Manchester Triage System: Validity, Challenges, and Optimisation in Emergency Care
Explore the validity and effectiveness of the Manchester Triage System (MTS) in emergency care. This comprehensive guide discusses the system's performance, its challenges, and optimization strategies for better patient outcomes.


Emergency services worldwide are experiencing an escalating demand for care, frequently exceeding their operational capacity and leading to significant overcrowding. This imbalance necessitates a highly structured and efficient approach to patient management. Triage serves as a fundamental process for reorganizing emergency department (ED) workflows, ensuring that patient care is prioritized based on the severity of their clinical condition rather than their order of arrival. It is characterized as a dynamic classification process aimed at directing patients to the most appropriate service for timely care. Effective triage is paramount for making rapid, critical decisions, which directly contributes to improved patient outcomes, reduced waiting times, and optimized resource allocation within the ED.
The Manchester Triage System (MTS) originated in Manchester, England, during the late 1990s. It was developed by a collaborative group of emergency nurses and doctors who recognized the imperative for a more structured, consistent, and objective method for patient assessment. Since its inception, MTS has become the most widely adopted triage system across Emergency Departments in the United Kingdom and Europe. At its core, MTS is a standardized, five-level, color-coded system designed for the rapid assessment of a patient's urgency level.
This report provides an expert-level, evidence-based analysis of the Manchester Triage System. It comprehensively examines its validity and reliability, delves into the inherent challenges and limitations encountered during its implementation, and explores effective strategies for its optimization within the complex environment of emergency care. The aim is to offer actionable insights to healthcare administrators, policymakers, and clinical leaders for informed decision-making, quality improvement initiatives, and strategic planning.
I. Fundamentals of the Manchester Triage System
The Manchester Triage System operates as a five-level classification tool, designed to provide a standardized approach to patient assessment in emergency settings. Its methodology relies on trained healthcare professionals who adhere to specific guidelines, ask targeted questions, and observe the patient's condition upon arrival. The system's development was rooted in evidence-based guidelines and the practical expertise of clinical professionals, emphasizing user-friendliness to facilitate quick and accurate patient needs assessment.
A central component of the MTS methodology involves the use of 52 (or 53 in some extended versions) predefined flowchart diagrams. Each flowchart corresponds to a specific reason for encounter, and triage nurses compare the patient's presenting complaints against these diagrams. A critical safety feature of MTS is its "reductive system" methodology. This approach begins with the initial premise that the patient's condition is potentially life-threatening. Triage nurses are then systematically required to rule out all high-priority discriminators before any reduction in the patient's assigned priority level can occur, thereby ensuring the inherent safety of the system. This design choice inherently biases the system towards patient safety by initially assuming the worst-case scenario. It minimizes the risk of undertriage—failing to identify a critical condition—by compelling the triage nurse to actively exclude severe conditions before assigning a lower priority. This proactive safety stance is a fundamental strength of the MTS, even if it may contribute to overtriage, where a higher priority is assigned than strictly necessary. This reveals a deliberate, safety-first philosophy embedded in the MTS design.
The MTS is consistently described as a "standardized" system that relies on "flowchart diagrams" and "fixed rules". Simultaneously, it is acknowledged that "decisions made regarding patient outcome are a clinical judgement made by the clinician". This highlights a critical dynamic within the system: MTS provides a structured framework to minimize variability and human error , yet its effective application ultimately requires the nuanced clinical judgment of a trained professional. The success of MTS hinges on balancing algorithmic guidance with the expertise and interpretive skills of the triage nurse. This duality is a source of both strength, through consistency, and potential weakness, through susceptibility to human error and bias. It indicates that MTS is not a purely automated system but a tool that augments, rather than replaces, human expertise.
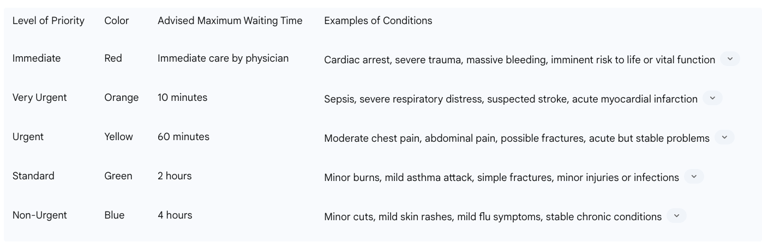
The Five-Level Prioritization System: Categories and Target Waiting Times
Patients are assigned to one of five distinct triage categories, each represented by a specific color and associated with a target maximum waiting time for physician attention. This tiered categorization is crucial for prioritizing patients effectively, ensuring that those with the most critical needs are seen first, thereby optimizing patient flow and resource allocation within the ED. It is important to note that triage is a dynamic process, and patients are continuously reassessed, allowing for re-categorization as their conditions evolve.
The five levels are detailed in Table 1:
Table 1: Manchester Triage System Five Priority Levels and Target Waiting Times

Role of Flowcharts and Discriminators in Patient Classification
Triage nurses utilize a list of 52 or 53 flowcharts, selecting the most appropriate one based on the patient's primary complaint, medical history, and presenting signs and symptoms. Each flowchart incorporates 'decision points' or 'discriminators'—these are specific key symptoms or signs that guide the nurse in determining the appropriate urgency level for the patient. For instance, when assessing a rash, the nurse would ask specific MTS-driven questions about its description, spread, associated symptoms (fever, swelling, pain), and potential exposures. Digital solutions like the eTriage system, which mirrors the MTS, employ branched algorithm decision logic with key discriminators that prompt further questioning, thereby standardizing and supporting the classification process.
II. Validity and Reliability of the Manchester Triage System
The effectiveness of the Manchester Triage System is contingent upon its validity and reliability, which have been extensively studied across various clinical settings.
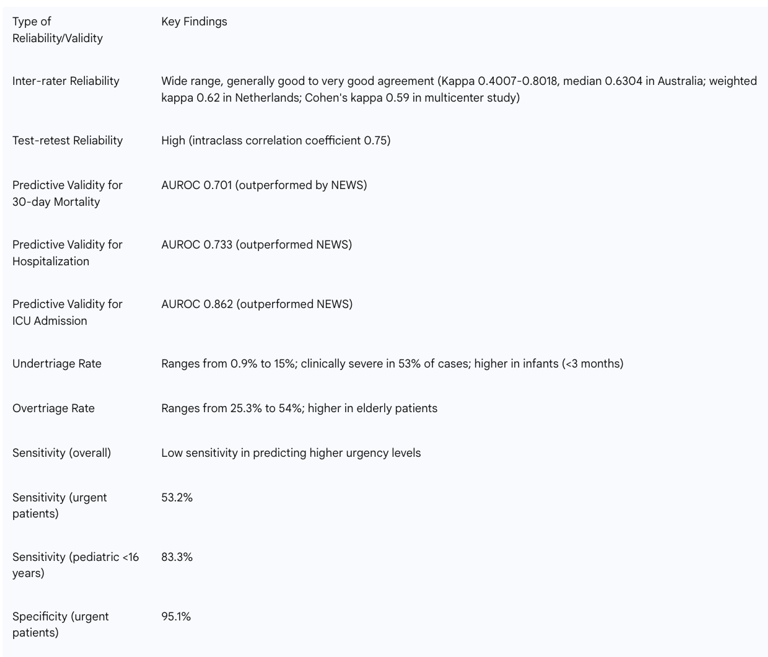
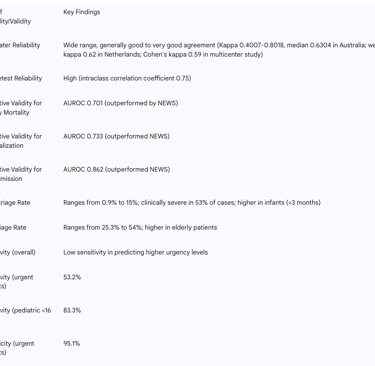
Inter-rater and Intra-rater Reliability Assessments
Studies on the Manchester Triage System consistently report a wide range of inter-rater agreement, with a general prevalence of good to very good agreement among healthcare professionals. Reliability, often assessed using the "kappa" statistic, varies across studies. An Australian study found weighted kappas ranging from 0.4007 to 0.8018, with a median of 0.6304, indicating overall reliability. A simulation study conducted in the Netherlands reported "substantial" inter-rater reliability (weighted kappa 0.62) and high test-retest reliability (intraclass correlation coefficient 0.75). Another study cited an unweighted kappa of 0.61, a linear weighted kappa of 0.71, and a quadratic weighted kappa of 0.81. According to standard interpretations, a kappa value between 0.41 and 0.60 indicates "moderate" reliability, while 0.61 to 0.80 signifies "substantial" reliability, and 0.81 to 1.00 indicates "almost perfect" agreement. This places MTS reliability predominantly in the "moderate" to "substantial" range.
However, a more recent multicenter vignette study (March 2025) presented a nuanced finding: the overall agreement (Cohen's kappa) was 0.59, and critically, it concluded that "Nurses with more ED experience and triage expertise had higher error rates" when applying MTS using case vignettes. This finding appears to contradict an older simulation study (August 2008) which stated, "No significant association was found between the experience of emergency department nurses and the reliability score (kappa)". This "experience paradox" is a critical, counter-intuitive observation. It suggests that simply having more years of experience in the ED or with triage does not automatically translate to higher MTS accuracy, and in fact, might lead to more errors in simulated scenarios. This could be attributed to an over-reliance on intuition rather than strict adherence to the MTS algorithm, or perhaps a lack of updated training for experienced staff. This observation points to a crucial area for optimization: the need for continuous, targeted training, especially for experienced nurses, to reinforce adherence to protocols and mitigate potential biases or shortcuts developed over time. It also raises the question of whether this observation is specific to vignette studies or if it translates to real-world clinical practice. The quality of reporting in studies investigating the reliability and validity of the Manchester Triage System is generally considered good.
Predictive Validity for Key Clinical Outcomes
The validity of MTS has been assessed against various clinical outcomes, including its ability to predict mortality, hospital admission, resource utilization, and length of stay in the emergency department. MTS has demonstrated its effectiveness as a tool for distinguishing between patients with a high versus low unadjusted risk of short-term death and those who will require hospitalization for at least 24 hours.
A direct comparison between MTS and the National Early Warning Score (NEWS) revealed that NEWS exhibited superior predictive accuracy for 30-day mortality (AUROC 0.745 vs. 0.701, p < 0.001). Decision Curve Analysis (DCA) also supported NEWS's greater net clinical benefit for mortality prediction. Conversely, MTS significantly outperformed NEWS across several other critical outcomes: hospitalization (AUROC 0.733 vs. 0.609, p < 0.001), ICU admission (AUROC 0.862 vs. 0.672, p < 0.001), and all secondary outcomes, including life-saving interventions, physician-defined clinical priority, and physician-defined severity. These findings imply that while NEWS is effective for predicting mortality, MTS remains the superior system for comprehensive triage decision-making and prioritizing high-risk patients based on their clinical severity. This highlights that MTS is fundamentally designed for initial risk stratification and resource allocation based on presenting symptoms, rather than a long-term prognostic tool. Its primary value lies in immediate operational decision-making within the ED. This means that while NEWS might be a good complementary tool for identifying patients at risk of future deterioration, it should not replace MTS for the primary function of triage. The implication for practice is that a multi-faceted approach, integrating MTS for initial severity assessment and potentially NEWS for ongoing monitoring or specific mortality risk stratification, might be optimal. The ongoing debate regarding the most appropriate outcome for evaluating triage systems is relevant here; 30-day mortality, being influenced by numerous post-triage factors and having a relatively low prevalence in ED settings, may not serve as the most comprehensive single endpoint for assessing triage effectiveness.
Analysis of Undertriage and Overtriage Rates
A significant concern highlighted in the literature is the "low safety" of MTS, primarily attributed to a notable rate of undertriage and a corresponding low sensitivity in accurately predicting higher urgency levels. Conversely, a high rate of overtriage, where patients are assigned a higher urgency than warranted, could lead to inefficient and unnecessarily high utilization of emergency department resources. This reveals a fundamental tension in triage system design. While prioritizing patient safety by minimizing missed critical conditions is essential, the resulting overtriage can strain already limited ED resources, potentially exacerbating overcrowding and affecting the timely care of other patients. Optimizing MTS involves finding a delicate balance that maintains safety (low undertriage) without unduly compromising efficiency (high overtriage). This suggests a need for targeted modifications to reduce overtriage without inadvertently increasing the risk of undertriage.
Specific rates observed include:
Undertriage: Reported at 11% in one comparison study (lower than ESI's 20%). While generally infrequent (0.9% in one study), when it occurs, experts deem it clinically severe in 53% of cases. Undertriage is more likely to occur in infants, particularly those younger than three months, and in children assigned to the MTS 'unwell child' flowchart.
Overtriage: This occurs more frequently than undertriage (25.3% vs 7.6% in a general ED population), with a particular prevalence in elderly patients. In pediatric emergency care, 54% of children were over-triaged, while 12% were under-triaged.
Patients presenting with headaches, especially those with warning signs indicating a potential emergency, are frequently undertriaged (85.1% in the very urgent classification level and 23.3% in the urgent level).
MTS also demonstrates an inability to correctly stratify patients with Transient Global Amnesia (TGA), resulting in 13.0% undertriage and 37.5% overtriage.
Sensitivity and Specificity in Identifying Urgency Levels
MTS generally exhibits low sensitivity in predicting higher urgency levels. For urgent patients in a general emergency department population, the reported sensitivity of MTS was 53.2%, with a specificity of 95.1%. In pediatric patients (under 16 years), MTS showed a higher sensitivity of 83.3%. However, for detecting emergent/very urgent cases in pediatric EDs, it demonstrated moderate sensitivity (63%) and specificity (78%). For critically ill patients presenting with chest pain, MTS had a sensitivity of 45.7% and a specificity of 84.8%, achieving an overall accuracy of 81.9%.
Table 2: Summary of MTS Validity and Reliability Findings
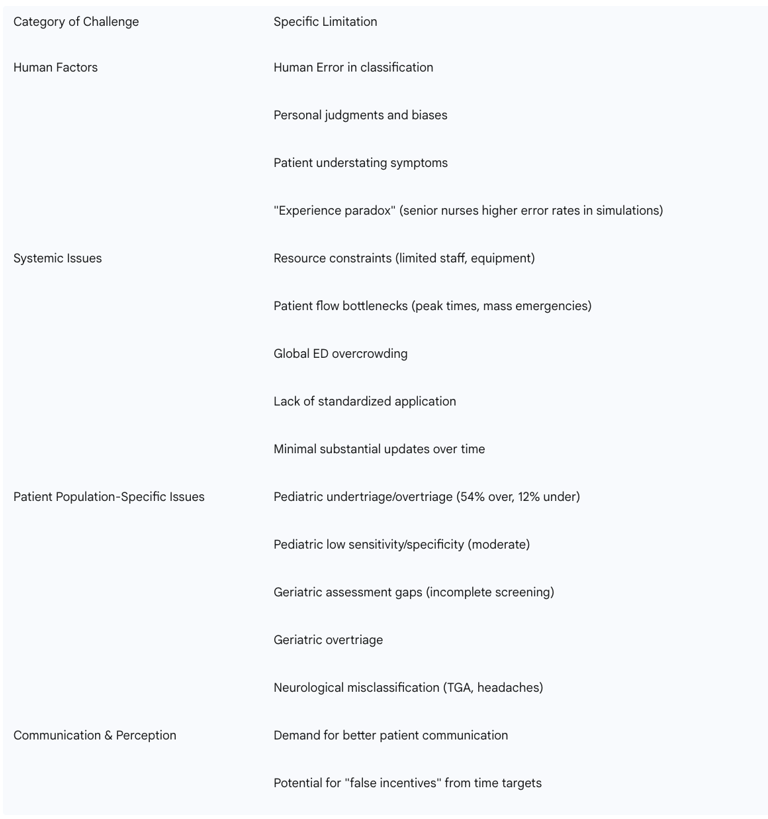
III. Challenges and Limitations in MTS Implementation
Despite its widespread adoption and foundational strengths, the Manchester Triage System faces several significant challenges and limitations in its real-world implementation, many of which extend beyond the algorithmic design itself.
Impact of Human Error and Cognitive Biases in Triage Decisions
Triage nurses operate under immense pressure, which can lead to human errors in classification. Personal judgments and inherent biases can influence patient categorization, potentially leading to inconsistencies in triage decisions. Patients themselves may inadvertently understate their symptoms, contributing to misclassification within the MTS framework. The "experience paradox," as previously discussed, suggests that, in simulated scenarios, more senior nurses with extensive ED experience and triage expertise might exhibit higher error rates in MTS application. This highlights a complex interplay between accumulated experience and the consistent adherence to structured protocols.
Resource Constraints and Patient Flow Bottlenecks
Limited staff and resources, a common challenge in healthcare systems globally, can result in longer than acceptable delays for patients, even when accurately categorized by MTS. Peak times or large-scale emergencies can create significant patient flow bottlenecks, overwhelming the system despite accurate categorization. Emergency room congestion is a pervasive global issue, frequently caused by rising patient volumes, leading to significant organizational challenges.
Lack of Standardized Application and Evidence for Benefits
Despite its widespread use, particularly in the European Union, a significant limitation of MTS is the current "no standard for its application, nor significant evidence of its benefits". This lack of universal guidelines can lead to considerable variability in its implementation across different emergency units, potentially impacting its overall effectiveness. Furthermore, a criticism leveled against widely used triage systems, including MTS, is their minimal substantial updates over time, leading to a failure to improve despite an increasing body of scientific evidence.
Many of the challenges associated with MTS are not inherent to the algorithm itself but stem from human factors and broader systemic issues. The statement that "no measurement instrument is infallible, as measurement errors can arise from personal factors, environmental conditions, changes in data collection methods, and the process of cultural adaptation" strongly reinforces this multi-faceted nature of limitations. This indicates that simply refining the MTS algorithm or its flowcharts will not fully resolve its limitations. A holistic approach is required, focusing on improving human performance through robust training and ongoing support, addressing systemic resource issues, and ensuring consistent, standardized application across diverse clinical settings. The "lack of standard for its application" is a critical systemic flaw, suggesting that even a well-designed tool can be undermined by inconsistent implementation practices.
Specific Challenges in Diverse Patient Populations
The evidence consistently highlights specific challenges with MTS's validity and accuracy in certain patient populations, often leading to misclassification. This suggests that while MTS provides a broad, foundational framework for triage, its "one-size-fits-all" approach for all patient populations is a significant limitation. As medical understanding advances and patient demographics shift, such as the increasing elderly population, there is a growing and critical need for specialized, adapted protocols or supplementary tools within the existing MTS framework. This would improve accuracy, reduce misclassification, and enhance patient safety for vulnerable or complex patient groups, pointing to a continuous adaptation requirement for triage systems.
Pediatric Patients: MTS exhibits only moderate sensitivity and specificity in pediatric emergency care, a limitation potentially stemming from a lack of specific flowcharts tailored for this age group. Studies report significant rates of both over-triage (54%) and under-triage (12%) in children. Infants, especially those younger than three months, are particularly prone to undertriage.
Geriatric Patients: The current emergency triage system is noted to not fully screen geriatric patients with severe acute illness. There is an identified need for the addition of comprehensive assessment tools specifically designed to match the unique characteristics of geriatric patients to improve triage outcomes for this population. Overtriage is also observed more frequently in elderly patients.
Neurological Problems: MTS demonstrates an inability to correctly stratify patients presenting with Transient Global Amnesia (TGA), indicating a clear need for specific flowcharts dedicated to neurological conditions to enhance its performance in such cases. Similarly, headache patients with warning signs are frequently undertriaged.
Communication Gaps and Patient Perceptions
While patients generally express trust in the MTS and healthcare professionals, there is an evident demand for improved communication with patients regarding their triage status and expected waiting times, along with general improvements in ED infrastructure and strategies to reduce actual waiting times. The practice of displaying time targets for treatment to ED personnel may inadvertently lead to "false incentives," potentially impacting the quality or thoroughness of care in pursuit of meeting time goals.
Table 4: Key Challenges and Limitations of MTS

IV. Optimization Strategies for the Manchester Triage System
To address the identified challenges and enhance the effectiveness of the Manchester Triage System, a multi-faceted approach incorporating advancements in training, technology, and operational management is essential.
Enhancing Training and Capacity Building for Triage Staff
Proper and comprehensive training is paramount for effective MTS implementation. This training must cover a deep understanding of triage criteria, the ability to quickly assess patients' signs and symptoms, and the capacity to make fast and accurate decisions. Ongoing training programs are vital not only for onboarding new team members but also for continuously updating existing professionals on best practices and any changes in protocols. Utilizing objective analysis tools, such as video analysis of triage processes, can help identify potential inconsistencies in categorization across different shifts and personnel. This approach can then prompt additional, targeted training and support to improve triage decision-making. Such feedback loops improve team cohesion and enhance skill development. Addressing the "experience paradox"—where more senior nurses may exhibit higher error rates in simulated MTS application—requires a specific focus on how to best support their clinical decision-making in triage, potentially through refresher courses or advanced training that reinforces algorithmic adherence.
Leveraging Technological Tools
The adoption of technological tools, such as software designed to perform triage functions, can significantly help standardize the triage process and minimize human errors. Electronic triage systems (e.g., eTriage, Ninsaúde Clinic) provide crucial support to healthcare professionals by aiding in documentation and decision-making. These systems can also facilitate the integration of medical records and communication between different departments, thereby optimizing the entire care process. AI-powered solutions, such as KATE, have demonstrated the ability to significantly improve triage accuracy by reducing variability and human error. This leads to the prompt identification of high-risk patients and overall streamlined operations within the ED. Seamless integration with Electronic Health Records (EHRs) and Hospital Information Systems (HIS) can further streamline the triage process, provide real-time access to comprehensive patient information, and contribute to a reduction in medical errors. Digital check-in kiosks can automate the initial patient check-in process, allowing patients to directly enter demographic details and medical history upon arrival. This reduces the administrative workload on clinical staff, enabling them to focus on direct patient care.
These descriptions of technological tools suggest a shift towards a "smart triage" ecosystem. The various components—digital kiosks for check-in, electronic triage software mirroring MTS, AI-powered solutions for accuracy, and EHR integration—are not isolated tools but rather form an interconnected system. This integration implies a future where MTS is not a standalone protocol but a central component within a comprehensive digital health ecosystem. Such an environment could lead to more efficient data capture, reduced administrative burden, real-time analytics for performance monitoring, and potentially more consistent and accurate triage decisions by augmenting human judgment with computational power. The primary challenge lies in ensuring seamless interoperability between these various technological components and avoiding over-reliance on technology without adequate human oversight and clinical judgment.
Implementing Nurse-Initiated Care Pathways and Rapid Assessment Zones (RATZs)
Empowering nurses through nurse-initiated care pathways and protocols allows them to initiate diagnostic tests, treatments, and referrals without requiring immediate physician input. The benefits include reduced patient wait times, improved patient satisfaction, enhanced nurse autonomy and job satisfaction, and more efficient utilization of physician resources. Rapid Assessment and Treatment Zones (RATZs) provide a structured approach for rapid assessment and treatment for certain patient categories. This strategy leads to reduced wait times, improved patient satisfaction, and enhanced ED efficiency.
These strategies, which revolve around empowering nurses, highlight a strategic shift in ED management. They recognize nurses as critical drivers of efficiency and patient flow, rather than merely implementers of protocols. By enabling nurses to act more autonomously within defined pathways, the system can reduce bottlenecks caused by waiting for physician input, leading to faster patient care and better utilization of physician resources. This also implies a need for robust training and clear protocols to support this expanded role, ensuring that increased autonomy is coupled with enhanced competency and accountability.
Improving Staffing Levels and Resource Allocation
Ensuring adequate staffing levels, particularly during peak periods, is identified as a best practice for effective triage and overall ED operation. Performance-oriented staff planning, which utilizes patient-specific engagement time data categorized by MTS levels, can objectively calculate the required full-time nursing staff. For instance, patients classified in the Red MTS category require significantly more nursing engagement time (an average of 97.93 minutes per patient) compared to those in the Blue category (14.99 minutes per patient), demonstrating the varying resource intensity. The methodology supports timely adjustments to staffing requirements based on alterations in patient flow and workload fluctuations.
Continuous Performance Monitoring and Feedback Loops
Implementing real-time data analytics and performance monitoring systems can help EDs identify areas for improvement and continuously optimize triage performance. Regular review and adjustment of triage criteria are necessary, especially for patient groups that pose specific classification challenges, such as headache patients. A formal governance structure for MTS is crucial to ensure routine training, audit, and robust ongoing review. This ensures that the triage tools remain safe, up-to-date, and relevant to current clinical practice.
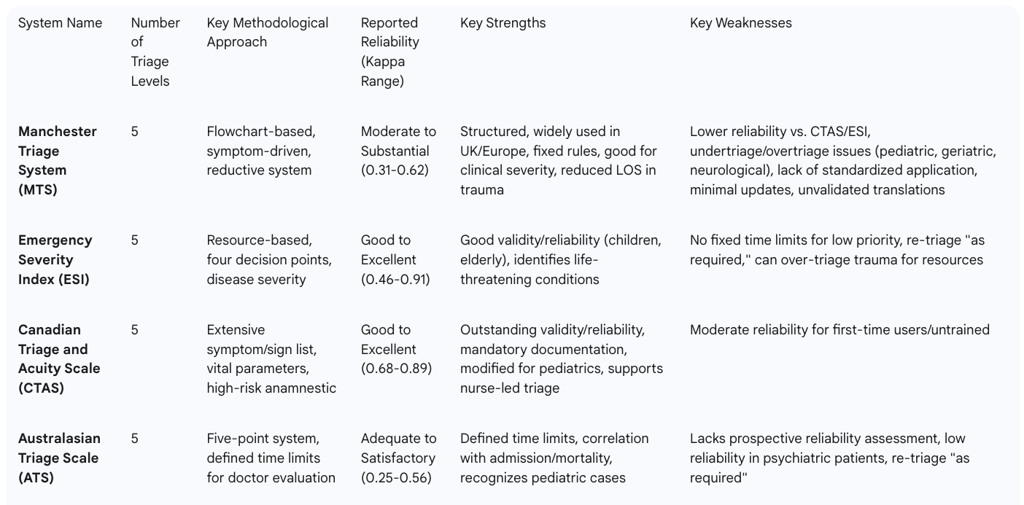
V. Comparative Analysis with Other Triage Systems
Globally, the emergency care landscape utilizes several prominent five-level triage instruments. The most extensively studied among these include the Australasian Triage Scale (ATS), the Canadian Triage and Acuity Scale (CTAS), the Manchester Triage System (MTS), and the Emergency Severity Index (ESI). Research indicates that triage instruments employing five levels of severity classification are generally superior to those with only three levels in terms of both validity and reliability.
MTS vs. Emergency Severity Index (ESI)
Reliability: ESI typically demonstrates good to excellent interobserver reliability, with kappa values ranging from 0.46 to 0.91, including strong reliability for pediatric cases (kappa 0.82). In contrast, MTS reliability is often reported as "moderate" to "substantial," with kappa values between 0.31 and 0.62.
Methodology: ESI's approach to treatment priority is based on the patient's disease severity and the anticipated need for resources, guided by four key decision points and specific questions. MTS, conversely, relies on a system of 52 or 53 flowcharts derived from the patient's chief complaint and specific discriminators. This reveals a fundamental philosophical difference in triage system design: a resource-driven approach (ESI) versus a symptom-driven approach (MTS). The choice of system has direct operational consequences on ED flow and resource utilization. While ESI's focus on resources aims to prepare for necessary interventions, it can inadvertently contribute to congestion. MTS's symptom-driven approach, despite its overtriage tendencies for safety, might be more efficient in managing patient flow for certain conditions like trauma by allowing quicker movement through the system. This suggests that there is no single "best" system for all contexts; hospitals should select or adapt a system based on their specific patient population, resource availability, and operational goals.
Trauma Patients: A comparative study on trauma patients revealed that the mean length of stay (LOS) in the emergency department was significantly lower in the MTS group (115 minutes) compared to the ESI group (157 minutes) (p<0.05). This difference is partly attributed to ESI's tendency to triage a higher percentage of trauma patients to level 3 (70% in one study) due to the perceived need for resources like X-rays or sutures, regardless of immediate clinical severity. This can inadvertently lead to more patients being routed to the main ED rather than a fast track, potentially wasting staff time and energy. In the same study, MTS distributed patients differently, with 34% in level 3 (yellow) and 48% in green.
Hospitalization/Mortality: Hospitalization rates were found to be approximately equal at each triage level across both systems in the trauma patient study. The mortality rate in both groups within that specific study was 0%.
Strengths of ESI: Demonstrates good validity and reliability in specific patient groups (e.g., children, elderly), has a validated German translation, and is designed to identify life-threatening conditions (ESI levels 1 and 2) first.
Weaknesses of ESI: Does not specify fixed time limits for low-priority patients (levels 3 to 5), and re-triage is only suggested "as and when required".
MTS vs. Canadian Triage and Acuity Scale (CTAS)
Reliability: CTAS consistently reports good to excellent interobserver reliability, with kappa values ranging from 0.68 to 0.89. Its reliability is also strong for pediatric patients (kappa 0.51 to 0.72). MTS, in comparison, is generally considered moderately reliable.
Methodology: CTAS is an adaptation of the ATS, employing an extensive list of presenting clinical complaints, high-risk anamnestic parameters, clinical signs, and vital parameters. It mandates re-triage after defined waiting times or upon changes in patient symptoms.
Strengths of CTAS: Recognized for outstanding validity and reliability, compulsory documentation of parameters in Canada, availability of a modified instrument for pediatric emergencies, and software encapsulation of descriptors and modifiers. It supports nurse-led triage, even in rural areas, and provides comprehensive implementation and training materials.
Weaknesses of CTAS: Some studies indicate only moderate reliability, particularly for first-time users or those without specialized training.
MTS vs. Australasian Triage Scale (ATS)
Reliability: ATS shows adequate to satisfactory reliability in adult emergency patients, with kappa values ranging from 0.25 to 0.56. MTS is generally considered moderately reliable.
Methodology: ATS is a five-point triage system that serves as the foundation for triage in most Australian emergency departments. Each priority level within ATS has a defined time limit for physician evaluation.
Strengths of ATS: Features defined time limits for physician evaluation, publishes process data from individual hospitals, and demonstrates correlation with inpatient admission rates and agreement with mortality data. It incorporates a four-point pain scale and explicitly recognizes pediatric cases as an important factor.
Weaknesses of ATS: Lacks prospective assessment of its reliability, shows low reliability in psychiatric patient populations (approximately 60% agreement), and re-triage is only specified "as required" rather than at fixed intervals.
Strengths and Weaknesses of MTS in Comparison
Strengths: MTS is widely utilized across the UK and Europe, offering a structured flowchart-based approach with fixed rules and readily available implementation and training materials. Notably, in trauma patients, MTS has been shown to significantly reduce the length of care in the emergency unit compared to ESI.
Weaknesses: Compared to CTAS and ESI, MTS is supported by fewer studies demonstrating satisfactory reliability, often falling into the moderate reliability range. It faces persistent issues with undertriage and overtriage, particularly pronounced in pediatric and elderly patient populations. Furthermore, modified German translations of MTS exist with potentially unfamiliar concepts (e.g., "hot adult," "young pain") and a notable absence of published validity and reliability data for these adapted versions. The system also lacks explicitly specified time to initial assessment and re-triage intervals in some contexts.
The challenges MTS faces with validity in pediatric and geriatric populations and the existence of "modified translations" (e.g., German version) with potentially unaccustomed concepts and a lack of published validation data underscore a critical point: a triage system, even if effective in its original context, is not universally applicable without rigorous adaptation and re-validation for different patient demographics, cultural contexts, and language translations. The absence of such validation for modified versions poses a significant risk to patient safety and system effectiveness. This implies a continuous need for localized research and validation studies when implementing or adapting MTS, rather than a simple "copy-paste" approach. The effectiveness of a triage system is intrinsically tied to its contextual fit and ongoing empirical verification.
Table 6: Comparative Overview of Major Triage Systems (MTS, ESI, CTAS, ATS)

VI. Real-World Applications and Outcomes
The Manchester Triage System has a tangible impact on the operational efficiency and patient outcomes within emergency care settings.
Impact on Patient Flow and Waiting Times
The Manchester Triage System is designed to effectively reduce queues in emergency units and aid in decision-making, ensuring that patients are assessed and prioritized based on the severity of their clinical condition rather than their order of arrival. MTS excels at rapid assessment and prioritization, which has been shown to significantly reduce the time required to identify and initiate treatment for critically ill patients. This rapid prioritization directly leads to improved survival rates and reduced long-term health complications. Furthermore, MTS optimizes patient flow, ensuring resources are allocated efficiently and patients receive timely care, which translates to reduced waiting times and faster access to necessary treatments. This structured approach allows emergency departments to focus resources on patients who need immediate care while ensuring everyone is attended to in a timely manner.
Resource Allocation and Efficiency
By minimizing variability in clinical decision-making, MTS ensures that patients receive appropriate and timely treatment, directly impacting their recovery and return-to-work timelines. This consistent application of clinical guidelines translates to more predictable and reliable patient experiences. The system's ability to categorize patients by urgency allows for the more efficient use of available resources. Studies confirm that MTS is a helpful tool for patient triage in emergency situations, improving patient outcomes and resource allocation. It enhances the quality of clinical evaluations performed by nurses, incorporating essential elements like reviewing medical history, taking vital signs, and performing auscultation.
Improved Patient Outcomes
The fundamental goal of MTS is to improve patient outcomes by ensuring that those with the most critical needs are seen first. Research consistently shows that MTS significantly reduces the time taken to identify and treat critically ill patients, directly leading to improved survival rates and reduced long-term health complications. The system has proven reliable in forecasting ED visits and short-term mortality. For trauma patients, MTS has been shown to significantly reduce the length of care in the emergency unit. It can also reduce treatment time for patients classified in the highest priority categories (orange and yellow). Studies indicate high accuracy in patient risk classification through MTS, with one study showing that in 91% of cases, waiting times reflected urgency ratings, and 98% of ratings corresponded to later medical diagnoses. MTS provides a high level of safety for severe illnesses and is an effective tool for prioritizing patients with symptoms requiring immediate attention, such as those with Acute Coronary Syndrome (ACS) or respiratory symptoms.
An illustrative example of MTS application involves a patient presenting with a rash. A trained nurse, guided by MTS principles, would gather basic information about the rash and the patient's concerns. The nurse would then ask specific, MTS-driven questions to determine urgency, such as describing the rash, its onset and spread, presence of other symptoms like fever or pain, and any unusual exposures or known allergies. This structured questioning ensures a thorough assessment and appropriate categorization.
Conclusion
The Manchester Triage System stands as a cornerstone of emergency care, providing a structured, five-level, color-coded framework for prioritizing patients based on clinical urgency. Its foundational principles, rooted in a "reductive methodology," inherently prioritize patient safety by requiring the systematic exclusion of life-threatening conditions before assigning lower priority levels. This design minimizes undertriage, a critical aspect of emergency care. The system effectively guides resource allocation and has demonstrated its ability to reduce patient waiting times and improve overall patient flow, leading to better patient outcomes, particularly for critically ill individuals.
However, the comprehensive analysis reveals several persistent challenges. While MTS exhibits good to substantial inter-rater reliability, the "experience paradox"—where more experienced nurses may show higher error rates in simulated scenarios—underscores the complex interplay of human factors, training, and adherence to protocols. The system's predictive validity, while strong for clinical severity, hospitalization, and ICU admission, is surpassed by tools like NEWS for 30-day mortality, indicating MTS's primary role as an initial risk stratification tool rather than a long-term prognostic indicator. Significant rates of overtriage, particularly in elderly populations, can lead to inefficient resource utilization. Furthermore, the lack of standardized application across diverse settings, minimal updates to the core system, and specific limitations in accurately triaging pediatric, geriatric, and neurological patient populations necessitate continuous adaptation. The current "one-size-fits-all" approach for these nuanced groups often results in misclassification, highlighting a critical need for specialized protocols.
To optimize the Manchester Triage System and address these limitations, a multi-faceted strategy is imperative:
Enhanced and Continuous Training: Implement robust, ongoing training programs for all triage staff, including experienced nurses, to reinforce algorithmic adherence, mitigate biases, and address the "experience paradox." Objective analysis tools, such as video review, can provide targeted feedback for skill development.
Technological Integration: Embrace a "smart triage" ecosystem by leveraging electronic triage systems, AI-powered solutions, and seamless integration with EHRs. These technologies can standardize processes, reduce human error, streamline documentation, and provide real-time data for decision-making, thereby augmenting human judgment.
Nurse Empowerment and Process Streamlining: Implement nurse-initiated care pathways and establish Rapid Assessment and Treatment Zones (RATZs) to empower nurses, reduce bottlenecks, and optimize the utilization of physician resources, thereby enhancing overall ED efficiency.
Strategic Staffing and Resource Allocation: Utilize performance-oriented staff planning based on MTS-specific patient engagement times to ensure adequate staffing levels, particularly during peak periods, and to make timely adjustments to fluctuating workloads.
Rigorous Performance Monitoring and Adaptation: Establish formal governance structures for continuous auditing, review, and adjustment of MTS criteria. Crucially, conduct localized research and validation studies when implementing or adapting MTS in new contexts or for specific patient demographics to ensure its continued effectiveness and safety.
In conclusion, the Manchester Triage System remains a vital and effective tool for managing patient flow and prioritizing care in emergency departments. However, its full potential can only be realized through a commitment to addressing its inherent challenges with human factors, systemic resource limitations, and the evolving complexities of diverse patient populations. By strategically investing in comprehensive training, technological advancements, process optimization, and continuous validation, healthcare systems can significantly enhance the accuracy, efficiency, and safety of MTS, ultimately leading to improved patient outcomes in emergency care.
FAQ Section
1. What is the Manchester Triage System (MTS) and why was it developed?
The Manchester Triage System (MTS) is a standardised, five-level, colour-coded system designed for the rapid assessment and prioritisation of patients in emergency departments (EDs). It was developed in Manchester, England, in the late 1990s by emergency nurses and doctors. The primary reason for its development was to create a more structured, consistent, and objective method for patient assessment, aiming to address the escalating demand for care in EDs and ensure that patients are seen based on the severity of their clinical condition rather than their order of arrival. This structured approach helps in making rapid, critical decisions, which in turn leads to improved patient outcomes, reduced waiting times, and optimised resource allocation.
2. How does the MTS classify patients, and what are its key features?
The MTS classifies patients into one of five distinct priority levels, each represented by a specific colour and associated with a target maximum waiting time for physician attention. These levels are:
Red (Immediate): Requires immediate care.
Orange (Very Urgent): Target waiting time of 10 minutes.
Yellow (Urgent): Target waiting time of 60 minutes.
Green (Standard): Target waiting time of 2 hours.
Blue (Non-Urgent): Target waiting time of 4 hours.
The system's methodology relies on trained healthcare professionals who use 52 or 53 predefined flowchart diagrams. These flowcharts correspond to specific reasons for encounter and incorporate 'decision points' or 'discriminators' – key symptoms or signs that guide the nurse in determining the urgency level. A critical safety feature is its "reductive system" methodology, which initially presumes a patient's condition is potentially life-threatening. Triage nurses must systematically rule out all high-priority discriminators before assigning a lower priority, inherently biasing the system towards patient safety and minimising undertriage, even if it may contribute to overtriage. While MTS provides a structured framework to reduce variability, its effective application ultimately requires the nuanced clinical judgment of a trained professional, making it a tool that augments, rather than replaces, human expertise.
3. How reliable and valid is the Manchester Triage System?
Studies consistently report a wide range of inter-rater reliability for MTS, generally falling into the "moderate" to "substantial" range, with kappa values typically between 0.41 and 0.80. Test-retest reliability is also reported as high.
In terms of predictive validity, MTS effectively distinguishes between patients with high versus low unadjusted risk of short-term death and those requiring hospitalisation. While the National Early Warning Score (NEWS) showed superior predictive accuracy for 30-day mortality, MTS significantly outperformed NEWS in predicting hospitalisation, ICU admission, life-saving interventions, and physician-defined clinical priority and severity. This indicates that MTS is primarily designed for initial risk stratification and resource allocation based on presenting symptoms, rather than a long-term prognostic tool.
However, significant concerns exist regarding undertriage and overtriage rates. Undertriage (assigning a lower urgency than warranted) is reported around 0.9% to 15%, but when it occurs, it is deemed clinically severe in over 50% of cases, particularly in infants under three months. Overtriage (assigning a higher urgency than warranted) is more frequent, ranging from 25.3% to 54%, with a particular prevalence in elderly patients and children. MTS also exhibits low sensitivity in predicting higher urgency levels generally.
4. What are the main challenges and limitations associated with MTS implementation?
The challenges with MTS extend beyond its algorithmic design and include:
Human Error and Cognitive Biases: Triage nurses operate under immense pressure, leading to potential errors. Personal judgments and biases can influence decisions, and patients may understate symptoms. The "experience paradox" suggests that, in simulated scenarios, more experienced nurses may even show higher error rates, possibly due to over-reliance on intuition rather than strict protocol adherence.
Resource Constraints and Bottlenecks: Limited staff and resources, common in EDs, can lead to delays even with accurate triage. Peak times and large-scale emergencies can overwhelm the system, creating significant patient flow bottlenecks.
Lack of Standardised Application and Updates: Despite widespread use, there is "no standard for its application, nor significant evidence of its benefits" in some contexts, leading to variability in implementation. The system has also seen minimal substantial updates over time, despite increasing scientific evidence.
Specific Challenges in Diverse Patient Populations: MTS struggles with accuracy in certain groups. It shows only moderate sensitivity and specificity in paediatric patients, with high rates of both overtriage (54%) and undertriage (12%), especially in infants. For geriatric patients, the system may not fully screen severe acute illness, leading to frequent overtriage. In neurological problems, such as Transient Global Amnesia or headaches with warning signs, MTS has shown an inability to correctly stratify, frequently leading to misclassification.
Communication Gaps: Patients desire better communication regarding their triage status and waiting times, and displaying time targets for staff may inadvertently create "false incentives," impacting care quality.
5. What strategies can be used to optimise the Manchester Triage System?
To enhance MTS effectiveness, a multi-faceted approach is essential:
Enhancing Training and Capacity Building: Comprehensive, ongoing training is crucial for all triage staff, including experienced nurses, to reinforce algorithmic adherence, mitigate biases, and improve decision-making. Objective analysis tools like video review can provide targeted feedback.
Leveraging Technological Tools: Adopting electronic triage systems, AI-powered solutions (e.g., KATE for accuracy), and seamless integration with Electronic Health Records (EHRs) can standardise processes, reduce human errors, streamline documentation, and provide real-time data. Digital check-in kiosks can also automate administrative tasks.
Implementing Nurse-Initiated Care Pathways and Rapid Assessment Zones (RATZs): Empowering nurses to initiate diagnostic tests, treatments, and referrals without immediate physician input, and establishing RATZs, can reduce wait times, improve patient satisfaction, and enhance ED efficiency.
Improving Staffing Levels and Resource Allocation: Ensuring adequate staffing, particularly during peak periods, and utilising performance-oriented staff planning based on patient engagement time data (categorised by MTS levels) can objectively calculate and adjust nursing staff requirements.
Continuous Performance Monitoring and Feedback Loops: Implementing real-time data analytics, regularly reviewing and adjusting triage criteria (especially for challenging patient groups like headache patients), and establishing a formal governance structure for MTS ensure ongoing review, auditing, and updates for safety and relevance.
6. How does the Manchester Triage System compare to other major triage systems like ESI, CTAS, and ATS?
The MTS is one of several prominent five-level triage systems globally, alongside the Emergency Severity Index (ESI), Canadian Triage and Acuity Scale (CTAS), and Australasian Triage Scale (ATS). Five-level systems are generally superior to three-level systems in validity and reliability.
Reliability: ESI and CTAS generally demonstrate good to excellent interobserver reliability (kappa values often 0.68-0.91), while MTS is typically reported as "moderate" to "substantial" (0.31-0.62). ATS shows adequate to satisfactory reliability (0.25-0.56).
Methodology: MTS is a symptom-driven, flowchart-based "reductive system." ESI is resource-based, determining priority on disease severity and anticipated resource needs. CTAS is an adaptation of ATS, using an extensive list of complaints, vital parameters, and high-risk factors, with mandated re-triage. ATS is a five-point system with defined time limits for physician evaluation.
Strengths: MTS is widely used in the UK/Europe, structured, and can reduce length of stay for trauma patients. ESI is good for identifying life-threatening conditions and has good validity in specific groups. CTAS is recognised for outstanding validity/reliability, mandatory documentation, and supporting nurse-led triage. ATS has defined time limits and correlates with admission/mortality.
Weaknesses: MTS has persistent issues with undertriage/overtriage, especially in paediatrics and geriatrics, and faces a lack of standardised application and minimal updates. ESI lacks fixed time limits for low-priority patients. CTAS can show moderate reliability for first-time users. ATS lacks prospective reliability assessment and shows low reliability in psychiatric patients.
A key distinction is MTS's symptom-driven approach versus ESI's resource-driven approach. While MTS can be efficient for patient flow, ESI's focus on resources can sometimes lead to more patients being routed to the main ED, potentially increasing congestion.
7. What are the real-world impacts and outcomes of applying the Manchester Triage System?
The Manchester Triage System has a tangible positive impact on emergency care operations and patient outcomes:
Patient Flow and Waiting Times: MTS is designed to effectively reduce queues in EDs by prioritising patients based on clinical severity rather than arrival order. This rapid assessment and prioritisation significantly reduces the time to identify and initiate treatment for critically ill patients, leading to improved survival rates and reduced long-term health complications. It optimises patient flow, ensuring resources are efficiently allocated and timely care is provided, thereby reducing waiting times.
Resource Allocation and Efficiency: By minimising variability in clinical decision-making, MTS ensures consistent application of guidelines, leading to more predictable patient experiences. Its ability to categorise patients by urgency allows for more efficient use of available resources, as studies confirm it is a helpful tool for improving resource allocation. It also enhances the quality of nurses' clinical evaluations.
Improved Patient Outcomes: The fundamental goal of MTS is to improve patient outcomes by ensuring the most critical needs are addressed first. Research consistently shows it significantly reduces treatment time for critically ill patients, leading to better survival. It has proven reliable in forecasting ED visits and short-term mortality, and for trauma patients, it has significantly reduced the length of care in the emergency unit. Studies indicate high accuracy in patient risk classification, with high correlation between urgency ratings and later medical diagnoses, and provides a high level of safety for severe illnesses, particularly for conditions requiring immediate attention like Acute Coronary Syndrome or respiratory symptoms.
8. Why is continuous adaptation and validation important for the Manchester Triage System?
Continuous adaptation and validation are crucial for MTS because, despite its effectiveness, it faces inherent challenges that can impact its accuracy and safety in diverse contexts. The "experience paradox" (where experienced nurses may make more errors in simulations) highlights that even a well-designed system can be undermined by human factors and the need for ongoing training to reinforce algorithmic adherence.
Furthermore, the system's "one-size-fits-all" approach is a significant limitation, especially for nuanced patient groups like paediatrics, geriatrics, and those with specific neurological conditions, where it consistently leads to misclassification (undertriage or overtriage). This necessitates the development of specialised, adapted protocols or supplementary tools within the existing MTS framework to improve accuracy and patient safety for these vulnerable populations.
The existence of "modified translations" (e.g., German versions) with potentially unfamiliar concepts and a notable absence of published validity and reliability data for these adapted versions poses a significant risk. This underscores that a triage system, even if effective in its original context, is not universally applicable without rigorous adaptation and re-validation for different patient demographics, cultural contexts, and language translations. The absence of such validation can compromise patient safety and system effectiveness. Therefore, continuous localised research, auditing, and validation studies are essential to ensure MTS remains safe, up-to-date, and relevant to current clinical practice and its specific implementation environment.
Additional Resources
Manchester Triage System Validity Study
German Version of the Manchester Triage System
Manchester Triage System in Pediatric Emergency Care
