Mastering the Emergency Severity Index (ESI)
An in-depth exploration of the Emergency Severity Index (ESI) triage system, including its history, implementation, challenges, and best practices for emergency healthcare providers.


The Emergency Severity Index (ESI) is a cornerstone of modern emergency department (ED) operations, functioning as a five-level triage algorithm. It provides a clinically relevant method for stratifying patients into five distinct groups, ranging from ESI Level 1 (most urgent) to ESI Level 5 (least urgent), based on a dual assessment of patient acuity and anticipated resource needs. As a standardized tool, the ESI aims to bring consistency and objectivity to the critical initial patient assessment process in the ED. The fundamental purpose of any triage system is to rapidly evaluate all incoming emergency patients, enabling clinical assessors to prioritize care based on the severity and acuity of illness. This prioritization dictates the selection of necessary interventions and treatments, a process indispensable for the seamless operation of busy EDs, particularly when managing high patient volumes or resource limitations.
The ESI's unique contribution lies in its explicit incorporation of resource needs for stable patients, differentiating it from systems focused solely on acuity. This means the ESI not only identifies patients requiring immediate, life-saving care but also predicts the intensity of ED services that stable patients will consume. Consequently, the ESI functions as an initial gatekeeper for ED resources, influencing the allocation of staff time, diagnostic tests, and treatment spaces from the moment a patient arrives. Accurate ESI assignment is therefore critical not only for individual patient safety but also for overall departmental efficiency and effective resource management. Misapplication can lead to inefficient resource utilization, potentially delaying care for other patients and impacting the ED's capacity to manage patient flow.
1.2. Historical Development and Evolution (AHRQ, ENA)
The conceptual foundation of the ESI was laid in 1998 by emergency physicians Dr. Richard Wuerz and Dr. David Eitel. Recognizing the need for a more standardized and effective triage system, their initial work received funding from the Agency for Healthcare Research and Quality (AHRQ), underscoring its importance from a healthcare quality and research standpoint. Following promising pilot testing, the ESI was first implemented in two university teaching hospitals in 1999. It was subsequently refined based on feedback and implemented in five additional hospitals in 2000. This iterative development involved a collaborative ESI Triage Group, comprising emergency nursing and medical clinicians, managers, educators, and researchers, ensuring the tool was honed through diverse expertise and real-world clinical practice.
The ESI is currently maintained by the Emergency Nurses Association (ENA), highlighting its integral role in contemporary emergency nursing practice and ongoing professional education. The widespread adoption of the ESI, with approximately 94% of United States EDs utilizing the algorithm as of 2019, signifies its status as the de facto standard in the U.S. This prevalence underscores the necessity for emergency clinicians to achieve mastery of the system. The development and broad acceptance of the ESI reflect a significant shift in emergency medicine from purely subjective or institution-specific triage methods towards standardized protocols. This standardization aims to enhance consistency in patient assessment, reduce inter-rater variability, and improve patient safety and operational efficiency. While clinical experience remains highly valued in triage , the ESI framework encourages the integration of this experience within a structured, evidence-based algorithm. This approach not only supports quality care but also facilitates research, inter-institutional quality comparisons, and the mobility of clinical staff.
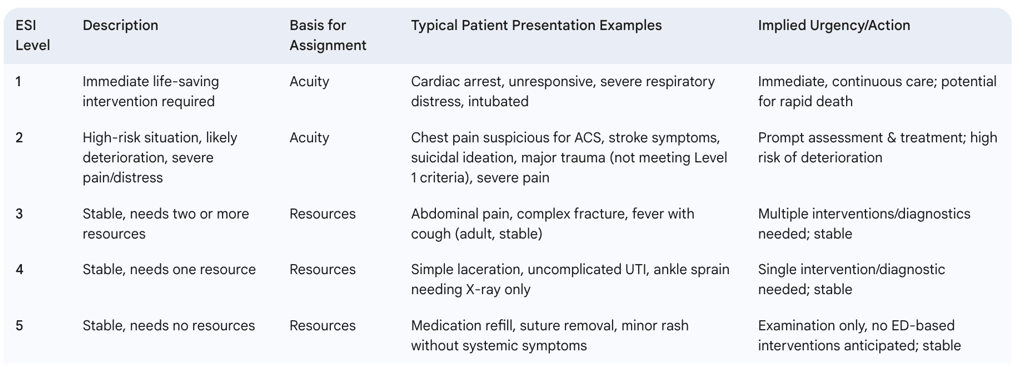
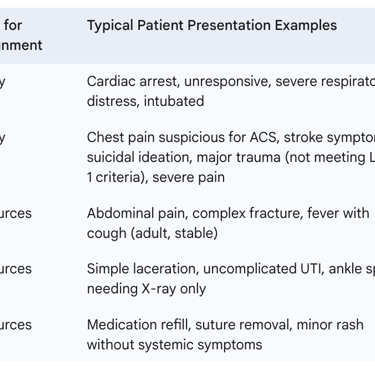
1.3. Overview of the Five ESI Levels: From Most Urgent (Level 1) to Least Urgent (Level 5)
The ESI categorizes patients into one of five levels, with Level 1 representing the highest urgency and Level 5 the lowest. A critical aspect of the ESI framework is that the basis for level assignment shifts: Levels 1 and 2 are determined by patient acuity (the severity of their condition and risk of deterioration), whereas Levels 3, 4, and 5 are determined by the anticipated number of resources required for the care of stable patients.
ESI Level 1: Assigned to patients requiring immediate, life-saving intervention without delay. These are individuals with an imminent threat to life or limb, such as those in cardiac arrest, unresponsive patients, or those with profound hypotension or hypoglycemia. Intervention, like cardiopulmonary resuscitation (CPR), is needed instantly.
ESI Level 2: Assigned to patients who are at high risk of deterioration or exhibit signs of a time-critical problem. While not requiring immediate life-saving measures like Level 1 patients, they are unstable or potentially unstable and need urgent attention to prevent worsening. Examples include patients with cardiac-related chest pain, acute asthma attacks, or significantly altered mental status. These patients should effectively "skip the line" for prompt assessment and treatment.
ESI Level 3: Assigned to stable patients who are predicted to require two or more resources to achieve a disposition (e.g., admission, discharge, transfer). Common examples include patients presenting with uncomplicated abdominal pain (requiring labs and imaging), a high fever with a productive cough, or a persistent headache needing diagnostic evaluation.
ESI Level 4: Assigned to stable patients who are predicted to require only one type of resource. Examples include patients with a simple laceration needing sutures, those requiring a rabies vaccination, or individuals with flu-like symptoms who may only need a diagnostic swab.
ESI Level 5: Assigned to stable patients who are predicted to require no ED resources beyond a basic examination and assessment. A classic example is a patient seeking a medication refill.
This dual-axis prioritization—acuity for Levels 1 and 2, and resource intensity for Levels 3, 4, and 5—makes the ESI a sophisticated operational tool. It moves beyond a simple linear scale of "sickness" to address two critical ED demands: managing immediate life threats and efficiently processing the overall patient load. For instance, a patient with a complex, angulated fracture might not be critically ill (thus not ESI 1 or 2) but would be an ESI 3 due to the need for multiple resources (e.g., X-rays, potent analgesia, procedural sedation, reduction, splinting). This patient significantly impacts ED flow and resource allocation, differently from an ESI 5 patient or even some ESI 2 patients who might be stabilized and discharged relatively quickly. Understanding this dual nature is fundamental to mastering ESI and appreciating its impact on ED operations, resource planning, and patient throughput.
Table 1: ESI Levels at a Glance
2. The ESI Triage Algorithm: A Step-by-Step Guide
2.1. The Conceptual Framework: Acuity vs. Resource-Based Decisions
The ESI algorithm is structured with a clear conceptual hierarchy: it first mandates an assessment of patient acuity to identify those requiring ESI Level 1 or Level 2 designation. Only after a patient is deemed stable and not meeting criteria for these high-acuity levels does the algorithm shift to predicting the number of resources needed to assign an ESI Level of 3, 4, or 5. This bifurcated logic ensures a "safety-first" approach. The algorithm compels the triage clinician to systematically rule out immediate life threats and high-risk conditions before considering the anticipated workload for stable patients.
This sequential decision-making process is fundamental to the ESI's design and reflects a core principle of emergency medicine: "rule-out worst-case first." The algorithm structurally prioritizes the rapid identification and categorization of the most critically ill or vulnerable patients. The more detailed, and potentially more time-consuming, process of resource prediction for less acute individuals is deliberately deferred until patient stability is reasonably assured. Triage nurses must internalize this flow. Attempting to count resources before definitively evaluating for ESI Level 1 or 2 criteria constitutes a deviation from the algorithm's intended application and carries the risk of dangerous under-triage. Strict adherence to this sequence is paramount for accurate and safe ESI assignment.
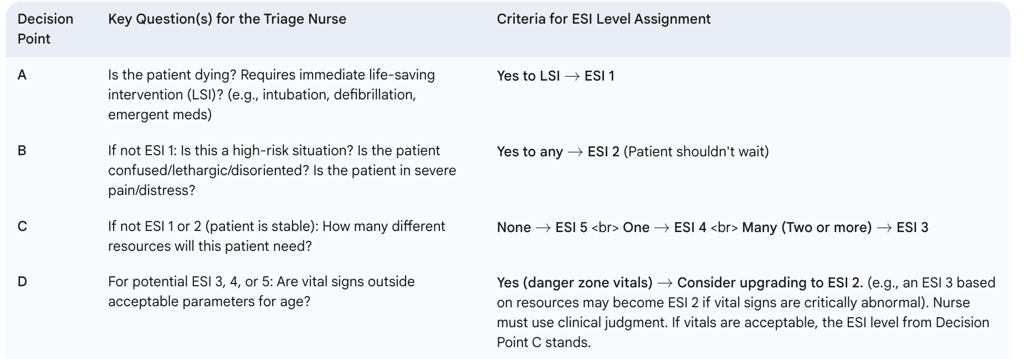
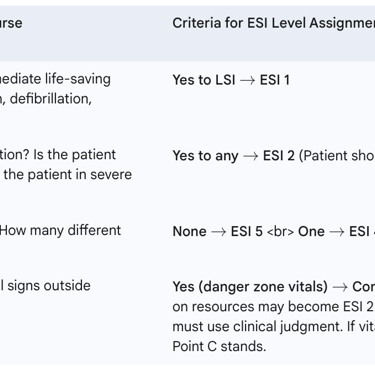
2.2. Detailed Breakdown of the Four Key Decision Points (A, B, C, D)
The ESI algorithm employs a maximum of four key decision points (A, B, C, and D) to systematically sort patients into one of the five triage levels. It is important to note that not all patients will proceed through all four decision points; higher acuity patients may be assigned an ESI level after only one or two decisions.
Decision Point A: Immediate Life-Saving Intervention Needed? (Assigns ESI Level 1) The first and most critical question the triage nurse must address is: "Is the patient unstable or does this patient require immediate life-saving intervention?". If the answer is "yes," the patient is immediately assigned ESI Level 1. This determination is based on findings indicating profound instability, such as unresponsiveness, an active seizure, airway obstruction, or evidence of ineffective gas exchange or perfusion. Life-saving interventions are those actions necessary to prevent imminent death or major disability, including but not limited to cardiopulmonary resuscitation (CPR), emergency intubation, defibrillation, external cardiac pacing, immediate administration of blood products, or emergent medications such as dopamine, epinephrine, or naloxone for opioid overdose. The focus here is on conditions requiring interventions within minutes to sustain life.
Decision Point B: High-Risk Situation, Likely Deterioration, or Severe Pain/Distress? (Assigns ESI Level 2) If the patient does not meet ESI Level 1 criteria (i.e., does not require immediate life-saving intervention), the triage nurse proceeds to Decision Point B. Here, the key questions are: "Is this a high-risk situation?" "Is the patient likely to deteriorate?" "Are there signs of a time-critical problem?" or "Is the patient in severe pain or distress?". A "yes" to any of these questions leads to an ESI Level 2 assignment. This decision point captures patients who, while not imminently dying, have conditions that could rapidly worsen or necessitate time-sensitive treatment to prevent significant morbidity. Examples include patients presenting with cardiac-related chest pain not requiring immediate intervention, new neurological deficits suggestive of a stroke (but not meeting Level 1 criteria like unresponsiveness), an immunocompromised patient with a fever, or a patient who is actively suicidal or homicidal. Severe pain or distress, whether physiological or psychological, is also a criterion for ESI Level 2, as it indicates a significant burden on the patient that requires prompt attention. This decision point demands considerable clinical judgment, pattern recognition, and an understanding of disease progression.
Decision Point C: Resource Prediction (Assigns ESI Levels 3, 4, or 5) If a patient does not meet the criteria for ESI Level 1 or Level 2, they are considered stable and at low risk of immediate deterioration. At this juncture, Decision Point C comes into play: "How many different types of resources are anticipated to be used to reach a disposition for this patient?". The assignment is based on this prediction:
Two or more resources predicted leads to an ESI Level 3 assignment.
One resource predicted leads to an ESI Level 4 assignment.
Zero resources predicted leads to an ESI Level 5 assignment. This is where the ESI's unique resource-prediction component is applied for stable patients. It requires the triage nurse to draw upon their experience and knowledge of typical care pathways for various presenting complaints to anticipate the ED services the patient will likely require.
Decision Point D: Vital Signs Assessment and Impact on Acuity The final decision point, D, involves assessing the patient's vital signs: "Do the patient's vital signs support changing their acuity level?". This is particularly crucial for patients provisionally triaged to ESI Levels 3, 4, or 5 based on resource prediction. A full set of vital signs—including heart rate, respiratory rate, and, for patients with potential respiratory compromise, oxygen saturation—must be obtained and considered before finalizing an ESI Level 3, 4, or 5. Temperature and blood pressure are also typically included. Vital signs serve as an objective safety net. Abnormal vital signs (e.g., significant tachycardia, tachypnea, hypoxia, hypotension, or hypertension in certain contexts) may indicate underlying instability not immediately apparent from the patient's general appearance or initial complaint. If dangerous vital signs are present, a patient initially considered ESI 3, 4, or 5 based on resource needs may be up-triaged to ESI Level 2. This decision point underscores that resource prediction for stable patients should not overshadow objective physiological data indicating potential risk.
The ESI algorithm is not a purely mechanical checklist; rather, it is a framework designed to guide and structure clinical judgment. While Decision Points A (life-saving interventions) and D (vital signs) rely on more objective criteria (e.g., apnea, specific vital sign thresholds), Decision Point B (high-risk assessment) and Decision Point C (resource prediction) inherently involve a greater degree of subjective clinical assessment. Questions like "Is the patient likely to deteriorate?" or predicting resources based on "previous patients with similar presentations" require clinical experience, pattern recognition, and nuanced interpretation. This blend of objective data points with experience-based predictions is why the ESI is recommended for use by experienced ED nurses who have undergone specific ESI training , and why training programs often emphasize case-based learning. Mastery of ESI involves developing the clinical acumen to apply the algorithm effectively across a spectrum of patient presentations, understanding that the algorithm provides the "what," but the clinician's expertise often determines the "how well." This also helps to explain why inter-rater reliability can vary, particularly between clinicians with different levels of experience.
Table 2: ESI Decision Points and Key Questions
2.3. The Role of Clinical Judgment and Experience
The ESI algorithm is explicitly designed to be utilized by healthcare professionals who possess both clinical experience in the emergency setting and specific training in the ESI methodology. The ESI handbook states that its use should be restricted to individuals with at least one year of ED experience who have completed a comprehensive triage education program. This prerequisite underscores that the ESI is not a simplistic checklist suitable for novice practitioners without a foundational understanding of emergency patient presentations and care pathways.
The nuances inherent in several decision points, particularly Decision Point B (assessing "high-risk" situations) and Decision Point C (predicting resource utilization), demand a level of pattern recognition and clinical intuition that is typically honed through experience. For example, determining if a patient is "likely to deteriorate" or accurately forecasting the number of distinct resource categories a patient will require based on their presenting complaint often involves drawing upon past encounters with similar patients.
It is also acknowledged that the initial ESI level assigned at triage is a snapshot in time and may be subject to revision as more information becomes available or as the patient's condition evolves. As one source notes, it is not uncommon for a patient initially triaged as ESI Level 3 to be reclassified as ESI Level 2 upon more detailed evaluation by the clinical team. This highlights that triage is an initial sorting process, and the ESI level is a dynamic assessment point rather than a definitive, immutable diagnosis.
Crucially, while the ESI provides a standardized framework, it does not supplant the overarching professional responsibility and clinical judgment of the healthcare provider. Each clinician applying the ESI algorithm does so based on their professional assessment of the specific patient before them. This balance is critical; the ESI is a tool to guide and structure decision-making, not to replace critical thinking.
The ESI system functions as a "guided estimation" tool. It relies on the clinician's ability to estimate urgency and resource needs at a particular point in time, framed by the algorithm's structure. The accuracy of these estimations is inherently linked to the clinician's skill and experience. Therefore, over-reliance on the ESI level as a definitive label without ongoing reassessment and clinical vigilance can be problematic. It serves as a crucial starting point for patient prioritization and resource allocation, but it is not an infallible diagnostic or prognostic instrument. This understanding also explains why ESI performance can demonstrate variability and why robust quality assurance measures are essential for its effective implementation.
3. Defining and Quantifying "Resources" in ESI
A distinctive feature of the Emergency Severity Index, particularly for determining ESI Levels 3, 4, and 5 for stable patients, is its reliance on the prediction of "resources." Understanding what constitutes a resource according to ESI guidelines is paramount for its accurate application.
3.1. Official ESI Guidelines on What Constitutes a Resource
According to the ESI algorithm, a "resource" is defined as a type of intervention or diagnostic tool that goes beyond a basic physical examination performed by the physician or advanced practice provider, and the initial nursing assessment including vital signs. It signifies an activity or service provided in the ED that contributes to determining the patient's disposition.
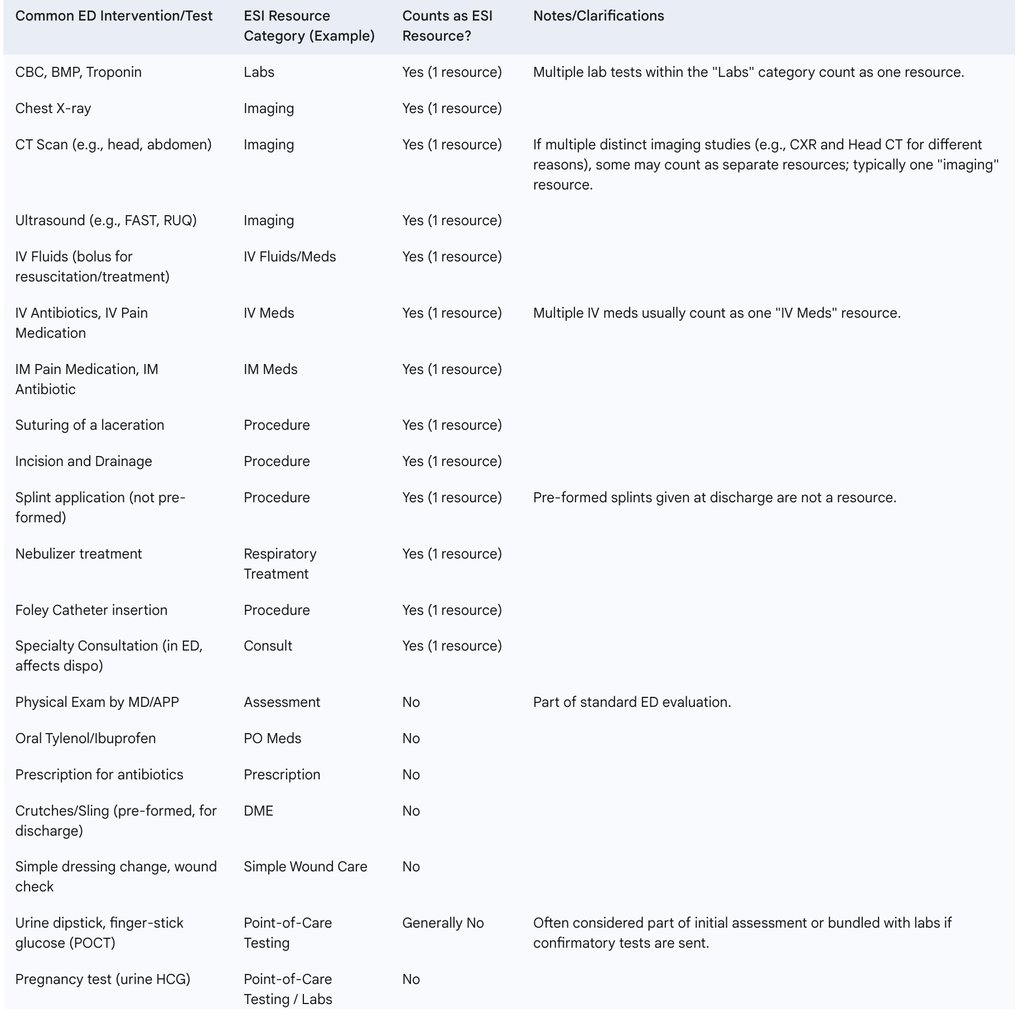
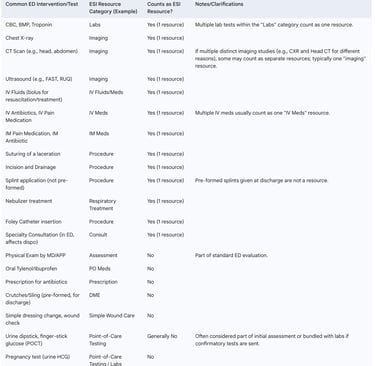
Examples of interventions or diagnostics that are considered resources include :
Laboratory studies: Blood tests (e.g., CBC, chemistry panel, cardiac markers), urine tests (e.g., urinalysis, urine culture), coags.
Diagnostic imaging: X-rays, CT scans, ultrasound examinations.
Intravenous (IV) or Intramuscular (IM) medications: Administration of medications via these routes (excluding routine immunizations in some contexts, but including therapeutic injections).
IV fluids: For hydration or as a vehicle for medication.
Specialty consultation: Formal consultation requested from a specialist (e.g., cardiology, surgery, neurology) that occurs in the ED and influences disposition.
Procedures: Such as suturing of lacerations, incision and drainage, foreign body removal, splint application (not pre-formed), Foley catheter insertion, or nasogastric tube placement.
Respiratory support: Such as nebulizer treatments or initiation of BiPAP/CPAP (though initiation of BiPAP/CPAP may also push a patient into ESI 2 territory depending on the overall clinical picture and stability).
Providing these concrete examples is essential for triage nurses to develop a consistent understanding and application of resource counting.
3.2. Items Specifically Not Considered Resources
Equally important as knowing what counts as a resource is understanding what is explicitly excluded. Miscounting these items can lead to inappropriate up-triage of stable patients (e.g., assigning an ESI Level 4 when the patient truly requires no resources and should be an ESI Level 5).
Items specifically not considered resources by the ESI algorithm include :
History and Physical Examination (H&P): The initial assessment by the physician or provider.
Point-of-care testing (POCT): Simple tests like a finger-stick glucose, urine dipstick, or a rapid strep test are generally not counted as separate resources if they are part of the initial assessment or a broader lab workup. However, interpretation may vary, and local institutional guidelines should be consulted. Some sources suggest pregnancy tests are not resources.
Oral medications (PO meds): Administering medications by mouth.
Saline lock, heparin lock, or IV Drip (maintenance fluids only): If an IV line is placed but no IV medications or bolus fluids for resuscitation are given.
Simple wound care: Such as cleaning a wound or applying a simple dressing (e.g., Steri-Strips, Dermabond for very minor wounds not requiring formal suturing), or dressing changes.
Crutches, slings, splints (pre-formed or off-the-shelf): Providing durable medical equipment for home use.
Prescriptions: Writing prescriptions for medications to be filled outside the ED.
Phone call to a primary care physician or specialist for advice (not a formal consult influencing ED disposition).
Social work or case management intervention (generally, unless it's a complex intervention directly leading to disposition).
3.3. Nuances in Resource Counting
A critical nuance in applying the ESI resource criteria is that resources are generally counted by category, not by the sheer number of individual tests or interventions within that category. For instance, if a patient requires multiple blood tests (e.g., a complete blood count, a basic metabolic panel, and cardiac enzymes), these collectively count as one "laboratory" resource. Similarly, if a patient needs both a chest X-ray and a CT scan of the head, this would typically count as one "imaging" resource, although some interpretations might count them as two if they are significantly distinct studies addressing different problems. However, the prevailing guidance leans towards categorical counting to prevent over-inflation of resource use for patients needing a battery of tests within the same domain. If a patient needed labs (one resource) and an X-ray (a second resource category), this would correctly be counted as two resources.
This categorical approach suggests that resource counting in ESI Levels 3-5 serves as a proxy for the complexity and breadth of the ED services a patient will engage, rather than simply tallying every single task performed. It reflects the number of different types of ED service pathways the patient will require. A patient needing only laboratory work (one resource category, ESI 4) has a less complex ED trajectory than a patient needing laboratory work, diagnostic imaging, and IV medications (three resource categories, ESI 3). Understanding this principle is key to consistently differentiating between ESI Level 3 and ESI Level 4 for stable patients and ensuring accurate application of the algorithm.
Table 3: ESI Resource Categorization Examples
4. Applying ESI: Clinical Scenarios and Case Studies
Abstract knowledge of the ESI algorithm and its decision points is insufficient for achieving true mastery. Clinical proficiency is developed through the application of these concepts to realistic patient scenarios. Authoritative resources such as the ESI Implementation Handbook (Version 4 from AHRQ, now the 5th Edition from ENA) and ENA-sponsored online courses provide numerous case studies for practice and competency assessment. Analyzing these cases allows clinicians to understand how the theoretical framework translates into practical decision-making.
4.1. Illustrative Case Studies for Each ESI Level
The following examples, drawn from or consistent with provided research, illustrate ESI assignment:
ESI Level 1 Scenario (Opioid Overdose): A patient arrives unresponsive, with a respiratory rate of 6 breaths per minute and pinpoint pupils.
Decision A (Life-Saving Intervention?): Yes. The patient is apneic/bradypneic and unresponsive, likely requiring immediate airway management and administration of naloxone. This is an ESI Level 1.
ESI Level 2 Scenario (Chest Pain, High-Risk): A 55-year-old male presents with severe chest pain (9/10) radiating to the jaw, accompanied by diaphoresis. Vital signs: respiratory rate 22, blood pressure 160/95 mmHg.
Decision A (Life-Saving Intervention?): No. While serious, the patient is conscious and maintaining their airway; interventions are not immediately required to prevent death within minutes.
Decision B (High-Risk?): Yes. This presentation is highly suspicious for an Acute Coronary Syndrome (ACS), a time-critical condition with a high risk of deterioration. This is an ESI Level 2.
ESI Level 2 Scenario (Immunocompromised Patient with Fever): A 70-year-old female actively undergoing chemotherapy presents with confusion, lethargy, and a fever of 38.9∘C (102∘F).
Decision A (Life-Saving Intervention?): No.
Decision B (High-Risk?): Yes. An immunocompromised patient with fever and altered mental status is at high risk for severe sepsis or other life-threatening infection. This is an ESI Level 2.
ESI Level 3 Scenario (Abdominal Pain, Stable): A 30-year-old female presents with right lower quadrant abdominal pain and nausea for one day. Vital signs are stable, and pain is rated 6/10.
Decision A (Life-Saving Intervention?): No.
Decision B (High-Risk?): No. The patient is currently stable, and the presentation does not immediately suggest a high-risk condition or severe distress warranting ESI 2.
Decision C (Resources?): Yes. This patient will likely require laboratory studies (e.g., CBC, pregnancy test) and diagnostic imaging (e.g., ultrasound or CT scan). This constitutes two or more resource categories. This is an ESI Level 3.
Decision D (Vitals?): Assuming vital signs are within normal limits for age and do not suggest instability, the ESI 3 assignment stands.
ESI Level 4 Scenario (Simple Laceration): A patient presents with a 2 cm simple laceration on the forearm, hemodynamically stable, with no other complaints.
Decision A (Life-Saving Intervention?): No.
Decision B (High-Risk?): No.
Decision C (Resources?): Yes. The patient will likely require sutures (a procedure). This is one resource. This is an ESI Level 4.
Decision D (Vitals?): Assuming stable vital signs, the ESI 4 assignment stands.
ESI Level 5 Scenario (Medication Refill): A patient presents requesting a refill for their blood pressure medication as they have run out. They are asymptomatic and report good blood pressure control.
Decision A (Life-Saving Intervention?): No.
Decision B (High-Risk?): No.
Decision C (Resources?): No. This patient is anticipated to require only a history and physical (not a resource) and a prescription (not a resource). This is an ESI Level 5.
Decision D (Vitals?): Vital signs should be checked. Assuming they are normal, the ESI 5 assignment stands.
4.2. Demonstrating the Decision-Making Process in Practice
Working through diverse clinical presentations using the ESI algorithm reveals the interplay between its structured, scientific framework and the "art" of clinical judgment. While the algorithm provides clear decision points , applying them effectively often requires nuanced interpretation. For example, determining if a situation is "high-risk" (Decision Point B) or accurately predicting the number of resources a stable patient will need (Decision Point C) is not always a black-and-white determination and relies heavily on the triage nurse's experience and pattern recognition abilities.
Case studies are essential because they bridge the gap between theoretical knowledge of the ESI rules and the practical skill of applying them in complex, often ambiguous, real-world situations. It is through repeated application to varied scenarios that clinicians hone their ability to integrate objective ESI criteria with their clinical intuition and experience. This practice is crucial for developing pattern recognition and confidence in navigating the grey areas inherent in emergency triage. This is a key reason why ENA training materials and the ESI handbook heavily feature case examples and competency assessments. The process of systematically applying Decision Points A through D to each case, verbalizing the rationale, and comparing outcomes with expert consensus is fundamental to achieving mastery.
5. Special Populations: Adapting ESI for Diverse Needs
While the ESI provides a standardized framework, its application requires adaptation and special consideration for certain patient populations whose physiological responses, presentations of illness, and communication abilities differ from the average adult.
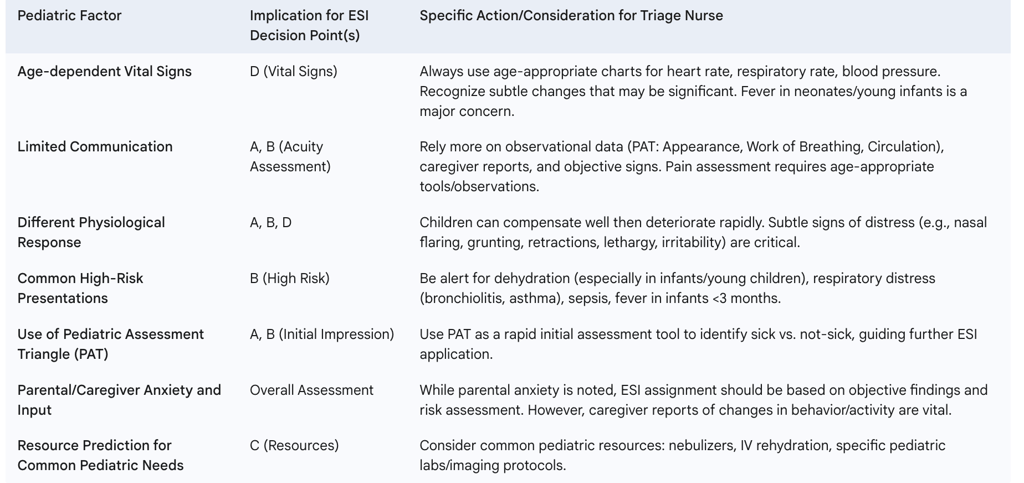
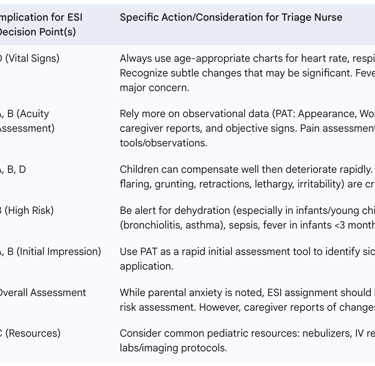
5.1. Pediatric Patients
Pediatric patients are not simply "small adults" and necessitate specific considerations when applying the ESI algorithm. The ESI Triage Tool Implementation Handbook (Version 4, 2012 edition, and subsequent ENA versions) includes a dedicated pediatric chapter, developed in response to validation research and requests for more detailed guidance. The ESI should be used in conjunction with tools like the Pediatric Assessment Triangle (PAT – assessing Appearance, Work of Breathing, and Circulation to Skin) and a focused pediatric history to accurately assign an acuity level.
Unique Challenges in Pediatric Triage: Children exhibit different physiological and psychological responses to stressors compared to adults. They are more susceptible to certain conditions like viral illnesses leading to rapid dehydration, and their limited ability to communicate symptoms clearly makes accurate and rapid assessment more challenging.
ESI Algorithm Considerations for Pediatrics:
Age is Paramount: The patient's age (in years, months, and days) is a critical initial input, as it dictates normal ranges for vital signs.
Life-Threatening Conditions (ESI 1): Assessment for immediate life-threatening conditions (e.g., severe trauma, cardiac arrest, severe respiratory failure) is the first step. A "yes" immediately classifies the child as ESI 1.
High Risk or Severe Pain/Distress (ESI 2): If not ESI 1, the clinician assesses if the child is at high risk of deterioration or in severe pain/distress. This includes conditions that may rapidly worsen or require urgent attention.
Resource Needs (ESI 3, 4, 5): For stable children not meeting ESI 1 or 2 criteria, resource prediction follows.
Vital Signs: Vital signs (heart rate, respiratory rate, oxygen saturation, blood pressure) must be meticulously obtained and interpreted based on age-specific normal ranges. Abnormal vital signs for age can upgrade a child to a higher acuity level (e.g., from a resource-based ESI 3 to an acuity-based ESI 2). For example, very young infants (<3 months) presenting with fever may be automatically considered higher risk and potentially up-triaged, irrespective of initial resource prediction, due to their vulnerability to serious bacterial infection.
Effective pediatric ESI application requires clinicians to shift their assessment focus. Given children's limited communication, there is less reliance on subjective symptom reporting and a greater emphasis on keen observational skills (using tools like the PAT), knowledge of age-specific physiology and common pediatric illness presentations, and careful interpretation of caregiver reports. While the ESI algorithm's structure remains consistent, the data input and its weighting are adapted to the pediatric context. Mastery involves not just memorizing pediatric vital sign tables but also cultivating specific observational skills and understanding how common pediatric conditions map to ESI criteria, often with less direct verbal information from the patient. Specialized training, such as the ENA's "Emergency Severity Index Pediatrics 2.0 Online Course," supports this.
Table 4: Key Modifications for Pediatric ESI Triage
5.2. Geriatric Patients
The geriatric population presents distinct challenges in ED triage, and studies suggest that the ESI may struggle with this group, with increasing age being a significant factor associated with the odds of under-triage. This vulnerability stems from several unique characteristics of older adults.
Unique Challenges in Geriatric Triage:
Atypical Presentations: Older adults frequently present with atypical or non-specific symptoms for serious conditions. For example, a myocardial infarction may occur without classic chest pain, or an infection may present without fever; instead, new confusion, weakness, or falls might be the primary indicators.
Polypharmacy: The use of multiple medications is common, increasing the risk of adverse drug events and drug-drug interactions that can complicate assessment or mimic acute illness.
Multiple Comorbidities: Pre-existing chronic conditions can obscure the acute presenting problem and make it difficult to determine the primary reason for the ED visit.
Cognitive and Functional Impairments: Pre-existing dementia, delirium, or functional limitations can affect the patient's ability to provide an accurate history, and new changes in cognition are red flags.
Higher Baseline Resource Utilization: Geriatric patients often utilize more ED resources per visit compared to younger populations.
Age as a Factor: Similar to very young children, very old patients (e.g., >75 years) may warrant up-triage based on their age and presenting complaint due to diminished physiological reserves.
Given these complexities, applying ESI to geriatric patients effectively means that the threshold for considering a patient "high-risk" (Decision Point B) should often be lower, and "normal" vital signs (Decision Point D) must be interpreted with caution. Subtle changes, such as new-onset confusion, unexplained weakness, or a recent fall, can be harbingers of serious underlying illness and should weigh heavily in ESI assignment, potentially warranting an ESI Level 2 even if classic "red flag" symptoms are absent. Supplementary geriatric-specific screening questions (e.g., for falls, delirium, functional decline, elder abuse) may be beneficial alongside the standard ESI algorithm. Mastery of ESI in this context involves developing a high index of suspicion for serious conditions in older adults and proactively considering factors beyond the core ESI questions.
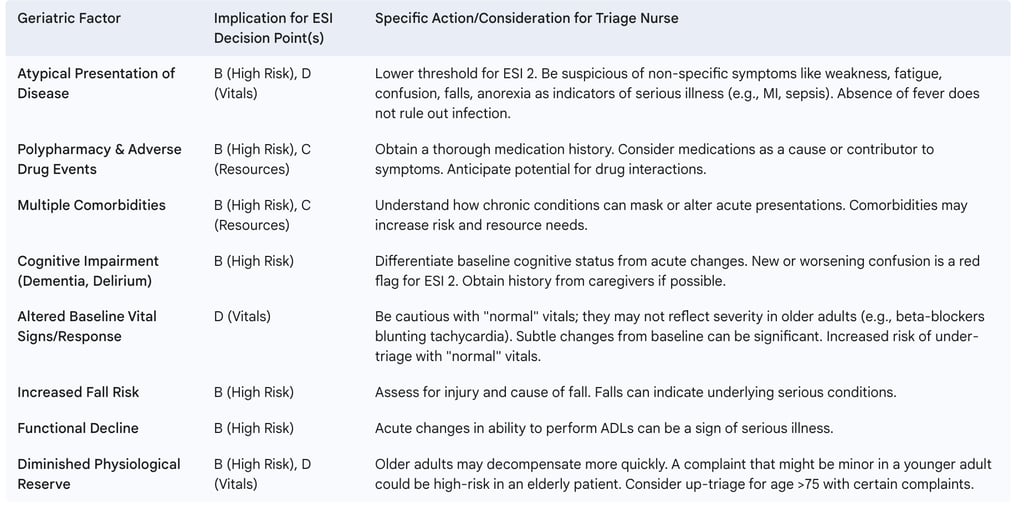
Table 5: Geriatric ESI Considerations
5.3. Pregnant Patients
Triage of pregnant patients in the ED presents a unique scenario because the assessment must consider two patients—the mother and the fetus—and because pregnancy induces significant physiological changes that can alter normal assessment parameters and mask or mimic signs of illness.
Unique Challenges in Triaging Pregnant Patients:
Altered Physiology: Pregnancy leads to changes in cardiovascular, respiratory, and hematological systems, resulting in different norms for vital signs, laboratory values, ECG findings, and even symptom morphology. What might be abnormal in a non-pregnant patient could be normal in pregnancy, and vice-versa.
Dual Focus (Maternal and Fetal): The well-being of the fetus is a critical consideration, and many ED interventions or maternal conditions can impact the fetus.
Obstetric vs. Non-Obstetric Conditions: Pregnant patients may present with conditions unrelated to pregnancy (e.g., appendicitis, trauma) or with obstetric emergencies (e.g., preeclampsia, vaginal bleeding, abruptio placentae, labor).
ESI Limitations: Standard triage acuity tools like the ESI are acknowledged to not provide the in-depth surveillance questioning and assessment specifically required to address maternal and fetal physiologic needs comprehensively. While the Maternal Fetal Triage Index (MFTI) has been developed for this purpose, it is not routinely used in general ED settings.
Given these limitations, while the ESI can be applied to pregnant patients for an initial gross categorization of urgency (identifying immediate life threats for ESI 1 or general high-risk situations for ESI 2), its utility for nuanced obstetric-specific risk assessment is restricted. Mastery of ESI in this context means recognizing these limitations and understanding that the ESI level assigned is often just a preliminary step. Early and frequent collaboration with obstetric clinicians is essential, regardless of the ESI level, if the presenting complaint could be pregnancy-related or could impact the pregnancy or fetus. Stabilizing emergent care procedures, including necessary radiologic examinations or medication administration, should not be delayed due to pregnancy status. The general triage principle of considering all childbearing-age females as potentially pregnant until proven otherwise is particularly salient.
6. ESI in Context: Comparison with Other Triage Systems
The Emergency Severity Index is a dominant triage system, especially in the United States, but it is important to understand its characteristics in relation to other widely used systems to appreciate its specific strengths and design philosophy.
6.1. Manchester Triage System (MTS)
The Manchester Triage System (MTS) is a five-level triage system extensively used in the United Kingdom and across Europe. Unlike the ESI's resource-prediction component for stable patients, the MTS is primarily designed to determine timeliness: how long a patient can safely wait for a physician assessment. It utilizes 52 standardized flowchart diagrams, each corresponding to a specific presenting complaint (e.g., "Headache," "Abdominal Pain"). Nurses select the appropriate flowchart and then work through a series of "discriminators" (specific signs or symptoms) to allocate the patient to one of five color-coded categories, each with an associated maximum target time to be seen by a clinician :
Red (Immediate): Immediate care by physician.
Orange (Very Urgent): Target time of 10 minutes.
Yellow (Urgent): Target time of 60 minutes.
Green (Standard): Target time of 2 hours.
Blue (Non-Urgent): Target time of 4 hours.
Algorithmic and Methodological Differences: The core difference lies in the primary driver for categorization in stable patients. ESI Levels 3-5 are based on predicted resource consumption , whereas MTS levels are determined by specific clinical discriminators within symptom-based flowcharts, aimed at defining safe waiting times.
Comparative Performance: Studies comparing ESI and MTS have yielded mixed results, suggesting that neither is universally superior and that their performance can be context-dependent.
One comparative study found that ESI was associated with a significantly higher rate of undertriage (20%) compared to MTS (11%) in a general ED population, though both systems were considered valid tools for acuity assessment.
In trauma patients, another study reported that the mean ED length of stay was significantly lower with MTS (115 minutes) compared to ESI (157 minutes). This study also found that ESI tended to categorize a larger proportion of trauma patients into Level 3 (70%), potentially because trauma patients often require at least one resource (e.g., X-ray), pushing them out of Level 4 even if their overall acuity might align with a less urgent MTS category.
Broader systematic reviews have suggested that there is no definitive preference for either ESI or MTS in terms of overall performance, with both demonstrating comparable capabilities in identifying critically ill patients.
The choice between ESI and MTS may hinge on an ED's primary operational priorities. An ED that prioritizes detailed anticipation of resource needs and internal workload balancing might find ESI more aligned with its goals due to its unique resource-prediction component for stable patients. Conversely, an ED focused primarily on adhering to specific time-based targets for physician assessment and managing patient queues based on maximum waiting times might favor the MTS. Understanding this fundamental difference in design philosophy—ESI's focus on "how much work" versus MTS's focus on "how long to wait"—is key when comparing these systems or considering which is a better fit for a particular healthcare environment or quality improvement initiative.
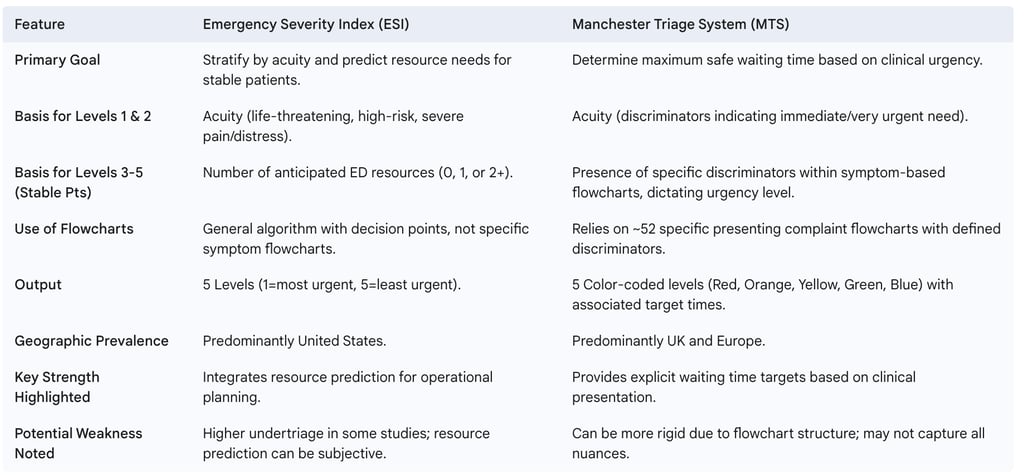
Table 6: Comparative Overview of ESI and MTS
6.2. Canadian Triage and Acuity Scale (CTAS)
The Canadian Triage and Acuity Scale (CTAS) is another widely recognized five-level triage system, predominantly used in Canadian hospitals. Similar to the MTS, CTAS primarily focuses on presenting symptoms, physiological parameters, and specific diagnostic considerations to determine how long a patient can safely wait for physician assessment and treatment. It defines maximum timeframes within which patients in each acuity level should receive care. This emphasis on timeliness based on clinical presentation aligns CTAS more closely with the MTS philosophy than with the ESI's distinct resource-prediction component for stable patients.
6.3. Considerations for Mass Casualty Incidents (MCI)
A critical aspect of mastering any ED triage system is understanding its limitations and appropriate scope of use. The ESI algorithm is not designed for and should not be used in mass casualty incidents (MCIs) or certain large-scale trauma scenarios. In such overwhelming situations, where the number of casualties vastly exceeds available resources, different triage principles and tools apply. Standard MCI triage systems, such as START (Simple Triage and Rapid Treatment) for adults and JumpSTART for pediatric patients, are designed for extremely rapid sorting of casualties (often in seconds per patient) into broad categories (e.g., Immediate, Delayed, Minor, Deceased/Expectant) based on basic physiological parameters like ability to walk, respiratory status, perfusion (capillary refill or pulse), and mental status. The goal in MCI triage is to do the "greatest good for the greatest number" with severely constrained resources, which often means prioritizing those with the best chance of survival with limited intervention.
The ESI's unsuitability for MCIs stems from its individualized patient assessment approach and its relatively complex resource prediction component. The detailed evaluation of an individual patient's stability and the nuanced prediction of specific ED resources are impractical and inefficient when faced with a large number of casualties requiring immediate attention. The more granular, resource-oriented methodology of ESI becomes a disadvantage in MCIs, where simpler, faster algorithms focusing on immediate life threats and basic physiological functions are far more effective for battlefield or disaster triage. Therefore, proficiency in ESI includes recognizing its boundaries and being trained in the appropriate switch to an MCI-specific triage system when circumstances demand it. Attempting to apply ESI in an MCI would be detrimental to the overall disaster response.
7. Achieving Proficiency: ESI Training, Implementation, and Quality Assurance
Mastering the Emergency Severity Index is not merely about memorizing the algorithm; it requires comprehensive training, clinical experience, effective institutional implementation, and a commitment to ongoing quality assurance.
7.1. Essential Training Components
Formal, standardized training is paramount for the reliable and valid application of the ESI. The primary authoritative resources for ESI education are the ESI Triage Tool Implementation Handbook (currently the 5th Edition, published by the Emergency Nurses Association, building upon the foundational Version 4 previously published by AHRQ) and associated training programs. The ENA offers an "Emergency Severity Index 2.0 Online Course" and a specialized "Emergency Severity Index Pediatrics 2.0 Online Course" to meet these training needs.
Effective ESI training programs should comprehensively cover:
The ESI five-level acuity scale and its underlying principles.
A detailed walkthrough of the four decision points (A, B, C, D) of the ESI algorithm.
Clear definitions and examples of what constitutes an ESI "resource" and what does not, including nuances in resource counting.
The correct use and interpretation of vital signs within the ESI framework, including age-specific considerations.
Application of the ESI algorithm to a variety of patient case studies and scenarios, covering diverse presentations and acuity levels.
Special considerations for pediatric, geriatric, and other vulnerable populations. Studies and experience show that robust training significantly improves nurses' recognition of high-risk patients and overall triage accuracy. Historically, AHRQ also produced a training DVD to accompany the Version 4 handbook, emphasizing the importance of multi-modal learning resources.
7.2. Importance of Experience
The ESI algorithm is designed for use by healthcare professionals, primarily registered nurses, who possess clinical experience in the emergency department setting. Official guidelines recommend that ESI users should have at least one year of ED experience and have completed a comprehensive ESI triage education program. This prerequisite reflects the significant degree of clinical judgment required to apply the ESI accurately, particularly when navigating Decision Point B (identifying "high-risk" situations) and Decision Point C (predicting resource utilization for stable patients). These components are more subjective than other parts of the algorithm and benefit greatly from the pattern recognition and clinical intuition that develop with experience.
Clinical experience acts as a crucial calibrator for the subjective elements within the ESI framework. An experienced ED nurse is better equipped to judge what constitutes a "high-risk" presentation for a given complaint or to accurately anticipate the typical resources required for various conditions within their specific ED environment. This experiential knowledge allows for a more nuanced and reliable application of the ESI. Therefore, ESI training should not be viewed as a one-time event. Ongoing mentorship, regular case reviews with experienced colleagues, and continued hands-on practice are vital for nurses to progress from a basic understanding of the rules to true proficiency and consistent application, thereby helping to reduce the inter-rater variability that can occur.
7.3. Implementation Strategies in EDs
Successful adoption and integration of the ESI into an ED's workflow go beyond individual staff training. It requires a systemic approach to implementation. The ESI Implementation Handbook provides detailed guidance for ED educators, clinicians, and managers on how to develop and conduct ESI educational programs, effectively implement the algorithm into daily practice, and design an ongoing quality improvement program. Key implementation strategies include:
Developing clear institutional policies and procedures for ESI application.
Ensuring staff buy-in through education on the benefits of standardized triage.
Integrating ESI documentation into the electronic health record (EHR) system.
Providing readily accessible ESI algorithm charts and resource definition lists.
Establishing a plan for initial training of all relevant staff and ongoing competency validation.
7.4. Ongoing Quality Monitoring and Competency Assessment
Triage accuracy is not a static achievement; it requires continuous attention and refinement. The ESI handbook includes chapters dedicated to quality monitoring. Regular competency assessments and ongoing quality improvement (QI) monitoring are essential to address inter-rater reliability and maintain high standards of ESI application. Effective QI programs for ESI typically involve:
Regular audits of triage records to assess accuracy and adherence to the algorithm.
Analysis of ESI data in conjunction with patient outcomes, ED length of stay, and rates of patients who leave without being seen (LWBS).
Providing constructive feedback to triage staff based on audit results.
Periodic refresher training and updates on ESI guidelines.
Reviewing challenging or high-risk triage cases to identify learning opportunities.
Quality assurance in ESI functions as an essential feedback loop. The ESI algorithm, despite its standardization, contains elements of subjectivity and is applied in dynamic, high-pressure ED environments. Inter-rater variability and the potential for errors such as under-triage or over-triage are recognized challenges. Without systematic quality monitoring, deviations from correct ESI application can become entrenched, leading to a "systemic drift" where local practices diverge from established ESI principles. Furthermore, patient populations, common presenting complaints, and even available ED resources can change over time, necessitating periodic review and potential adjustments to local interpretations or educational emphasis. Ongoing QA identifies performance gaps, informs targeted re-education, and ensures that the ESI system remains a clinically relevant, reliable, and effective tool for that specific ED, rather than degrading into an inconsistent or merely ritualistic practice. Mastering ESI at an institutional level thus requires a sustained commitment to a continuous cycle of training, application, diligent monitoring, and thoughtful refinement.
8. ESI Effectiveness, Reliability, and Common Pitfalls
The widespread adoption of the Emergency Severity Index is supported by research into its validity and reliability, as well as its reported effectiveness in improving ED operations. However, like any clinical tool, its performance is influenced by user proficiency and specific clinical contexts, and common pitfalls in its application must be recognized and addressed.
8.1. Studies on Validity and Inter-Rater Reliability
Numerous studies have generally found the ESI to be a reliable, consistent, and accurate triage tool across various settings, languages, age groups, and countries. The ESI algorithm has undergone rigorous testing and has been described as both reliable and valid in foundational ESI documentation. This broad validation has been a key factor in its extensive implementation.
However, the practical application of ESI can exhibit variability. Studies and observational data indicate that inter-rater reliability—the consistency of ESI scores assigned by different nurses to the same patient or scenario—can vary, particularly between experienced and novice nurses. Without adequate training, ongoing support, and robust quality assurance, accurate triage rates can be alarmingly low, with some reports suggesting accuracy at 60% or less in suboptimal conditions. This discrepancy suggests that while the ESI tool itself possesses a sound structure, its "proven reliability" is conditional. Achieving consistent and high reliability in real-world practice hinges critically on optimal implementation, comprehensive user training, sufficient clinical experience among triage staff, and continuous quality monitoring. Institutions cannot simply adopt the ESI and assume it will automatically yield reliable results; a sustained investment in these supporting factors is crucial to bridge any gap between the tool's potential and its actual performance.
8.2. Reported Effectiveness in Improving Patient Flow and Outcomes
A well-implemented ESI program is reported to offer significant operational benefits to emergency departments. It helps ED staff to rapidly identify patients who require immediate, life-saving attention, while also better identifying those patients who could be safely and more efficiently managed in fast-track or urgent care areas within the ED, thereby optimizing patient flow. The Emergency Nurses Association highlights that EDs utilizing ESI effectively have realized benefits such as a twofold improvement in triage acuity assignment for high-risk patients, as well as improvements in overall ED throughput, reduced length of stay (LOS), and lower rates of patients leaving without being seen (LWBS). These are key performance indicators for ED efficiency and patient satisfaction.
However, the effectiveness of ESI in improving outcomes is directly tied to its accurate application. For instance, the ESI level assigned upon arrival has been shown to correlate with median waiting times. This correlation means that undertriaged patients—those assigned a less urgent ESI level than their condition warrants—may be exposed to dangerously longer waiting times for physician assessment and treatment. This underscores the critical importance of accuracy in ESI assignment to ensure patient safety.
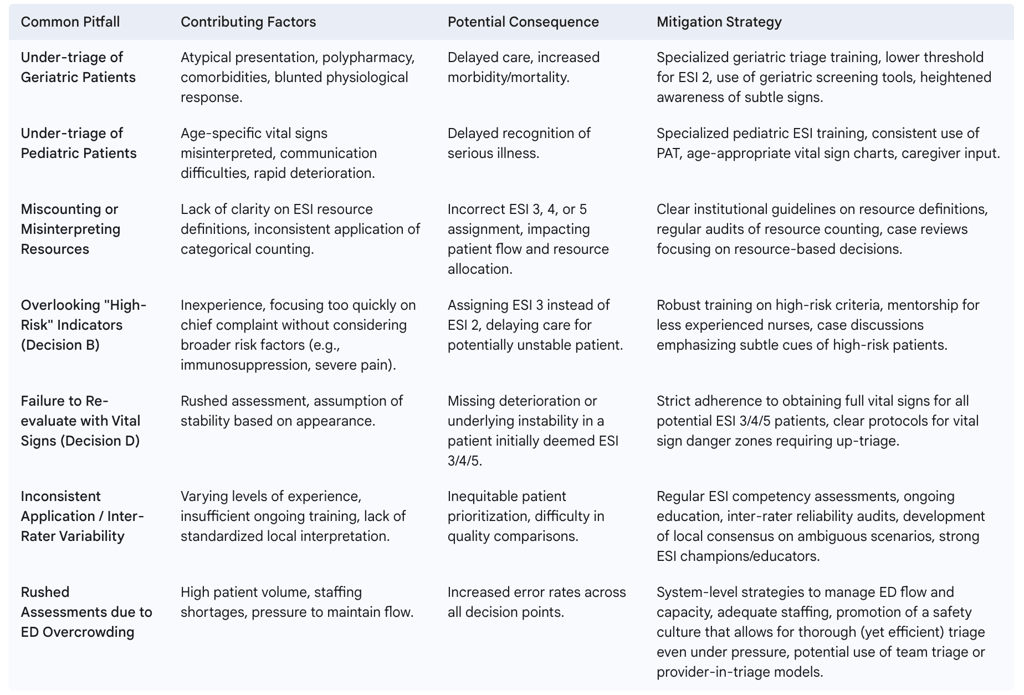
8.3. Common Errors and Pitfalls in ESI Application
Despite its structured approach, several common errors and pitfalls can occur during the application of the ESI. Awareness of these is essential for mitigation and continuous improvement:
Misclassification of Severity (Under-triage or Over-triage): This is one of the most frequent errors. Under-triage, where a patient's condition is underestimated (e.g., mistaking cardiac chest pain for indigestion), can lead to delayed care and adverse outcomes. Over-triage, while generally safer for the individual patient, can strain ED resources unnecessarily. Studies have shown that ESI can result in both under-triage and over-triage, with variations influenced by facility characteristics and specific patient populations, such as geriatric patients who are at a higher risk for under-triage.
Incomplete Patient Assessment or History: Failure to obtain a thorough patient history, including relevant medical background, medications, and allergies, can lead to inaccurate ESI assignment.
Challenges with Specific Presentations or Populations: The ESI has been noted to struggle with accurately triaging patients with certain presentations, such as non-specific abdominal pain, some psychiatric conditions, and suspected Acute Coronary Syndrome (ACS), where its association with serious outcomes may be poor without supplementary clinical tools. As discussed previously, geriatric and pediatric patients also require specialized assessment approaches within the ESI framework.
Resource Counting Errors: Misinterpreting what constitutes an ESI resource or incorrectly counting resource categories (e.g., counting each lab test individually instead of as one "lab" resource) can lead to incorrect assignment of ESI Levels 3, 4, or 5.
Over-reliance on the Algorithm / Insufficient Clinical Judgment: Mechanically applying the algorithm without considering the "whole patient" or subtle atypical factors can lead to errors. The ESI is intended to guide, not replace, clinical judgment.
Vital Sign Misinterpretation or Omission: Failing to obtain a full set of vital signs for potentially stable patients (ESI 3, 4, or 5 candidates), or not recognizing age-specific danger signs in vital parameters (especially in pediatric or geriatric patients), can result in missed opportunities to identify higher-risk individuals.
Communication Breakdowns: Ineffective communication between the patient and the triage provider, or among healthcare team members, can lead to missed critical information and flawed triage decisions.
Impact of ED Environment: High-pressure environments characterized by overcrowding and staff shortages can contribute to rushed assessments and an increased likelihood of triage errors.
Many of these common ESI pitfalls are rooted in human factors—such as cognitive biases, incomplete information gathering, or experience gaps—and systemic issues within the ED environment, rather than fundamental flaws in the ESI algorithm itself. The algorithm provides a structured decision-making pathway. However, its application by humans under pressure, often with incomplete initial information, can lead to variability. Challenges with special populations often arise because these patients do not fit neatly into typical adult presentation patterns, requiring more nuanced application of clinical judgment within the ESI framework. Therefore, improving ESI accuracy requires a multifaceted approach that extends beyond simply "knowing the algorithm." It involves robust and continuous training (with a strong emphasis on clinical judgment, special populations, and resource definitions), clear local protocols, strategies to mitigate human error in high-stress settings (e.g., cognitive aids, decision support where appropriate), and addressing systemic factors like ED staffing and patient flow management.
Table 7: Common ESI Pitfalls and Mitigation Strategies
9. Conclusion
9.1. Recap of ESI's Critical Role in Modern Emergency Medicine
The Emergency Severity Index has established itself as a vital and widely adopted standardized tool in the complex environment of modern emergency medicine. Its five-level system, which uniquely balances the assessment of patient acuity with the prediction of resource needs, provides a structured and clinically relevant approach to ED triage. By enabling healthcare professionals to rapidly identify patients requiring immediate life-saving interventions and to anticipate the care demands of more stable individuals, the ESI plays a critical role in prioritizing care, optimizing patient flow, and managing departmental resources effectively. Its widespread use, particularly in the United States, underscores its significance as a foundational element of emergency nursing and medical practice.
9.2. Emphasis on Continuous Learning, Critical Thinking, and Adherence to Best Practices
Mastering the ESI is not a singular achievement but an ongoing process that extends far beyond rote memorization of the algorithm. True proficiency demands a commitment to continuous learning, the development of astute critical thinking skills, and unwavering adherence to best practices. This includes not only a thorough understanding of the ESI decision points and resource definitions but also the cultivation of clinical experience necessary to navigate the nuances of patient presentation, especially in special populations such as pediatric, geriatric, and pregnant patients. Awareness of common pitfalls and potential errors, coupled with a dedication to quality assurance and performance improvement, is essential. Crucially, the ESI is designed as a tool to aid and structure clinical judgment, not to replace it. The experienced clinician's ability to synthesize algorithmic guidance with holistic patient assessment remains paramount.
9.3. Future Directions or Refinements in ESI or ED Triage
The field of emergency triage, including the ESI, continues to evolve. There is ongoing recognition of the need for supplementary tools or refined approaches for specific patient populations where the standard ESI may have limitations. The ESI itself has undergone revisions, as evidenced by the progression from AHRQ's Version 4 handbook to the ENA's current 5th Edition handbook and ESI 2.0 online courses, indicating a commitment to its refinement based on research and clinical feedback. Furthermore, emerging technologies, including artificial intelligence and machine learning, hold potential for augmenting triage processes in the future, potentially offering enhanced predictive capabilities or decision support. Indeed, organizations like the ENA are already exploring partnerships in AI-driven ED research. These developments suggest that while the core principles of ESI remain robust, the tools and methods for achieving optimal emergency triage will continue to adapt to new knowledge and technological advancements, always aiming to improve patient safety and the efficiency of emergency care delivery.
FAQ Section
What is the Emergency Severity Index (ESI)?
The Emergency Severity Index is a five-level triage algorithm used in emergency departments to categorize patients based on both their acuity (how quickly they need medical attention) and the number of resources they are likely to require. Developed in 1998 and currently maintained by the Emergency Nurses Association, it helps prioritize patients and allocate resources efficiently.
How does ESI differ from other triage systems?
Unlike some triage systems that focus solely on acuity, the ESI incorporates resource prediction as a key component. This dual focus helps emergency departments not only prioritize critical patients but also plan for resource utilization, making it particularly useful for operational efficiency and patient flow management.
Who can perform ESI triage?
ESI triage is typically performed by registered nurses with specialized training in the methodology. Most recommendations suggest that triage nurses should have at least one year of emergency department experience before assuming triage responsibilities, along with comprehensive training in the ESI algorithm and ongoing competency assessment.
What constitutes a "resource" in the ESI system?
In the ESI algorithm, resources include diagnostic tests (laboratory, imaging, ECG), interventions (IV fluids, medications), and consultations with specialists. Notably, simple interventions like oral medications, tetanus immunizations, and point-of-care testing are not counted as resources in the ESI framework.
How reliable is the ESI triage system?
Research has consistently demonstrated good to excellent reliability of the ESI, with inter-rater agreement (measured by kappa statistics) typically ranging from 0.7 to 0.9 across various studies. This indicates substantial agreement between different triage nurses when applying the ESI algorithm.
Does the ESI work for pediatric patients?
Yes, the ESI has been validated for use with pediatric populations, though special considerations apply. These include age-appropriate vital sign parameters and incorporation of the Pediatric Assessment Triangle (appearance, work of breathing, circulation) into the assessment process. Specific training on pediatric applications is recommended.
How long does an ESI triage assessment typically take?
Most ESI triage assessments can be completed in 2-5 minutes, though complex presentations may require additional time. The streamlined nature of the algorithm allows for efficient triage while still capturing essential information for patient prioritization.
What are the recommended response times for each ESI level?
While specific timeframes may vary by institution, general guidelines suggest immediate evaluation for ESI Level 1, evaluation within 10 minutes for ESI Level 2, within 30 minutes for ESI Level 3, within 1 hour for ESI Level 4, and within 2 hours for ESI Level 5. These timeframes should be adjusted based on departmental resources and patient volume.
How does ESI impact emergency department metrics?
Implementation of the ESI has been associated with improvements in several key emergency department metrics, including reduced length of stay for high-acuity patients, decreased left-without-being-seen rates, and more appropriate resource utilization. The system also provides valuable data for quality improvement initiatives.
Is the ESI used internationally?
While developed in the United States, the ESI has been implemented and studied in numerous countries worldwide, including Canada, European nations, Middle Eastern countries, and parts of Asia and South America. Some adaptations may be necessary to account for differences in healthcare systems and resource availability.
Additional Resources
Emergency Nurses Association. ESI Triage Research and Practice: A Comprehensive Guide. Available at: www.triageiq.com/resources/comprehensive-guide
Gilboy N, Tanabe P, Travers D, Rosenau AM. Emergency Severity Index (ESI): A Triage Tool for Emergency Department Care, Version 4. Implementation Handbook 2020 Edition. Emergency Nurses Association.
Agency for Healthcare Research and Quality. Improving Patient Flow and Reducing Emergency Department Crowding: A Guide for Hospitals. Available at: www.triageiq.com/resources/patient-flow-guide
World Health Organization. Emergency Triage Assessment and Treatment (ETAT): Manual for Participants. Geneva: WHO Press.
American College of Emergency Physicians. Emergency Department Operations Management: Best Practices and Systems Approaches. Available at: www.triageiq.com/resources/operations-management
