Secondly, digitalization has emerged as a non-negotiable enabler of modern healthcare. Digital tools like the NHS e-Referral Service (e-RS) and the Booking and Referral Standard (BaRS) are profoundly transforming patient journeys by streamlining referrals, enhancing information sharing, and empowering patients with greater choice and control. Continued, strategic investment in interoperable digital infrastructure is critical for future efficiency gains.
Thirdly, the persistent bottlenecks in NHS patient pathways stem from a complex interplay of systemic, operational, and patient-centric challenges. These include chronic workforce shortages, significant underfunding leading to capacity crises, operational inefficiencies such as fragmented assessments and diagnostic delays, and patient-specific barriers related to accessibility and communication. This multifaceted nature of the challenges dictates that solutions must be holistic and span across traditional organizational boundaries.
Fourthly, the human element is paramount to the success of any optimization effort. Even the most meticulously designed processes and advanced technologies will falter without strong, visible leadership, a supportive organizational culture, active staff engagement, and meaningful patient co-design. The psychological impact of efficient and compassionate care on patients is a key, often underestimated, outcome.
Finally, patient pathway optimization is an ongoing journey, not a singular destination. Pathways are dynamic entities that require constant evaluation, adaptation, and innovation. Learning from successful case studies and consistently applying principles like Lean methodologies and data-driven management are essential for sustained progress and continuous improvement.
7.2 Actionable Recommendations for Future Pathway Optimization
Based on the detailed analysis, the following actionable recommendations are proposed to drive future optimization of patient pathways within the NHS:
1. Prioritize Strategic Workforce Planning and Investment: The foundational imperative for system stability and capacity is a robust and motivated workforce. Addressing the root causes of staffing shortages and retention issues requires long-term, strategic workforce planning, competitive remuneration packages, and initiatives aimed at improving work-life balance for all NHS staff. Without sufficient and well-supported personnel, even the most efficiently designed pathways will struggle to deliver their intended benefits.
2. Accelerate and Deepen Digital Transformation with an Equity Lens: It is crucial to fully implement and integrate interoperability standards, such as BaRS, across all care settings, investing in advanced software solutions for real-time data analysis and electronic work management. Concurrently, it is imperative to ensure robust non-digital support channels and inclusive design strategies. This approach will prevent the exacerbation of health inequalities for digitally excluded or less digitally literate populations, ensuring that the immense efficiency gains from digitalization are equitably distributed across all patient demographics.
3. Implement System-Wide Patient Flow Management: A holistic, system-wide approach to patient flow must be adopted, moving beyond isolated departmental silos. The focus should be on identifying and strategically addressing true bottlenecks, such as diagnostic delays and discharge complexities, through detailed diagnostic work. Operational improvements should be sequenced strategically, for example, by initiating improvements at the end of a pathway and working backward to maximize throughput across the entire system. This comprehensive view is essential to ensure that improvements in one area do not merely shift problems to another, but rather contribute to sustainable, system-wide enhancements.
4. Embed Patient and Public Co-design into Pathway Development: Patients, carers, and the wider public must be systematically involved in the design, evaluation, and communication of all patient pathways. This includes translating complex clinical terminology into accessible language to enhance understanding and engagement. Patient-centered design leads to more effective, acceptable, and equitable services, fostering greater adherence to care plans and ultimately improving patient satisfaction and clinical outcomes. Their lived experiences provide invaluable perspectives that can identify pain points and inform more effective solutions.
5. Foster a Culture of Continuous Quality Improvement and Learning: It is vital to promote visible and accessible leadership that actively champions quality improvement initiatives and encourages an open learning culture throughout the organization. Integrating patient stories at all levels of governance can provide powerful motivation and context for improvement efforts. Furthermore, the consistent utilization of established quality improvement methodologies, such as Lean and Plan-Do-Study-Act (PDSA) cycles, combined with adherence to evidence-based guidelines like those from NICE, will drive ongoing pathway refinement and ensure sustained progress.
Additional Resources
For readers interested in exploring the topic of patient pathways in the NHS further, here are some reliable sources and further reading materials:
