NHS Integrated Care and Role of Unified Digital Triage
Explore how unified digital triage platforms transform NHS Integrated Care Systems, reducing A&E attendance by 28%, streamlining patient journeys across organisational boundaries, and enabling population health management through shared clinical decision-making frameworks.


The National Health Service (NHS) in the United Kingdom has long contended with the challenges posed by fragmented healthcare services. This fragmentation, particularly evident in the divisions between primary, secondary, and social care, frequently results in discontinuous patient experiences and represents a persistent policy concern. The drive towards "integrated care" stems from a fundamental desire to enhance patient experience and achieve greater efficiency and value from the health delivery system. This is particularly critical given the increasing incidence of chronic diseases within an aging population, which places significant demands on existing care structures. The inherent lack of service coordination for individual patients, coupled with the structural and cultural isolation of generalist from specialist medicine and health from social care, underscores why integration is not merely a logistical aspiration but a deep-seated systemic necessity. The implication is that effective integration requires profound changes that extend beyond mere technological adjustments, touching upon the very organizational and cultural fabric of the NHS.
In parallel with the evolution of integrated care, digital transformation has emerged as a pivotal enabler for addressing these systemic challenges. The adoption of digital health solutions is increasingly recognized as central to shifting the healthcare paradigm from a reactive "diagnose and treat" model to a more proactive "predict and prevent" approach. The COVID-19 pandemic served as a significant catalyst, rapidly accelerating the pace of digital transformation across the NHS. This period demonstrated unequivocally how technology and data could facilitate the delivery of safe and compassionate care, while also significantly improving communication channels among healthcare professionals.
This report aims to systematically explore the foundational principles of NHS Integrated Care Systems (ICSs) and the operational mechanisms of Unified Digital Triage (UDT). It will delve into their synergistic relationship, examining the tangible benefits realized through their combined application, and addressing the significant challenges encountered during implementation. Furthermore, the report will analyse the guiding policy landscape and present real-world case studies that illustrate practical successes. The analysis will culminate in strategic recommendations for the future development and scaling of these critical initiatives.
Understanding NHS Integrated Care Systems (ICSs)
Integrated care represents an overarching organizational principle for healthcare delivery, designed with the primary objective of enhancing patient care and experience through improved coordination. Distinct from this principle, "integration" refers to the specific methods, processes, and models employed to achieve this improved coordination. Integrated Care Systems (ICSs) have been established across the NHS to operationalize this vision, aiming to join up care delivery by fostering collaboration among local partners, including the NHS, local councils, voluntary sector organizations, and other key stakeholders such as housing, employment, education, and justice services.
The core objectives of ICSs are multifaceted: to improve outcomes in population health and healthcare, to address inequalities in health outcomes, patient experience, and access to services, to enhance productivity and achieve greater value for money, and to support broader social and economic development within their respective areas. Achieving these objectives necessitates a shared vision among all involved parties—those responsible for planning, financing, and providing services—along with the adoption of combined processes and mechanisms that consistently keep the patient's perspective at the forefront.
The evolution of integration within the NHS reflects a continuous journey towards more comprehensive and collaborative models. Earlier initiatives, such as the introduction of National Service Frameworks (NSFs) for specific conditions or the merging of regulators to facilitate joint inspection, focused on achieving consistency and coordination within particular sectors or for specific conditions. The current emphasis on ICSs, however, signifies a shift towards a broader, geographically-based, and multi-sectoral approach. This framework prioritizes population health and addresses the wider determinants of health, moving beyond siloed, condition-specific or regulatory integration to encompass a more holistic view of community well-being.
Structural Components: Integrated Care Boards (ICBs), Provider Collaboratives, and Integrated Neighbourhood Teams
The structural framework of an ICS is designed to facilitate this collaborative and integrated approach:
Integrated Care Boards (ICBs): These are NHS organizations that hold primary responsibility for planning health services tailored to their local population's needs. Each ICS area is served by one ICB, which plays a pivotal role in strategic decision-making and resource allocation.
Provider Collaboratives: These represent partnership arrangements involving at least two trusts that work together across multiple geographical areas. Their shared purpose is to plan, deliver, and transform local services. Key aims include reducing unwarranted variation in care, enhancing system resilience through mutual aid, and promoting specialization and consolidation of services where it leads to improved outcomes and greater value.
Integrated Neighbourhood Teams: These multidisciplinary teams comprise professionals from primary and secondary care services, as well as social and voluntary sectors. They work collaboratively, leveraging data and personalized care approaches to address the holistic needs of individuals. These teams are particularly crucial for providing proactive, joined-up care to higher-need groups, such as the frail elderly or individuals with multiple long-term conditions.
Rationale for ICSs: Addressing Complex Conditions, Ageing Populations, and Health Inequalities
The establishment of ICSs is a strategic response to profound demographic shifts and escalating systemic pressures within the NHS. The population is living longer, often with more complex and multiple chronic conditions, which places immense strain on traditional, fragmented care models. ICSs were specifically created to encourage and enable local organizations to collaborate effectively, understand the health and wellbeing needs of their communities, agree on shared priorities, and develop innovative strategies for delivering efficient, needs-based care.
The core rationale for ICSs is to prevent health deterioration, support individuals in maintaining independence, and provide comprehensive care for those with complex and multiple needs. A central tenet of their approach is a strong focus on prevention, leveraging data and population health management techniques to proactively identify individuals most at risk and determine the services they might require. This emphasis on prevention and proactive care is a direct response to the macro-level challenges posed by an aging population and the increasing prevalence of chronic diseases, representing a strategic imperative to ensure the long-term sustainability and effectiveness of the NHS in the face of evolving societal health demands.
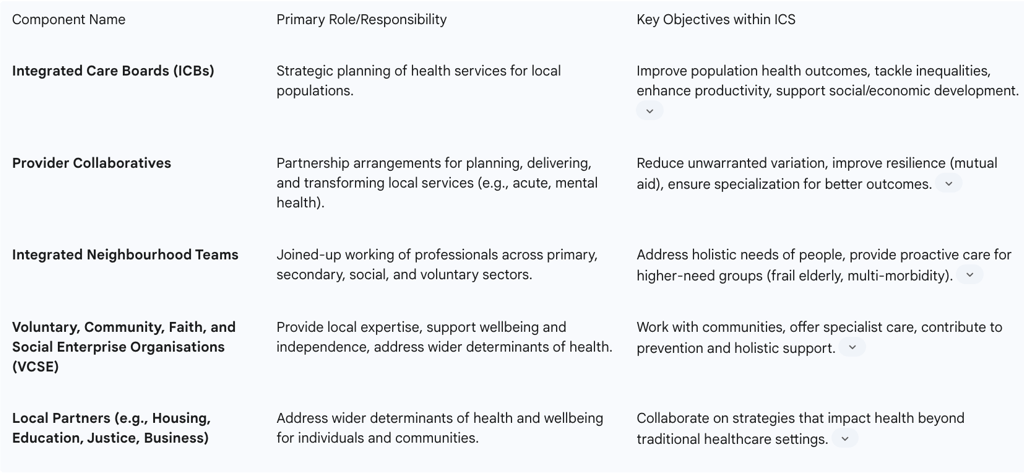
To further illustrate the organizational structure and responsibilities within an ICS, Table 1 provides a concise overview of its key components.
Table 1: Key Components of NHS Integrated Care Systems (ICSs) and their Roles
The Concept and Functionalities of Unified Digital Triage
Unified Digital Triage (UDT) encompasses a range of digital tools and processes designed to efficiently manage patient requests and direct individuals to the most appropriate care pathway. This system is built upon foundational concepts of triage and care navigation, adapted for the digital age.
Defining Digital Triage, Care Navigation, and Total Triage Models
Triage: At its core, triage involves determining the necessary level of support, the urgency with which it should be provided, and identifying the healthcare professional or service best equipped to manage the patient's condition or request.
Care Navigation: This is a structured approach, often implemented by appropriately trained non-clinical staff, to collect initial patient information and then guide individuals to the correct service or team member. The objective is to redirect a significant proportion of patient contacts—over 15%—away from direct GP consultations towards self-care, community pharmacy, or other local services.
Digital Triage: This specifically refers to remote triage conducted using digital tools, such as online consultation (OC) platforms, online messaging (OM) tools, or other secure two-way digital communication channels.
Total Triage: This model signifies a comprehensive approach where every patient request is remotely screened before being directed to an appropriate pathway or consultation type. This can involve a combination of both digital and traditional methods. A more specific form, "total digital triage," mandates that every patient request, even those received via telephone or in-person at reception, is inputted into an online consultation tool for systematic screening.
Core Functionalities: Structured Information Gathering, Query Filtering, Navigation, Prioritization, and Allocation
Effective UDT relies on several core functionalities that are intrinsically linked, with data serving as the central nervous system that enables their seamless operation. The efficacy of UDT is entirely dependent on the quality, structure, and intelligent analysis of patient data, implying that investment in data standards, capture, and analytics is as crucial as the digital tools themselves.
Structured Information Gathering: This involves collecting comprehensive patient data at the initial point of contact, regardless of whether the interaction occurs online, via phone, or in-person. This data typically includes demographics (age, sex, and who is completing the form), a detailed description of the problem (symptoms, new/existing, duration, progression), any attempted remedies, patient expectations, preferred consultation mode (phone, face-to-face, video, message), preferred healthcare professional, availability, and specific communication needs (e.g., interpreter). Beyond initial contact, Remote Patient Monitoring (RPM) programs further contribute by collecting and analysing patient-generated health data (PGHD), such as vital signs and symptoms, transmitted digitally from the patient to the care team.
Query Filtering: Once information is gathered, UDT systems inform the filtering of both clinical and administrative queries. Advanced AI capabilities can automatically identify whether a request is administrative or clinical in nature and assign it to the appropriate service, streamlining initial processing.
Navigation: This functionality directs requests to the most suitable service or member of the care team. Intelligent navigation systems are designed to guide patients seamlessly across the entire spectrum of care, from self-care options to primary care, diagnostics, specialist care, and even Accident & Emergency services.
Prioritization: UDT systems are crucial for prioritizing requests and allocating them to the right appointment type—considering timeframe, the most appropriate healthcare professional, and modality—to effectively meet the patient's needs. AI-powered systems can enhance this by applying risk stratification models, such as RAG (red, amber, green) ratings, to identify high-risk individuals and optimize care prioritization.
Allocation: This final step involves directing patients to the most appropriate service or professional, or enabling patients to self-book their appointments directly, thereby reducing administrative bottlenecks.
Digital Tools Supporting UDT: Cloud-based Telephony, Online Consultation Platforms, Messaging Tools, and Self-booking Links
A suite of digital tools underpins the functionalities of UDT:
Cloud-based Telephony: Modern telephony systems, which all practices are encouraged to adopt by 2025, offer advanced features such as call-back and intelligent call routing. These capabilities are vital for supporting care navigation and ensuring that patient data is easily accessible to staff.
Online Consultation Tools: These platforms enable patients to submit requests for both clinical and administrative assistance. For practice staff, they provide functionalities to receive, review, prioritize, allocate, action, and record patient requests. They are instrumental in ensuring equitable access and choice of contact channels for patients, facilitating structured information collection, and enhancing workflow efficiency.
Messaging Tools: These tools support care navigation workflows by allowing staff to request further information from patients, send reminders and alerts, and manage administrative requests. Two-way messaging systems are particularly important for dynamic digital triage processes.
Self-booking Links: Digital tools that generate self-booking links empower patients to choose and book appropriate appointments directly, significantly reducing administrative workload and bottlenecks in the system.
Operational Steps for Implementing Care Navigation (Understand, Design, Go-live, Measure & Improve)
Implementing care navigation, as a form of UDT, is not a static project but an iterative process, emphasizing continuous improvement rather than a one-off deployment. This implies that successful UDT requires an organizational culture of continuous learning and agility, rather than a rigid, one-time technological rollout. The process typically involves four key steps:
Understand: This initial phase requires measuring and analysing existing demand and capacity data to establish a baseline. Practices should undertake an audit of avoidable appointments to identify cases that could potentially be navigated elsewhere. Based on this data, key metrics are decided upon to demonstrate future improvements in the care navigation process.
Design: This involves creating a structured approach for collecting patient information, developing a clear care navigation protocol (which outlines how patients are filtered and directed to internal or external resources), compiling a comprehensive directory of services, and providing thorough training for staff involved in care navigation.
Go-live: This step focuses on the practical implementation and testing of the designed plan. This can include immediate "quick wins" such as updating telephone messages, creating a staff skills matrix, training care navigators, and leveraging cloud-based telephony. It then progresses to comprehensive staff training, refining the care navigation protocol, developing the service directory, aligning appointment books, and fully utilizing digital tools for information capture and communication. Crucially, communicating these changes to patients through informative telephone messages, text messages, website descriptions, and social media is vital for successful adoption.
Measure & Improve: The final, ongoing step involves evaluating the success of the implemented changes using data-driven measures. This includes tracking reductions in avoidable appointments, improvements in continuity of care, and decreases in complaints. Sustainability planning is key, focusing on maintaining gains, expanding successful approaches across Primary Care Networks (PCNs), troubleshooting any emerging problems, and ensuring ongoing training and monitoring to adapt and refine the system.
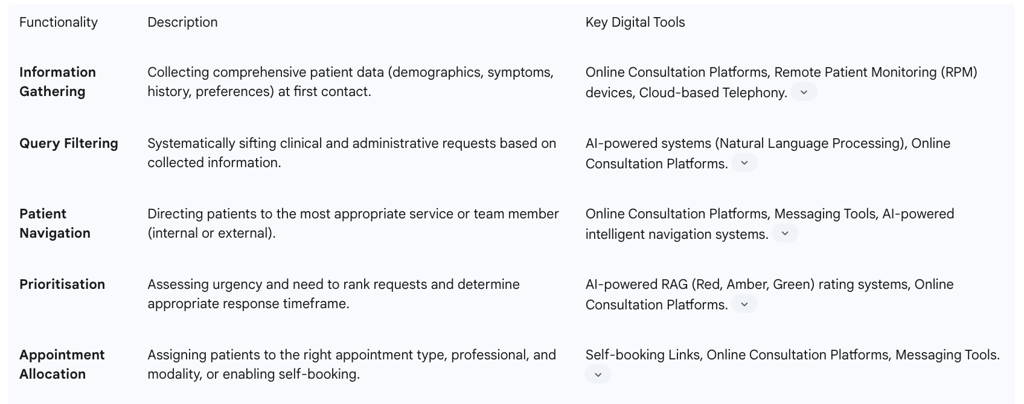
Table 2 provides a summary of the core functionalities of UDT and the digital tools that enable them.
Table 2: Core Functionalities and Digital Tools of Unified Digital Triage
Synergies: How Unified Digital Triage Enhances Integrated Care
Unified Digital Triage (UDT) is not merely a standalone technological enhancement; it acts as a powerful catalyst for achieving the broader objectives of NHS Integrated Care Systems (ICSs). The synergistic relationship between UDT and integrated care manifests across several critical domains, fundamentally reshaping patient flow, information sharing, and coordinated service delivery.
4.1 Optimizing Patient Flow and Access
UDT systems are designed to transform patient access from a reactive, often chaotic process into a proactive, guided journey. Historically, patients frequently found themselves in the "wrong queue," leading to frustrating delays and re-directions, akin to a gratuitous game of snakes and ladders. Long waits in A&E departments have been associated with significant adverse outcomes, and patients risk being shunted between low-acuity settings when their problems are more serious. The ease of getting a GP appointment, for instance, significantly declined between 2012 and 2023. UDT directly addresses these issues by fundamentally redesigning how patients access and move through the healthcare system.
Intelligent Navigation as Default: UDT systems are engineered to guide patients seamlessly to the most appropriate care pathway across the entire service spectrum, encompassing self-care, primary care, diagnostics, specialist care, and Accident & Emergency services. This intelligent navigation facilitates a dynamic "channel shift," allowing patients to interact via online platforms, phone, or in-person, as best suits their needs and the urgency of their condition.
AI-Supported Auto-routing: Advanced platforms leverage Artificial Intelligence (AI), including natural language processing, biometric data capture, and analysis of patient history, to accurately auto-route cases. These systems are capable of detecting and escalating "red-flag" symptoms, even when submitted through online interactions, wearable devices, or home monitoring systems, including during out-of-hours periods.
Direct Self-Booking: Digital systems empower patients to directly book their own appointments, which significantly reduces administrative workload and alleviates bottlenecks within the service. This capability shifts administrative burden from staff to patients, enabling more efficient allocation of resources.
Reduced Unnecessary Interactions: By intelligently directing patients to the appropriate service from their initial point of contact, digital triage aims to "short-circuit" avoidable touchpoints in the patient journey. This not only saves patients millions of unnecessary journeys but also conserves billions of pounds for the NHS, by optimizing resource allocation and reducing demand on overstretched services. The shift from reactive queues to proactive pathways represents a fundamental redesign of how patients access and move through the healthcare system, ensuring more timely and appropriate care.
4.2 Facilitating Information Sharing and Data Integration
The power of UDT to enhance integrated care is deeply rooted in its capacity to facilitate comprehensive information sharing and data integration. This capability allows for a shift from simply sharing static information to actively using data for foresight, enabling proactive and personalized care.
Unified Digital Health Records: A central ambition is the creation of a single, secure, and authoritative digital health record for every citizen. This record would span all health and social care touchpoints, effectively eliminating inefficient processes such as the manual handling of referral and discharge letters. NHS England has set ambitious targets, aiming for 100% Electronic Patient Record (EPR) adoption by NHS trusts by March 2025, with all constituent organizations within an ICS expected to be connected to an integrated health and care record by 2024.
Interoperability Mandates: Regulatory frameworks are increasingly mandating interoperability between GP, hospital, pharmacy, and social care records. This is crucial for overcoming the inefficiencies caused by fragmented, siloed data systems. NHS England Digital Services for Integrated Care (DSIC) plays a key role by publishing standards and capabilities, defining assurance processes, and standardizing integration to ensure digital products operate seamlessly across various healthcare settings.
Data Lakes and Integrated Information: The combination of health and social care data into comprehensive "data lakes" presents an unprecedented opportunity to profoundly impact people's lives. By understanding the multifaceted factors that contribute to illness, this integrated data supports the journey to health, with the potential to extend not just lifespan but also "health span"—the period of life spent in good health. These data lakes are structured to provide usable information for healthcare teams, with clear, definable outcomes, and the integration of genomic data further catalyzes the potential for personalized and highly effective interventions.
Predictive Analytics: Building upon a data-first system, advanced population health management leverages predictive analytics to guide resource allocation, inform service design, and drive preventative outreach programs. For example, AI can forecast the demand for blood plasma or predict the risk of missed outpatient appointments, allowing for proactive adjustments.
AI for Data Extraction: AI technologies can efficiently identify and code diagnoses buried within unstructured information found in electronic health records (EHRs). This capability is vital for identifying patients who might otherwise miss out on preventative care, thereby increasing the uptake of crucial preventative management strategies.
Patient-Carried Records: A future vision includes empowering patients to digitally carry their own records. These records would be safe, user-friendly, and secure, traveling with the patient to ensure continuity and accessibility of their health information. The NHS App is central to this vision, empowering citizens to access and interact with their health and care records, including viewing test results, managing medications, and booking appointments. The combined impact of unified records, data lakes, predictive AI, and remote monitoring points to a future where healthcare is not a series of episodic interventions but a continuous, personalized journey. This enables a fundamental shift in the relationship between individuals and the healthcare system, moving towards continuous health management and preventative interventions tailored to individual needs, rather than solely disease treatment.
4.3 Enabling Coordinated Service Delivery
UDT plays a pivotal role in enabling the operationalization of integrated care, particularly through the development of digital "nerve centres" and the strategic deployment of AI.
Community-Based Healthcare: The future of healthcare delivery increasingly envisions services provided within communities. This involves developing local hubs that offer diagnostics, specialist-led clinics, and multidisciplinary community teams, thereby reducing the need for patients to travel extensively for most of their care. This aligns with the broader strategic shift towards delivering more care in community settings to alleviate pressure on hospitals, allowing them to focus on the sickest patients.
Proactive Care Management Teams: These teams are designed to actively identify individuals at high risk of deteriorating health and intervene early. This proactive approach significantly reduces the reliance on crisis-driven care and ensures timely interventions, improving patient outcomes and reducing emergency admissions.
AI-Based Resource Allocation: Full AI-based triage systems are capable of directing patients to the right clinicians at the optimal time. This transforms demand planning into a sophisticated, data-driven process, making surges in demand more predictable and manageable. By optimizing patient flow, these systems also free up valuable clinician capacity, helping to mitigate burnout and improve staff morale.
Ambient Scribes and Clinical Decision Support: AI-powered ambient scribes can automatically transcribe and summarize consultations, generating automated tasks, coding, and referral letters. This significantly reduces the administrative overhead for healthcare professionals, allowing them to dedicate more time to direct patient care. Furthermore, AI provides real-time feedback from patient records, supporting high-quality clinical decision-making by offering relevant insights and recommendations.
Nerve Centres: These represent the operational apex of integrated care, enabled by UDT's data aggregation capabilities. Nerve centres provide a comprehensive, real-time view of resources across the entire healthcare ecosystem, including hospital and community bed stock, primary and urgent care appointments, and ambulance positions and availability. This mirrors the sophisticated logistics systems used by multinational corporations, enabling a truly responsive healthcare system. By analysing demand patterns, these centres can dynamically deploy teams to areas of greatest need, optimizing resource allocation and improving patient outcomes. This capability signifies a move beyond simply sharing static patient records to a dynamic, responsive system that can allocate resources and deploy teams based on real-time demand and capacity, leading to greater agility and efficiency in service delivery.
Dynamic Digital Care Plans: For severely frail patients with complex needs, dynamic digital care plans are implemented and continuously supported. These plans are updated following every significant change, such as hospital admissions, medication adjustments, or social care changes, acting as a single, clear, and up-to-date record that travels with the patient. This ensures that the entire system takes collective responsibility for their part of the patient's care, enhancing coordination and continuity.
Benefits of Unified Digital Triage in Practice
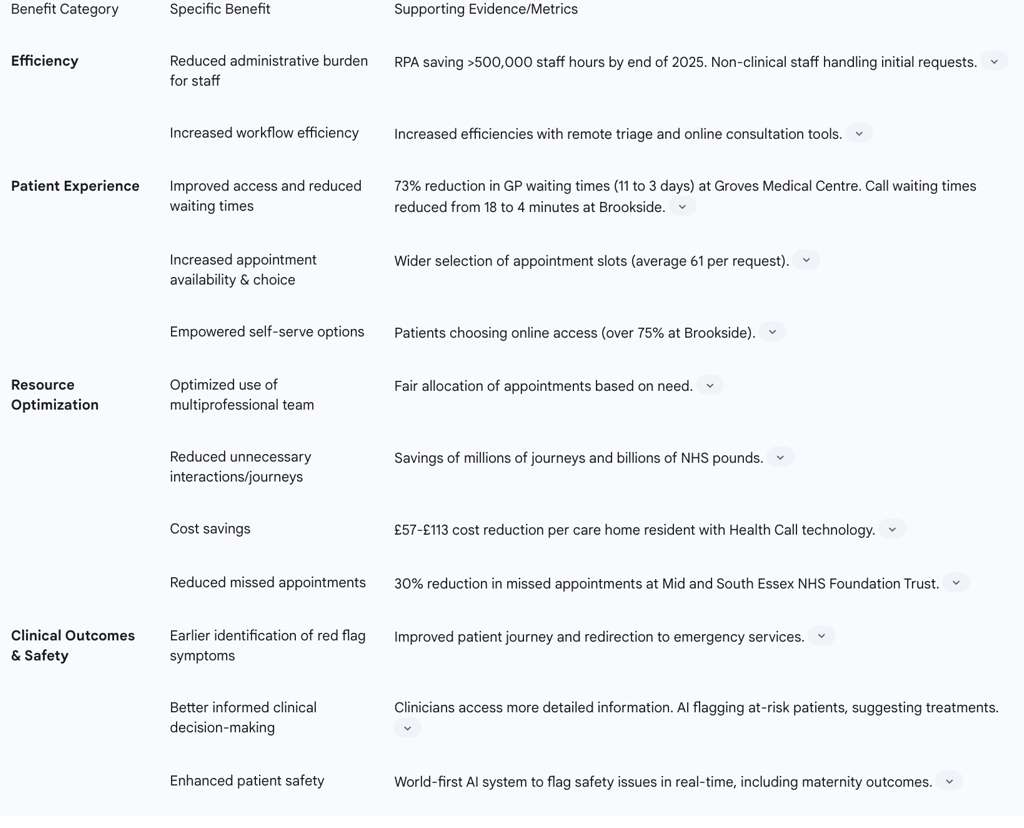
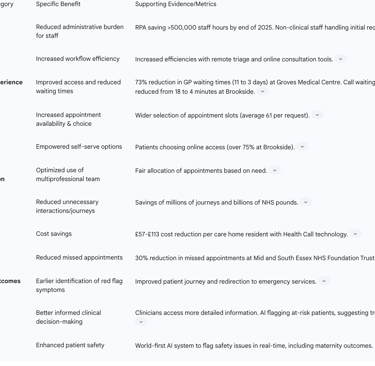
The implementation of Unified Digital Triage (UDT) within the NHS Integrated Care Systems yields a multitude of benefits, translating into improved efficiency, enhanced patient experience, optimized resource utilization, and ultimately, better clinical outcomes and patient safety.
Improved Efficiency and Reduced Administrative Burden
UDT significantly streamlines healthcare operations, leading to notable efficiency gains. The ability to implement remote triage, particularly with the aid of online consultation tools, demonstrably increases efficiencies. This allows for consultations to be closed directly via written communication in many instances, reducing the need for subsequent telephone calls or face-to-face appointments. A key advantage is the reduction in administrative tasks for clinicians, as non-clinical staff and automated systems handle initial patient requests and information gathering. Robotic Process Automation (RPA) and Artificial Intelligence (AI) have the potential to save hundreds of thousands of staff hours by automating repetitive tasks, freeing up valuable human resources. This establishes a clear cause-and-effect: UDT's efficiency improvements directly free up valuable clinical time, allowing healthcare professionals to focus on more complex cases and patient-facing activities, thereby addressing workforce pressures. For example, RPA could save the NHS more than 500,000 hours of staff time by the end of 2025.
Enhanced Patient Experience and Access to Care
UDT fundamentally transforms the patient journey, moving beyond mere convenience to foster greater patient empowerment and trust. The system prioritizes care based on clinical need, ensuring patients gain access to the right healthcare professional within an appropriate timeframe. This leads to increased appointment availability and offers a wider variety of access options for patients. UDT empowers patients with self-serve options and creates a more transparent process for accessing care. Concrete examples demonstrate this impact: at Brookside, the use of online forms led to a significant reduction in call waiting times, from an average of 18 minutes to just 4 minutes. Furthermore, remote consultation methods are particularly convenient for patients of working age, enabling them to access care without needing to take time off work. The shift towards patient agency and transparency, facilitated by UDT, can foster greater trust in the healthcare system.
Optimized Resource Utilization and Cost Savings
The strategic implementation of UDT facilitates a more efficient allocation of resources, leading to substantial cost savings and contributing to the long-term financial sustainability of the NHS. By optimizing the use of the multiprofessional team, UDT ensures that appointments are allocated fairly and appropriately, matching patient needs with the most suitable clinician. The reduction in unnecessary interactions and avoidable patient journeys directly translates into significant savings for the NHS. Pilot programs have demonstrated tangible financial benefits; for instance, the Health Call technology implemented in care homes in the North East UK resulted in a cost reduction of £57 to £113 per resident. AI-powered systems have also proven effective in reducing missed appointments by as much as 30%, preventing hundreds of non-attendances and allowing thousands of additional patients to receive care. Research indicates that digital and data use cases deployed at scale could unlock £15-25 billion annually in the UK, highlighting that UDT is a critical tool for strategic resource reallocation and systemic sustainability.
Better Clinical Decision-Making and Patient Safety
UDT enhances clinical decision-making and significantly improves patient safety. The structured collection of information and intelligent filtering capabilities enable earlier identification of "red flag" symptoms in the patient journey. Clinicians gain access to more detailed and organized patient information, which supports better-informed decision-making. AI-enabled Electronic Patient Record (EPR) systems can augment human decision-making by flagging at-risk patients, suggesting potential treatment options, or predicting demand, thereby supporting overstretched teams. Furthermore, pioneering AI systems are being developed to scan NHS systems in real-time to identify and flag safety issues, including a new maternity outcomes signal system designed to detect higher rates of stillbirth, neonatal death, and brain injury, ultimately preventing failures before they escalate.
Table 3 provides a summary of the key benefits of Unified Digital Triage within NHS Integrated Care, supported by quantifiable evidence where available.
Table 3: Key Benefits of Unified Digital Triage in NHS Integrated Care
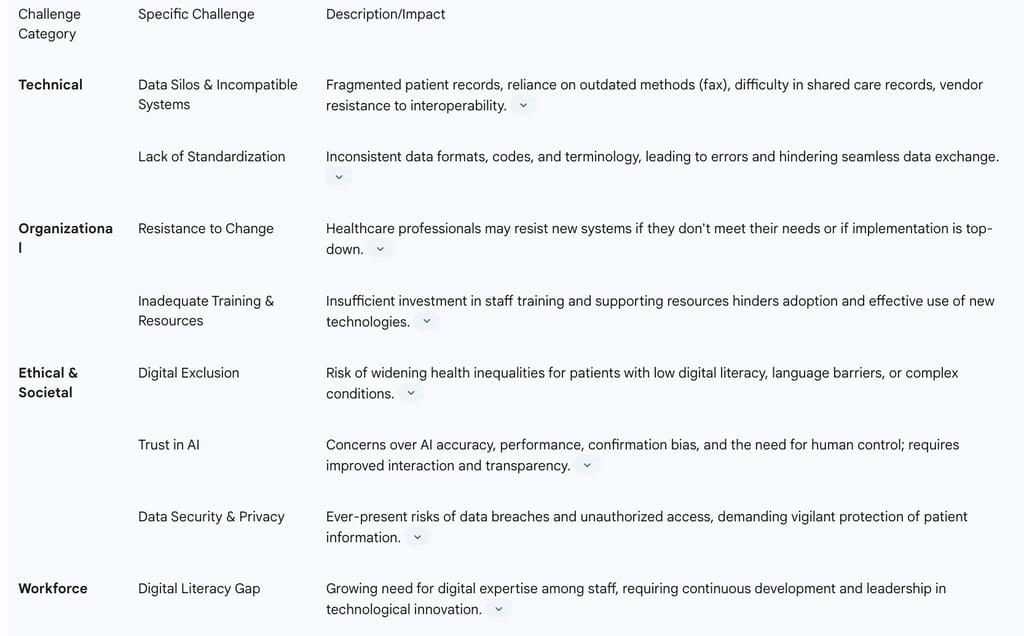
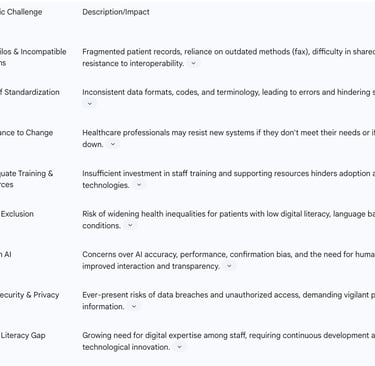
Challenges and Considerations for Implementation
Despite the significant potential of Unified Digital Triage (UDT) within NHS Integrated Care, its widespread and effective implementation faces several substantial challenges. These hurdles span technical, organizational, ethical, and workforce domains, requiring careful consideration and strategic mitigation.
6.1 Data Interoperability and Siloed Systems
One of the most profound and persistent obstacles to digital transformation in the NHS is the pervasive issue of data interoperability. The NHS currently operates on a multitude of incompatible IT systems that are unable to communicate effectively with one another. This results in patient records being trapped in digital silos, and referrals often still rely on outdated methods such as paper files and fax machines. This lack of seamless information exchange is a fundamental structural impediment to nearly every proposed reform. For instance, delivering integrated neighbourhood health services becomes exceedingly difficult if a GP cannot access a patient's hospital records, and implementing outcome-based commissioning is hampered when data exists in incompatible formats across various systems.
The challenges related to interoperability are multifaceted: a significant lack of standardization, where most health information systems (HIS) use proprietary formats and unique data elements, leads to non-interoperable and disparate data versions. Even within the same system, inconsistencies can arise due to varied use of codes, abbreviations, and terminology, complicating medical interpretations. Furthermore, vendors often resist true interoperability and charge premium fees for integration, contributing to the patchwork approach that perpetuates inequalities. This highlights that interoperability is not just a technical challenge but a deeply entrenched organizational and commercial issue that requires systemic intervention. Without mandatory interoperability standards enforced at a national level, the ambition for a truly integrated, data-driven NHS will remain constrained.
6.2 Digital Exclusion and Equity
While digital solutions offer considerable benefits for efficiency and access, there is a critical need to ensure they remain accessible to all segments of the population. Without proactive strategies for digital inclusion and a multi-channel approach, UDT could inadvertently widen existing health inequalities, contradicting the core ICS objective of tackling inequalities in access and outcomes.
National digital inclusion policies have provided funding for community-led training programs to help both patients and professionals effectively use emerging technologies. However, certain patient groups face inherent barriers. Individuals with low digital literacy or for whom English is not their first language may find remote consulting more challenging. Similarly, patients with increasingly complex conditions and multiple comorbidities may find remote consultation a barrier to the holistic assessment of their needs, requiring more nuanced, in-person interactions. Ensuring equitable access necessitates a hybrid approach that combines digital innovation with traditional access points and targeted support for digitally disadvantaged populations.
6.3 Governance, Ethics, and Trust
The deployment of UDT, particularly systems incorporating Artificial Intelligence (AI), introduces significant governance and ethical considerations. Data security and patient privacy are paramount, with ever-present risks of data breaches and unauthorized access. Building trust in AI-based triage systems is crucial for their successful adoption, requiring improved interaction design that adapts to users' competencies and expertise.
Concerns persist regarding AI's accuracy and performance, as well as the potential for confirmation bias, which underscores the critical importance of human oversight and control. Robust governance frameworks are essential for any AI tools, focusing on their ethical application and rigorously measuring their value in patient outcomes. The psychological and ethical dimensions of AI adoption mean that even technically sound AI will only achieve widespread acceptance and effective use if trust deficits among both healthcare professionals and patients are addressed, ensuring transparency, accountability, and a clear understanding of AI's limitations and oversight mechanisms.
6.4 Workforce Adaptation and Training
Achieving successful technology transformation within a large organization like the NHS is inherently difficult, often met with natural resistance from healthcare professionals if new systems do not adequately meet their needs. There is a growing and exponential need for nurses and other healthcare staff with digital expertise and the ability to lead change. However, inadequate investment in training and resources, coupled with existing hierarchical structures, can significantly hinder the adoption of new digital tools and processes.
This highlights that technology alone is insufficient; successful UDT implementation requires significant investment in workforce training, digital literacy initiatives, and comprehensive change management strategies. These efforts are necessary to overcome resistance and ensure that staff are not only equipped with the necessary skills but are also willing and confident to embrace new ways of working. The human element is as critical as the technological one in determining the success of digital transformation initiatives.
Table 4 summarizes the key challenges and considerations for implementing Unified Digital Triage.
Table 4: Key Challenges to Unified Digital Triage Implementation
Policy Landscape and Strategic Direction
The strategic direction for Unified Digital Triage (UDT) and broader digital transformation within the NHS is firmly anchored in national policies and frameworks, reflecting a concerted effort to create a more integrated and technologically advanced healthcare system.
Alignment with NHS Long Term Plan and National Digital Health Strategies
The ambition to make digitally-enabled care mainstream was articulated in the NHS Long Term Plan, published in January 2019. This vision has been significantly propelled by the COVID-19 pandemic, which demonstrated the critical role of technology and data in delivering safe patient care and enhancing communication. National policy drivers for digital transformation in 2025 include ambitious targets such as universal Electronic Patient Record (EPR) adoption, with 100% of NHS trusts expected to have a core EPR system in place by March 2025. There is also a strong emphasis on interoperability and the integration of Integrated Care Systems (ICSs).
The 'What Good Looks Like' (WGLL) programme and its associated framework serve as a crucial guide, defining digital maturity standards and building upon established best practices for digitizing, connecting, and transforming services securely. Local strategies, such as the Maidstone and Tunbridge Wells NHS Trust's (MTW) Digital and Data Strategy and the South West London ICS Digital Strategy , explicitly align with these national guidelines and the WGLL framework, ensuring consistency and coherence across the diverse NHS landscape.
Role of NHS England Digital Services for Integrated Care (DSIC) in Standardisation and Innovation
NHS England Digital Services for Integrated Care (DSIC) plays a pivotal role in driving digital transformation and integration. DSIC is tasked with improving digital products across various care settings to support and enable the integrated care system. Its core purpose is to equip healthcare professionals with digital products and services that facilitate optimal patient care, reduce administrative burdens, and offer greater value for money.
DSIC achieves this by publishing standards and capabilities that guide technology suppliers in meeting the necessary technical and clinical requirements for digital systems. It also defines rigorous assurance processes to ensure that available products and services are fit for purpose, thereby instilling confidence in buyers. Crucially, DSIC works to standardize integration methods, making it easier for different digital products and services to operate seamlessly across various healthcare settings. The DSIC model evolved from the GP IT Futures programme, recognizing the expanding range of care settings that require support and the need to drive standardization and innovation throughout the NHS. DSIC also manages the Buying Catalogue, which serves as a primary resource for commissioners to digitally select and deploy assured clinical information technology systems, simplifying procurement and reducing complexity.
Funding and Investment Priorities for Digital Transformation
Significant financial commitment underpins the NHS's digital transformation agenda. The 2024 Spring Budget, for instance, earmarked £3.4 billion for NHS technology and digital transformation in 2025/26. This substantial investment is intended to drive productivity improvements and support the Long Term Workforce Plan. Investment priorities are strategically focused on building robust infrastructure that will underpin the successful deployment of the latest technologies.
While national policy aims for coherence and universal adoption, there exists a tension between these mandates and the autonomy of individual trusts. Greater autonomy for high-performing trusts to choose their IT systems could potentially lead to further fragmentation if not carefully managed. This highlights the need for stronger national governance to mandate interchange standards and ensure alignment across the diverse NHS landscape, preventing local procurement decisions from undermining broader integration goals.
Emphasis on Universal Electronic Patient Record (EPR) Adoption and Interoperability
A core and non-negotiable goal of the NHS's digital strategy is the universal adoption of EPR systems. The aim is for all NHS trusts to have a core EPR system in place by March 2025. Furthermore, by 2024, all constituent organizations of an ICS are expected to be connected to an integrated health and care record, providing clinicians with a comprehensive view of a person's information across all care settings. This push for interoperability is viewed as a default, signifying a move beyond siloed deployments towards actively "connecting the dots" across the healthcare ecosystem. The repeated emphasis on universal EPR adoption and interoperability signifies a policy recognition that these are not just desirable but fundamental prerequisites for any advanced digital capabilities, including UDT. Without a complete, accessible, and shareable patient record, the benefits of intelligent triage, predictive analytics, and coordinated care cannot be fully realized. The success of the entire digital transformation agenda hinges on achieving these foundational data capabilities.
Case Studies and Pilot Programs: Real-World Impact
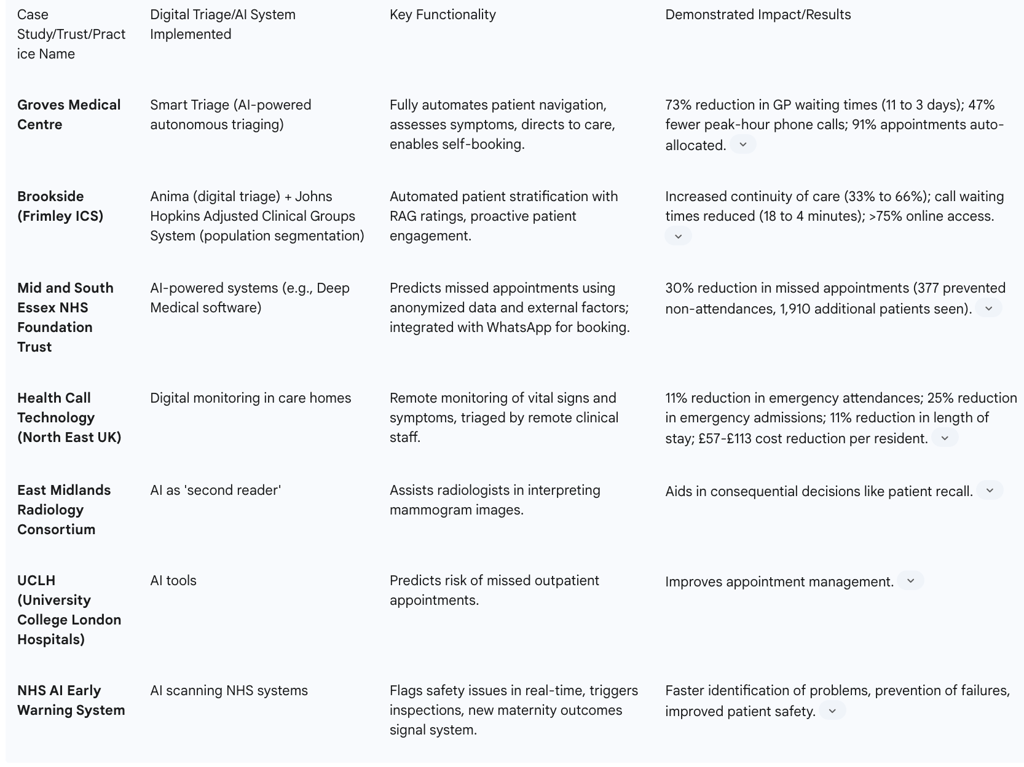
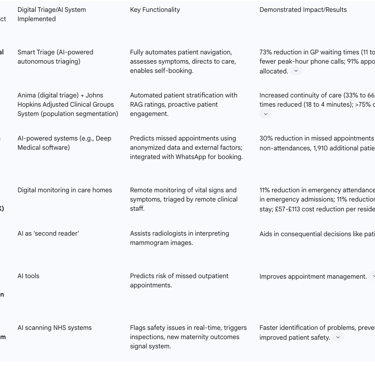
The theoretical benefits of Unified Digital Triage (UDT) and Artificial Intelligence (AI) are substantiated by a growing body of real-world implementations and pilot programs across the NHS, demonstrating tangible improvements in efficiency, patient access, and clinical outcomes. These examples provide compelling evidence of the practical application of these concepts and illustrate their potential for broader scalability.
Examples of Successful UDT and AI Implementations across NHS Trusts and Practices
Pilot programs are demonstrating clear return on investment (ROI) and the scalability of UDT.
Groves Medical Centre (Smart Triage): This practice implemented an AI-powered autonomous patient triaging system, "Smart Triage." The results were remarkable: patient waiting times for pre-bookable appointments were reduced by 73%, dropping from 11 days to just 3 days. The system also led to a 47% reduction in peak-hour phone calls and saw 91% of appointments automatically allocated without the need for staff intervention. This system fully automates the patient navigation process from the initial point of contact.
Brookside (Frimley ICS): This case study exemplifies good practice in neighborhood health. Brookside combined Anima, a digital triage platform, with the Johns Hopkins Adjusted Clinical Groups System for population segmentation. This integration enabled automated stratification of patients with RAG (red, amber, green) ratings, optimizing care prioritization. The initiative led to a significant increase in continuity of care, rising from 33% to 66% on average between April and November 2023. Furthermore, improved access through online forms, utilized by over 75% of patients, reduced average call waiting times from 18 minutes to 4 minutes.
Mid and South Essex NHS Foundation Trust: This trust utilized AI-powered systems to address missed appointments. During a six-month trial, these systems reduced missed appointments by 30%, preventing 377 non-attendances and enabling 1,910 additional patients to receive care. Deep Medical's software, for instance, predicts which patients might miss appointments by analyzing anonymized data alongside external factors such as weather patterns, traffic conditions, and work schedules.
Health Call Technology (North East UK): A digital monitoring program implemented in 118 care homes across the North East of the UK demonstrated significant benefits. This technology reduced emergency attendances by 11%, emergency admissions by 25%, and the average length of hospital stay by 11%. A retrospective analysis also showed a tangible cost reduction, increasing from £57 per resident in 2018 to £113 in 2021.
These quantifiable results move UDT beyond theoretical discussion to evidence-based efficacy. The successful implementation and evaluation of these programs suggest a clear pathway for broader adoption and justification for further investment, demonstrating the real-world impact and potential for scalability across the NHS.
Illustrative Applications of AI in Diagnostics, Appointment Management, and Patient Safety
The role of AI extends beyond simple patient triage, acting as an augmentative force that enhances human capabilities, improves accuracy, and streamlines processes across the entire care continuum. This indicates that the future of UDT is deeply intertwined with the broader adoption and sophisticated application of AI, moving towards a truly intelligent healthcare system.
Diagnostics: AI is being explored as a 'second reader' for mammogram images by the East Midlands Radiology Consortium, assisting radiologists in critical decisions. AI is also being used to detect adrenal lesions in CT scans and identify tissue growth from CT scans, potentially speeding up analysis.
Appointment Management: University College London Hospitals (UCLH) are trialling tools to predict the risk of missed outpatient appointments. Furthermore, AI tools integrated with platforms like WhatsApp allow patients to book, modify, or cancel appointments around the clock, removing accessibility barriers.
Patient Safety: A world-first AI system is being developed to scan NHS systems in real-time to flag safety issues and trigger earlier inspections. This includes a new maternity outcomes signal system set to launch across NHS trusts, which will use near real-time data to flag higher than expected rates of stillbirth, neonatal death, and brain injury.
Population Health Management: The combination of digital triage with population segmentation models, as seen at Brookside, enables the identification of high-risk patients for proactive care.
Administrative Automation: Robotic Process Automation (RPA) is being deployed to automate repetitive tasks, with a projected saving of over 500,000 staff hours by the end of 2025.
The NHS App's Expanding Role
The NHS App is increasingly central to patient empowerment and the digital transformation agenda. It allows users to view test results, manage medications, book and manage appointments, and message their GP, providing direct access to their GP health record. The App also supports carers in managing the health of their dependents and assists patients with long-term conditions in self-managing their health. The UK government highlights the NHS App as being at the heart of the planned tech transformation, envisioning AI-enabled features, links with wearable technology, and seamless access to the Single Patient Record.
Table 5 provides a summary of selected case studies, illustrating the practical impact of digital triage and AI within the NHS.
Table 5: Selected Case Studies of Digital Triage and AI in NHS
Future Outlook and Recommendations
The trajectory of NHS Integrated Care, powered by Unified Digital Triage (UDT) and advanced digital technologies, points towards a transformative future for healthcare delivery. This future is characterized by a fundamental shift from reactive treatment to proactive, personalized health management, ultimately aiming to extend not just lifespan but also "health span"—the period of life spent in good health.
Emerging Technologies and Their Potential
The continuous evolution of technology promises to further enhance the capabilities of integrated care and digital triage. There is an anticipated expansion of remote monitoring tools, AI "bots," and generative AI to support both clinical and operational decision-making. Remote Patient Monitoring (RPM) is already demonstrating its value by collecting and analyzing patient-generated health data for individuals with chronic and acute conditions, informing treatment plans and goal setting.
Ambient AI, a location- or task-specific AI capability, holds significant potential to streamline clinical documentation and enhance clinician-patient interactions, allowing healthcare providers to dedicate more time to direct patient engagement. The broader integration of big data, AI, and smart systems is expected to facilitate more informed decisions, efficient service allocation, and timely identification of potential risks through continuous monitoring. The NHS Federated Data Platform (FDP) is a crucial component in this vision, designed to gather real-time data on quality and enable coordinated decision-making across diverse care settings. This indicates that the future of integrated care, powered by UDT and AI, is fundamentally about moving upstream in the healthcare journey, anticipating needs, and intervening early to improve population health, rather than solely reacting to illness. This implies a significant reorientation of resources and care models.
Long-Term Impact on Healthcare Delivery and Patient Outcomes
The long-term impact of UDT within NHS Integrated Care is envisioned as the creation of a seamless continuum of care. Within this model, patients receive aligned support without clear demarcations between different parts of the system, ensuring holistic care regardless of the specific provider. The overarching goal is to extend not just lifespan but also "health span" through data-driven, personalized interventions. This combined impact of unified records, data lakes, predictive AI, and remote monitoring points to a future where healthcare is not a series of episodic interventions but a continuous, personalized journey. This implies a fundamental shift in the relationship between individuals and the healthcare system, moving towards continuous health management and preventative interventions tailored to individual needs.
AI-enabled systems are poised to augment human decision-making, providing invaluable support to overstretched teams by flagging at-risk patients, suggesting treatment options, and predicting demand. This augmentation allows healthcare professionals to focus on complex clinical judgments while routine or high-volume tasks are intelligently managed by technology.
Strategic Imperatives for Successful Scaling and Sustainability
To successfully scale and sustain the benefits of UDT and digital transformation, several strategic imperatives must be addressed:
Embed and Innovate: Once core digital infrastructure is established, trusts must shift their focus to fostering innovation on top of this foundation. This involves continuous exploration and adoption of new technologies that build upon existing capabilities.
Interoperability as Default: Moving beyond fragmented, siloed deployments, achieving true interoperability must become the default. The year 2025 is highlighted as a critical period for "connecting the dots" across the system.
Workforce Development: Sustained investment in developing and enhancing the skills of the healthcare workforce is crucial to keep pace with technological innovations. This includes improving digital literacy across all staff levels and fostering a culture of continuous learning.
Co-production: New digital solutions must be developed in collaboration with both citizens and staff. This co-production approach ensures that technology genuinely meets the needs of the population and is accessible to all, promoting user adoption and satisfaction.
Robust Governance: Implementing robust governance frameworks for AI tools is essential, with a strong focus on ethical application, transparency, and rigorous measurement of their value in patient outcomes.
Sustained Investment: Delivering the ambitious goals of digital transformation requires sustained and strategic investment, exploring various funding models, including cloud-hosted solutions and managed services for cost efficiency.
Recommendations for Policy, Investment, Technology Development, and Workforce Development
Based on the analysis, the following recommendations are proposed to ensure the continued success and expansion of Unified Digital Triage within NHS Integrated Care:
Policy: It is imperative for national policy to mandate strict interoperability standards to overcome the fragmentation caused by disparate IT systems and local autonomy in procurement. Policy should also prioritize sustained funding for foundational digital infrastructure, recognizing it as the bedrock for all advanced digital capabilities.
Investment: Continued, strategic investment in core digital capabilities, such as Electronic Patient Records (EPRs) and shared care records, must precede or run in parallel with the scaling of advanced AI applications. Exploring cloud-hosted solutions and managed services can offer significant cost efficiencies and scalability benefits.
Technology Development: Future technology development should prioritize user-centric design, ensuring that systems are intuitive, easy to navigate, and accessible to all users, regardless of their digital literacy. Emphasis should be placed on AI development that augments human decision-making and demonstrably reduces administrative burdens, rather than seeking to replace clinical expertise.
Workforce Development: Comprehensive training programs are essential to improve digital literacy across all staff levels within the NHS. Fostering a culture of continuous learning and adaptation to new technologies is critical. Strategies to address resistance to change should involve effective communication, early engagement, and active involvement of staff in the design and implementation processes.
Ethics & Trust: Develop and enforce clear ethical guidelines and robust governance frameworks for AI deployment. This includes ensuring transparency in AI decision-making processes, establishing clear accountability mechanisms, and prioritizing patient safety. Proactive communication about AI's role, benefits, and limitations is necessary to build and maintain trust among both healthcare professionals and patients.
Conclusion
Unified Digital Triage (UDT) is unequivocally a critical enabler for the successful realization of NHS Integrated Care Systems. It offers a powerful pathway to address long-standing challenges of service fragmentation, significantly improve operational efficiency, enhance the patient experience, and optimize resource utilization across the healthcare landscape. The evidence from various pilot programs and strategic initiatives demonstrates tangible benefits, from drastically reduced waiting times and improved access to substantial cost savings and enhanced patient safety.
The journey towards a fully integrated, digitally-enabled NHS is complex and multifaceted, requiring sustained commitment across policy, technology, and workforce domains. Overcoming entrenched challenges such as data interoperability, ensuring digital inclusion for all segments of the population, and building profound trust in AI-based systems will be paramount. However, the demonstrated benefits, coupled with the clear strategic alignment with national healthcare goals, underscore that UDT is not merely an optional enhancement but an indispensable component in constructing a more responsive, proactive, and patient-centered healthcare system for the future. The continued strategic investment in digital foundations, coupled with a human-centric approach to technological adoption, will be key to unlocking the full transformative potential of integrated care in the NHS.
FAQ Section
Here are ten frequently asked questions about NHS Integrated Care Systems and unified digital triage:
What are NHS Integrated Care Systems (ICSs)? NHS Integrated Care Systems (ICSs) are partnerships of organizations that come together to plan and deliver joined-up health and care services for a defined geographical area. Formally established in July 2022 through the Health and Care Act, ICSs bring together NHS providers, commissioners, local authorities, and other stakeholders to improve population health, reduce inequalities, enhance quality of care, and achieve better value.
What is unified digital triage in the NHS context? Unified digital triage in the NHS context refers to standardized, technology-enabled approaches to patient assessment and routing that work consistently across organizational boundaries within an Integrated Care System. These platforms create single points of entry to multiple services, using consistent protocols to direct patients to the most appropriate care setting based on clinical need, urgency, and service availability.
How do unified triage systems differ from traditional NHS triage approaches? Traditional NHS triage approaches were service-specific, with each entry point (GP practices, A&E, mental health, community services) using different assessment criteria and processes. Unified triage systems provide consistent front doors to care regardless of entry point, use standardized protocols across service boundaries, incorporate data sharing to prevent duplicate assessments, and dynamically route patients based on both clinical need and system capacity.
What governance structures are needed for implementing unified triage in an ICS? Effective governance for unified triage typically includes a clinically-led design authority with multi-professional representation from across the ICS, clear data sharing agreements between constituent organizations, operational oversight groups to monitor performance and address issues, and user representation to ensure patient perspectives inform decision-making. Most successful models balance system-wide standards with appropriate place-based flexibility.
How do ICSs address digital exclusion in their unified triage approaches? ICSs address digital exclusion through multi-channel access maintaining telephone and in-person options alongside digital routes, assisted digital support services providing hands-on help, community access points in trusted locations like libraries and community centers, device loan schemes for those without technology access, and targeted interventions for specific excluded groups such as language adaptations, accessibility features, and outreach programs.
What measurable outcomes have been achieved through unified digital triage in ICSs? Documented outcomes include 20-30% reductions in low-acuity A&E attendances, 25-40% decreases in assessment duplication across services, 15-30% improvements in appropriate service utilization, significant reductions in patient journey times from first contact to definitive care, and substantial improvements in patient-reported satisfaction with care navigation experiences.
How does unified digital triage integrate with existing NHS technical infrastructure? Integration typically occurs through connections with shared care records to access patient history, links to service directories and capacity management systems for real-time routing, integration with existing booking systems for seamless appointments, interfaces with NHS 111 and 999 infrastructure, and connections to population health management platforms to inform triage algorithm refinement with outcome data.
What implementation models are used for unified triage across different ICSs? Implementation models include centralized approaches with single ICS-wide platforms and standardized protocols, federated models that maintain local triage systems while establishing shared standards and interoperability, and hybrid approaches that combine elements of both, typically with centralized models for specific care domains and federated approaches for others. The choice depends on local context, existing digital maturity, and governance preferences.
How does unified digital triage contribute to reducing health inequalities? Unified triage addresses inequalities through systematic identification of social vulnerability factors during assessment, culturally adapted interfaces and content for diverse communities, proactive outreach to traditionally underserved populations, integration of social prescribing and community support into routing options, and continuous equity monitoring to identify and address disparities in access patterns or service allocation.
What role do place-based partnerships play in unified digital triage? Place-based partnerships typically lead local implementation of unified triage, adapting system-wide standards to local service configurations and population needs. They provide crucial local intelligence about service capacity and referral pathways, engage local clinical and community stakeholders in protocol development, monitor outcomes from a place perspective, and connect triage systems to locality-based care coordination functions.
Additional Resources
For readers interested in exploring NHS Integrated Care Systems and unified digital triage further, the following resources provide valuable insights:
"Integrated Care Systems: Design Framework" by NHS England - The official guidance document outlining the core components, governance structures, and operational principles for Integrated Care Systems, providing essential context for understanding the organizational framework within which unified triage operates.
"Digital Clinical Safety Strategy" by NHSX and NHS Digital - A comprehensive framework for ensuring patient safety in digital health implementations, with specific sections addressing risk management in algorithmic decision support and triage systems that span organizational boundaries.
"Reducing Health Inequalities Through Digital Inclusion" by the NHS Confederation - A practical guide addressing approaches to ensuring digital healthcare innovations reach all population groups, with case studies highlighting successful models for inclusive implementation of digital front doors to care.
Journal of Integrated Care Special Issue on Digital Integration - A collection of peer-reviewed academic articles examining various aspects of digital transformation within integrated care systems, including several studies specifically focused on unified assessment and navigation approaches.
"Place-Based Partnerships for Integrated Care: Implementation Guide" by The King's Fund - A detailed exploration of how place-based collaboration operates within the ICS framework, providing valuable context for understanding the organizational dynamics influencing unified triage implementation.
