Essential Triage Process: A Step-by-Step Guide to Emergency Medical Sorting
Discover the essential triage process used in emergency medicine, including assessment protocols, priority categorization, and modern technologies that are revolutionizing patient sorting and care prioritization.


Triage is a fundamental process in emergency medicine, defined as the systematic sorting and categorization of patients based on the clinical severity of their conditions. Its core objective is to maximize positive outcomes for the largest number of patients, particularly when medical resources are limited. This critical methodology is applied globally across diverse medical environments, ranging from a patient's initial arrival at a medical facility to the complex scenarios presented by mass casualty incidents (MCIs). The term "triage" itself is derived from the French verb "trier," meaning "to sort out".
The consistent emphasis on "limited resources" and the goal to "maximize results for most patients" or "maximize the number of survivors" underscores that triage extends beyond a mere clinical assessment. It represents a strategic approach to resource allocation. This perspective highlights that triage is not simply a diagnostic step but a dynamic resource management tool. Its effective application is crucial for achieving operational efficiency and ensuring the ethical distribution of scarce resources, especially in high-demand environments such as emergency departments (EDs) or disaster zones. Consequently, proficient triage directly influences system capacity and overall public health outcomes, transcending the scope of individual patient care.
Purpose and Importance in Healthcare Settings
The primary purpose of triage is to prioritize patients for emergency medical attention, thereby ensuring that individuals with life-threatening conditions receive immediate care. It is considered an "inseparable part of emergency management in hospitals" and serves as a vital index for assessing and validating the quality of emergency services. The ultimate aim of triage is to deliver the most appropriate clinical care to the largest possible number of patients within the shortest feasible timeframe.
Effective and prompt triage significantly enhances patient outcomes. It achieves this by increasing the overall quality of patient care services, substantially reducing waiting times, decreasing the average patient length of stay in the emergency department, lowering mortality rates, and ultimately contributing to reduced treatment costs. Conversely, inefficient or incorrect triage can lead to severe consequences, including ED overcrowding, delays in patient transfer to appropriate care areas, and considerable dissatisfaction among patients and their families. The explicit connection between accurate and timely triage and improved patient care quality, reduced waiting times, decreased mortality, and lower costs indicates that triage is not just a basic sorting mechanism but a critical determinant of core healthcare performance indicators. This elevates triage to a foundational pillar of patient safety and quality assurance in emergency medicine, making its efficacy a direct measure of an emergency department's operational health and its capacity to deliver timely and effective care.
Historical Context and Evolution of Triage
The concept of emergency triage has deep roots in military medicine, where it first emerged as a method for field doctors to prioritize the treatment of wounded soldiers during conflicts. Its practice dates back to historical events such as the Napoleonic Wars, demonstrating its long-standing utility in crisis situations. From these origins, triage has evolved into a "tried and true method" that is now universally applied in diverse scenarios worldwide, encompassing everything from the initial arrival of patients at medical facilities to large-scale mass casualty incidents. Over the decades, various adaptations and updates to triage tools and methodologies have been developed to meet evolving medical needs and challenges.
The historical transition of triage from a military necessity to a widespread civilian standard in hospitals and emergency services highlights a profound recognition of universal principles concerning resource scarcity and the imperative for prioritization during crises, irrespective of their origin. This trajectory reveals that triage's fundamental role in crisis management, aimed at maximizing survivability under extreme resource constraints, has been adapted for civilian healthcare. This adaptation acknowledges that even in routine operations, emergency departments frequently encounter resource limitations that necessitate a similar, albeit refined, strategic approach to patient allocation. This historical development underscores the enduring relevance of triage principles in any high-demand, resource-constrained medical environment.
II. Foundational Principles of Emergency Triage
Prioritization for Maximizing Outcomes with Limited Resources
At its core, triage involves the systematic sorting of patients based on their clinical severity, with the overarching goal of maximizing positive outcomes for the greatest number of individuals, particularly when resources are constrained. This principle becomes acutely critical during mass casualty incidents (MCIs), where human and material resources are, by definition, inherently insufficient to meet the overwhelming demand. In such scenarios, the focus shifts from providing optimal care to every individual to strategically identifying and treating those patients who are most likely to benefit from medical intervention, thereby optimizing the overall number of survivors.
The consistent emphasis on "maximizing results for most patients" and "maximizing the number of survivors" directly aligns with the utilitarian ethical principle of achieving the greatest good for the greatest number. This perspective indicates a systemic, rather than purely individual, approach to patient care in these contexts. This implies that the foundational principle of triage is deeply rooted in a utilitarian ethical framework, which prioritizes collective benefit over individual entitlement in situations of scarcity. Consequently, triage decisions, especially during MCIs, are inherently ethical dilemmas that necessitate a departure from typical individual-focused medical care towards a population-level strategy. Understanding this shift is crucial for comprehending the rationale behind potentially difficult allocation choices.
The Dynamic Nature of Triage: Continuous Reassessment
Triage is not a static, one-time assessment but a highly dynamic process. A patient's clinical status can change rapidly over time, necessitating continuous reassessment to ensure their assigned priority remains accurate and appropriate. Patients may undergo multiple stages of triage throughout their journey through the healthcare system. This includes initial triage upon arrival at a medical facility, subsequent triage before transfer to other treatment areas or different facilities (often referred to as evacuation triage), and yet another triage process upon arrival at a higher level of care. For example, evacuation triage specifically focuses on prioritizing the movement of patients to the next appropriate care level rather than initiating new treatments, as these patients are presumed to be already receiving medical care.
The description of triage as a "dynamic process" and the imperative for "continuous reassessment" highlight that a single initial evaluation is insufficient to manage evolving patient conditions. This understanding implies that a rigid approach to triage, failing to account for changes in patient status, can lead to suboptimal outcomes. Therefore, triage is an ongoing, adaptive process. This necessitates that triage personnel possess a high degree of flexibility and critical thinking to adjust patient priorities as their conditions evolve or as available resources change. The ability to adapt and reassess is as crucial as the initial sorting, particularly in rapidly changing and unpredictable emergency environments.
Core Competencies and Skills for Triage Personnel
Effective triage hinges on the proficiency of the personnel performing it. Triage nurses, for instance, must possess a comprehensive set of professional capabilities. These include adequate knowledge of triage methodologies, extensive clinical experience, profound clinical knowledge in the physiopathology of various diseases and high-risk emergencies, and the practical skill to execute quick and accurate clinical measures. They must be adept at rapidly and accurately evaluating vital signs and conducting precise patient assessments.
Beyond clinical acumen, essential interpersonal and cognitive skills are paramount. These include excellent communication abilities, the capacity to remain calm and composed in high-stress situations, strong decision-making capabilities, and effective multitasking skills. Empathy and compassion are also vital attributes, enabling triage personnel to connect with patients facing difficult and frightening circumstances. The Manchester Triage System (MTS) explicitly emphasizes that it should be utilized by the "most, rather than the least experienced personnel" within a department. Similarly, the Emergency Severity Index (ESI) is specifically designed for nurses with established emergency nursing and triage experience.
The consistent emphasis on "professional capabilities," "clinical experience," "sufficient clinical knowledge," and "clinical skill" , coupled with the recommendation for MTS to be used by the "most experienced personnel" , indicates that triage expertise extends far beyond simply following an algorithm. This suggests that effective triage is an art form requiring seasoned clinical judgment, critical thinking, and the ability to synthesize complex information under immense pressure. This highlights the indispensable role of human expertise, even when sophisticated tools are available, and underscores the profound need for robust training, ongoing education, and mentorship programs to cultivate these advanced competencies in emergency medical professionals.
III. The Triage Process: A Step-by-Step Guide to Assessment and Categorization
Initial Patient Contact and Information Gathering
The triage process initiates the moment a patient arrives, ideally before any administrative procedures such as registration are undertaken. In an emergency department, nurses are typically the first point of contact, responsible for gathering crucial information from patients and their families to inform subsequent care decisions. This initial data collection includes the patient's chief complaint, a comprehensive set of vital signs, and their pertinent medical history, encompassing pre-existing conditions and known allergies.
The instruction that triage should occur "as soon as a sick child arrives, before any administrative procedure" , alongside the Simple Triage And Rapid Treatment (START) system's objective of calculating triage status in "less than 60 seconds" , underscores the extreme time sensitivity of this initial assessment phase. This highlights that the initial moments of patient contact are a "golden minute" for triage, where rapid information gathering and assessment are paramount. Any delays at this stage, even for seemingly routine administrative tasks, can critically compromise patient outcomes, particularly for those presenting with high-acuity conditions. This necessitates streamlined intake processes and the deployment of highly skilled personnel at the very first point of patient contact.
Rapid Assessment Techniques: Airway, Breathing, Circulation (ABC/CAB) and Mental Status
A cornerstone of emergency triage is the rapid assessment of vital physiological functions. Medical experts universally agree that the immediate priority for assessment and intervention across all types of injuries and illnesses is the airway, followed by breathing, and then circulation (ABC). While this sequence remains standard, for adult cardiac arrest, the protocol may shift to compressions first (CAB), though for hypoxic adult arrests and pediatric arrests, airway and breathing maintain their primary importance.
In the context of trauma triage, the primary survey is systematically based on the 'ABCDE' resuscitation system: Airway control, which includes stabilization of the cervical spine; Breathing, assessing the adequacy of ventilation; Circulation, focusing on effective blood flow and control of external hemorrhage; Disability, evaluating neurological status; and Exposure, involving complete undressing of the patient while preventing hypothermia. For pediatric patients, initial emergency assessments specifically look for signs related to airway or breathing problems, indications of shock or severe dehydration, and altered consciousness or convulsions. The AVPU scale (Alert, Voice, Pain, Unconscious) is a widely used tool to quickly ascertain a child's level of consciousness. The START triage system, designed for mass casualty incidents, similarly relies on the rapid assessment of RPM: Respirations, Pulse/Perfusion, and Mental Status.
The consistent and fundamental focus across various triage contexts—be it pre-hospital, in-hospital, for adults, or for pediatric patients—on physiological parameters related to life-sustaining functions such as airway, breathing, circulation, and mental status (ABC/CAB, RPM, AVPU, GCS) signifies their universal importance. This recurring pattern demonstrates that despite variations in specific algorithms and patient demographics, the immediate assessment of fundamental physiological stability remains the bedrock of emergency triage. This highlights that regardless of the incident type or the patient's age, the most immediate threat to life is always prioritized through the evaluation of these core physiological indicators.
Sequential Steps in Patient Evaluation
The triage process is inherently a systematic approach designed to efficiently evaluate and categorize patients. In the START system, the initial step involves identifying the "walking wounded" (those with minor injuries) by instructing them to move to a designated safe area. Following this, non-ambulatory patients are assessed. A crucial, and often the only, intervention performed before declaring a patient deceased is an attempt to open their airway. Patients who are breathing are then further evaluated using the RPM (Respirations, Pulse/Perfusion, Mental Status) criteria.
The Emergency Severity Index (ESI) algorithm, commonly used in emergency departments, follows a structured sequence of four decision points:
Decision Point A: Is the patient unstable and in need of immediate lifesaving intervention?
Decision Point B: Is this a high-risk situation, is the patient likely to deteriorate, or do they have new onset altered mental status or severe pain/distress?
Decision Point C: How many resources will this patient need for the provider to reach a disposition decision?
Decision Point D: Do the patient's vital signs warrant a reassessment of the acuity level?
These decision points must be performed in order, with higher acuity patients often requiring only one or two points for categorization. Similarly, the Manchester Triage System (MTS) involves an immediate assessment upon patient arrival, which then leads to the allocation of a specific time window for the patient's first physician contact. This allocation is based on the association of symptoms with urgency levels, typically using an ABCDE scheme.
The explicit sequential decision points embedded in systems like START and ESI demonstrate a deliberate design choice to guide decision-makers through complex scenarios, especially under pressure. This structured, step-by-step approach represents a critical evolution in triage, moving from purely intuitive judgment to a more standardized, efficient, and reproducible process. This systematic methodology aims to reduce cognitive load on triage personnel and enhance consistency in patient prioritization, which is particularly beneficial in high-volume or high-stress emergency environments.
Categorization and Acuity Assignment
Following assessment, patients are categorized into priority levels based on the severity of their condition, which directly guides the order in which they receive medical care. Different triage systems employ distinct categorization frameworks tailored to their specific operational contexts.
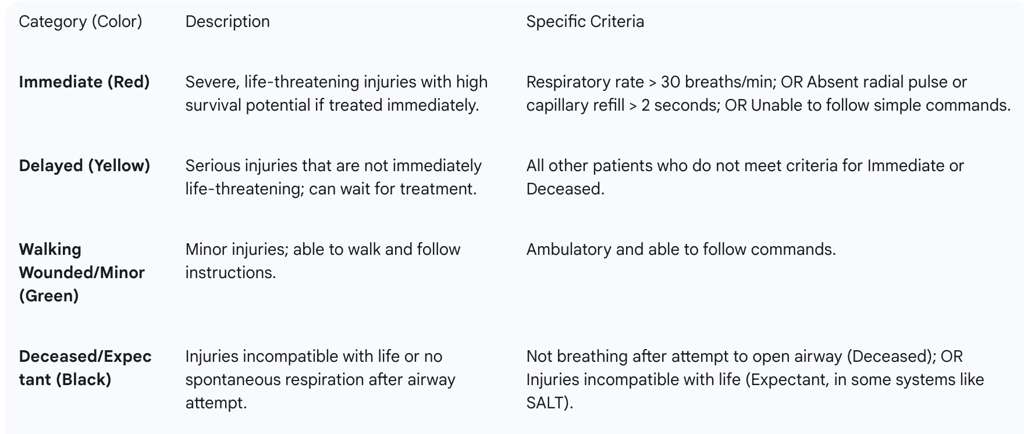
START/Mass Casualty Categories: Designed for mass casualty incidents, the START system uses a four-tier color-coded categorization:
Red (Immediate): This category is assigned to patients with severe, life-threatening injuries who possess a high potential for survival if they receive immediate treatment. Specific criteria for this classification include a respiratory rate greater than 30 breaths per minute, an absent radial pulse or a capillary refill time exceeding 2 seconds, or an inability to follow simple commands.
Yellow (Delayed): Patients in this category have serious injuries that are not immediately life-threatening, meaning their treatment can be safely delayed until more critical patients have been addressed.
Green (Walking Wounded/Minor): This group comprises individuals with minor injuries who are ambulatory and able to follow instructions.
Black (Deceased/Expectant): This category is reserved for individuals with injuries deemed incompatible with life or those who do not exhibit spontaneous respiration even after an attempt to open their airway. The SALT system further refines this by including an "expectant" category for patients with a low likelihood of survival given the available resources.
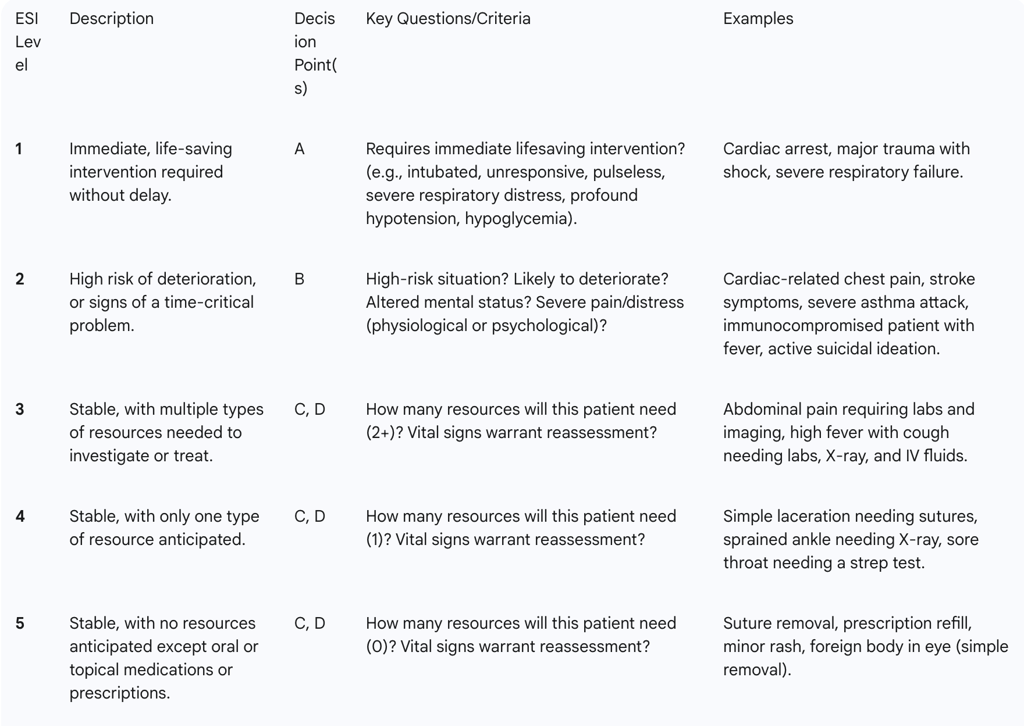
ESI/Emergency Department Categories: The Emergency Severity Index (ESI) is a widely adopted five-level algorithm used primarily in emergency departments, ranging from Level 1 (most urgent) to Level 5 (least urgent).
Level 1 (Resuscitation): These patients require immediate, life-saving interventions without any delay. Examples include patients in cardiac arrest, those who are unresponsive, or individuals presenting with profound hypotension or hypoglycemia.
Level 2 (Emergent/High Risk): This category includes patients at high risk of deterioration, those with time-critical problems, new onset altered mental status, or severe pain/distress. Examples typically involve cardiac-related chest pain or acute asthma attacks.
Level 3 (Urgent): Patients are stable but are anticipated to require multiple types of resources for investigation or treatment. Abdominal pain is a common example.
Level 4 (Semi-Urgent): These patients are stable and are expected to require only one type of resource. A simple laceration requiring sutures is a typical example.
Level 5 (Non-Urgent): This category is for stable patients who are not anticipated to require any resources beyond oral medications or prescriptions. Suture removal or prescription refills are common scenarios.
The clear distinction between START/SALT (color-coded, MCI-focused, emphasizing immediate survival and evacuation) and ESI (numerical levels, ED-focused, incorporating resource needs) is explicitly noted, with ESI specified as
not suitable for MCIs. This difference highlights that the most appropriate categorization system is critically dependent on the operational context (e.g., mass casualty event versus daily emergency department operations) and the availability of resources. This underscores the importance of training personnel in the specific triage system applicable to their environment to prevent mis-triage and optimize patient outcomes.
IV. Key Triage Systems in Practice
A. Mass Casualty Incident (MCI) Triage Systems
Triage during a Mass Casualty Incident (MCI) fundamentally differs from routine daily triage due to the inherent potential for severe resource limitations. In these overwhelming situations, the primary objective of triage shifts to the rapid identification and prioritization of individuals who are in immediate need of life-saving interventions.
1. Simple Triage And Rapid Treatment (START)
The START system was developed in 1983 by the staff of Hoag Hospital and the Newport Beach Fire Department in California. It is widely adopted across the United States for initial triage in MCIs. The primary goal of START is to classify victims quickly, ideally within 60 seconds, based on the severity of their injuries.
The process begins by instructing all ambulatory patients to move to a designated safe area, immediately classifying them as "Green" or "Minor". Following this, non-ambulatory patients are assessed. The only medical intervention typically performed before declaring a patient deceased is an attempt to open their airway. Patients who are breathing are then evaluated using the RPM mnemonic: Respirations, Perfusion, and Mental Status.
The design of START emphasizes "simplicity" and the rapid classification of victims, aiming for completion in "less than 60 seconds". This focus on speed and ease of use is a deliberate design choice, enabling the system to function effectively in the chaotic, high-stress, and resource-constrained environments characteristic of MCIs. This highlights a conscious trade-off between achieving granular diagnostic precision and ensuring operational efficiency under extreme conditions, where rapid sorting to identify the most critical and salvageable patients is paramount.
2. JumpSTART for Pediatric Patients
JumpSTART is a crucial modification of the START system specifically designed for pediatric patients, typically those between 1 and 8 years old. This adaptation is necessary because children have unique physiological responses and developmental differences compared to adults, including an increased likelihood of respiratory failure and potential inability to follow verbal commands.
A key modification in JumpSTART involves different "normal" respiratory rate ranges; for instance, a child may be classified as "immediate" if their respiration rate is below 15 or above 45 breaths per minute. For an apneic pediatric patient who still has a pulse, the protocol dictates giving 5 rescue breaths; if breathing resumes, the child is tagged as "immediate," but if breathing does not resume, they are classified as "deceased". Infants under 12 months are generally marked as "IMMEDIATE".
JumpSTART's specific modifications for children, such as adjusted respiratory rate thresholds and the protocol for apneic pediatric patients with a pulse , directly address the physiological and developmental differences in children compared to adults. This highlights a recognition that a "one-size-fits-all" approach to triage is inadequate when it comes to pediatric populations. This underscores the critical need for pediatric-specific training and specialized tools to accurately assess and prioritize children, thereby preventing undertriage that might result from applying adult-centric criteria and ensuring they receive appropriate life-saving interventions.
3. Sort-Assess-Lifesaving Interventions-Treatment/Transport (SALT)
The SALT system was developed in 2008 as an evidence-based, non-proprietary triage system, aiming for national standardization in all-hazards Mass Casualty Incidents. It defines criteria across four categories: general considerations, global sorting, lifesaving interventions, and the assignment of triage categories.
The SALT process involves a sequence of steps:
Sort: Victims are initially sorted based on their ability to walk, wave, or if they are still.
Assess: An individual assessment is performed to determine the need for immediate life-saving interventions (LSI).
Lifesaving Interventions: Critical interventions such as controlling severe hemorrhage or opening an airway are performed at this stage.
Treatment/Transport: Patients are then directed for definitive treatment or transport.
A key distinction between SALT and START is that SALT incorporates an internal question to differentiate between "immediate" and "expectant" categories: "Is the patient likely to survive the current circumstance given the resources available?". If the answer is no, the patient is deemed expectant, providing a "grey area" for flexibility in decision-making under severe resource constraints.
SALT's unique question, "Is the patient likely to survive the current circumstance given the resources available?" , explicitly introduces the factor of resource scarcity into the triage decision. This pragmatic consideration is vital in MCIs, moving beyond a purely clinical assessment to incorporate operational realities. This represents an evolution in MCI triage by integrating resource availability directly into the prioritization decision. The system aims to optimize overall outcomes not solely based on the severity of injuries but also on the realistic potential for successful intervention given the immediate and limited resources at hand.
B. Emergency Department (ED) Triage Systems
1. Emergency Severity Index (ESI): A Five-Level Algorithm
The Emergency Severity Index (ESI) is a widely adopted five-level triage algorithm used in emergency departments. It was initially developed in 1998 by emergency physicians Richard Wuerz and David Eitel and is now maintained by the Emergency Nurses Association (ENA). As of 2019, ESI was the most commonly used triage system in US EDs, utilized by 94% of facilities.
The ESI system categorizes patients not only by their acuity (severity of medical condition) but also by their anticipated resource needs. This dual focus is crucial for efficient patient flow and resource allocation within the ED. The ESI algorithm is structured around four decision points (A, B, C, D) that must be performed sequentially. Higher acuity patients typically require only one or two decision points for their acuity level to be assigned.
The explicit incorporation of "anticipated resource needs" into ESI's categorization, particularly for levels 3-5, distinguishes it significantly from MCI systems that primarily focus on immediate life threat and evacuation. This emphasis on resources indicates a crucial aim to optimize ED operations. This means ESI is designed not just for clinical prioritization but also as a sophisticated patient flow management tool within the ED. By anticipating resource consumption, it facilitates a more efficient allocation of staff, diagnostic services, and treatment spaces, directly impacting patient throughput and reducing waiting times. This highlights the system's shift from pure patient "sorting" to integrated operational management.
The ESI algorithm guides triage nurses through a series of questions to assign an acuity level:
2. Manchester Triage System (MTS): A Clinical Risk Management Tool
The Manchester Triage System (MTS) is prevalent in Europe and functions as a clinical risk management tool. Its purpose is to assess patient urgency and safely manage patient flow, particularly when clinical demand surpasses available capacity. The procedure involves an immediate assessment upon a patient's arrival, which then leads to the assignment of a time window for their first physician contact.
MTS utilizes 53 presentation-based charts rather than diagnosis-based ones, meaning the assessment focuses on what the patient reports is happening, not necessarily the underlying cause. These charts incorporate common names, discriminators (worsening symptoms or signs), and definitions to maintain consistency and facilitate robust auditing. The system is described as a "reductive system," meaning it starts with the premise that the patient is presenting with a life-threatening condition. All high-priority discriminators must be systematically ruled out before the patient's priority can be lowered.
The description of MTS as a "reductive system, starting from the premise that the patient is presenting with a life threatening condition and all high priority discriminators must be ruled out prior to reducing the patient priority" reveals a built-in safety mechanism. This approach prioritizes avoiding missed critical conditions. This implies that MTS embodies a highly risk-averse approach, prioritizing patient safety by defaulting to the highest acuity until proven otherwise. This "rule-out" methodology minimizes the chance of undertriage for critical conditions, even if it might lead to some overtriage, reflecting a strong emphasis on preventing adverse events.
3. Brief Overview of Other Systems (ATS, CTAS, CHT)
Beyond START, SALT, ESI, and MTS, several other prominent triage systems are utilized globally, each with its own nuances:
Australasian Triage Scale (ATS): Adopted as the national triage scale in Australia in 1993, ATS is a 5-level categorical scale. It integrates presenting patient problems, appearance, and pertinent physiological findings, guided by 79 clinical descriptors. Its primary focus is on determining how long a patient can safely wait for care.
Canadian Triage and Acuity Scale (CTAS): This is another 5-level system that bases acuity on illness severity or the time required before medical intervention. It is combined with a standardized list of patient complaints and includes "first-order" and "second-order" modifiers that allow for adjustments to the initial acuity level based on additional clinical factors.
Chinese Four-level and Three District Triage Standard (CHT): Drafted in 2011, the CHT system categorizes patients into four acuity levels. It then sorts these patients into three distinct treatment zones: a Red Zone for critically ill patients requiring resuscitation, a Yellow Zone for emergent cases, and a Green Zone for non-emergent patients.
The observation that multiple prominent triage systems—including ESI, MTS, ATS, CTAS, and CHT—converge on a multi-level (typically four or five levels) categorization approach , despite originating in different regions, suggests a global consensus on the necessity for nuanced patient stratification beyond a simple emergent/non-emergent distinction. This widespread adoption indicates a recognized best practice for managing patient flow and acuity. The convergence implies that a more granular classification is crucial for optimizing resource allocation and patient outcomes across diverse healthcare systems, reflecting a shared understanding of the inherent complexities in emergency care.
V. Prioritization Criteria and Physiological Indicators
Utilizing Vital Signs and Clinical Presentation
Triage decisions are heavily dependent on a comprehensive evaluation of a patient's vital signs and their overall clinical presentation. Key vital signs considered include heart rate, blood pressure, respiratory rate, oxygen saturation, and temperature. Clinical presentation encompasses factors such as the patient's reported pain level, observable signs of distress, any altered mental status, and overt signs of respiratory distress.
The Emergency Severity Index (ESI) specifically incorporates a "Decision Point D" to utilize vital signs for identifying "well-appearing ill" patients—individuals who may appear stable but whose physiological parameters indicate underlying instability warranting a higher acuity level. It is crucial that vital signs are not interpreted in isolation but are contextualized with the patient's medical history, current medications (e.g., beta-blockers, corticosteroids), and their specific presenting complaint. For instance, a seemingly "normal" vital sign might be abnormal for a specific patient, such as a child whose age-adjusted respiratory rate is outside the expected range, or an elderly patient whose baseline blood pressure is significantly lower than average.
The emphasis in ESI's Decision Point D that vital signs are not just absolute numbers but must be interpreted within context (e.g., age-adjusted pediatric ranges, patient's baseline, medications) highlights a critical nuance. This implies that a seemingly "normal" vital sign could, in fact, be abnormal for a specific patient, necessitating experienced clinical judgment. This underscores that triage is not a simple checklist of absolute vital sign thresholds. Instead, it requires sophisticated interpretation of physiological data within the context of the patient's age, medical history, and presenting complaint. This capability is essential for comprehensive clinical knowledge and the ability to detect subtle, yet critical, signs of deterioration, particularly in vulnerable populations like children or the elderly.
Assessing Injury Severity and Anticipating Resource Needs
A primary function of triage is to accurately categorize patients based on the severity of their injuries or illness. In the ESI system, levels 3, 4, and 5 are differentiated primarily by the anticipated number of resources a patient will likely need for the healthcare provider to reach a disposition decision (e.g., discharge, admission, transfer).
The term "resources" in the ESI framework specifically refers to types of interventions or diagnostic tools that extend beyond a basic physical examination. Examples include laboratory tests (blood, urine), diagnostic imaging (X-rays, CT scans, MRIs, ultrasounds), intravenous (IV) or intramuscular (IM) medications, nebulized medications, specialty consultations, and various procedures (e.g., laceration repair, complex procedures like procedural sedation). Conversely, certain common interventions are explicitly not considered ESI resources. These include oral medications, simple wound care (e.g., dressings, rechecks), crutches, splints, and prescriptions.
The explicit requirement in ESI for nurses to "anticipate the number of resources" a patient will need elevates triage beyond immediate assessment to a predictive judgment. This predictive skill is based on clinical knowledge and experience regarding typical patient pathways for various conditions. This implies that anticipating resource needs transforms triage into a predictive diagnostic skill, demanding that nurses not only assess current acuity but also project the likely investigative and therapeutic trajectory. This capability is crucial for ensuring efficient patient flow and optimal resource utilization within the emergency department, thereby moving beyond immediate crisis management to strategic operational planning.
Trauma Scoring Systems (e.g., GCS, RTS, ISS)
Trauma scoring systems are specialized tools primarily utilized in audit and research to study the outcomes of trauma and trauma care, rather than for predicting individual patient outcomes or for real-time triage decisions. These systems aid in quantifying injury severity for epidemiological purposes and quality improvement initiatives.
Physiological Scoring Systems:
Glasgow Coma Scale (GCS): This is a simple and widely used method to quantify the level of consciousness following traumatic brain injury. It is the sum of three parameters: Best Eye Response, Best Verbal Response, and Best Motor Response, with scores ranging from 3 (indicating the worst outcome) to 15 (indicating the best outcome).
Revised Trauma Score (RTS): Used as a triage tool in pre-hospital settings, RTS is a physiological scoring system based on initial data sets of three specific parameters: the GCS, systemic blood pressure (SBP), and respiratory rate (RR). A significant limitation of RTS is its inability to accurately score patients who are intubated and mechanically ventilated.
Acute Physiology and Chronic Health Evaluation (APACHE): This system is widely employed for assessing illness severity in intensive care units (ICUs).
Anatomical Scoring Systems:
Abbreviated Injury Scale (AIS): Introduced in 1969, AIS is designed to reflect the impact of a particular organ injury on patient outcome. Scores range from 1 (Minor) to 6 (Unsurvivable). However, AIS has limitations; it does not provide a comprehensive measure of overall severity and is not a linear scale, meaning the difference between scores (e.g., AIS1 and AIS2) is not uniform.
Injury Severity Score (ISS): Introduced in 1974, the ISS is considered the 'gold standard' for severity scoring in patients with multiple injuries. Each injury is assigned an AIS score and categorized into one of six body regions. The ISS is calculated by summing the squares of the three highest AIS scores, with the caveat that only one score from each body region may be included. Limitations include its unsuitability as a triage tool and its potential to underestimate severity in patients with multiple injuries within the same body region. The New Injury Severity Score (NISS) is a modified version that addresses some of these limitations.
Combination Scoring Systems:
Trauma and Injury Severity Score (TRISS): TRISS combines anatomical (ISS) and physiological (RTS) scores to determine the probability of patient survival (Ps) using a logarithmic regression equation.
The explicit statement that trauma scoring systems (GCS, RTS, ISS, TRISS) are primarily for "audit and research to study the outcomes of trauma and trauma care" rather than for "predicting individual patient outcomes" or for "triage" clearly delineates their purpose from immediate patient sorting. This highlights that while triage systems guide immediate patient sorting, trauma scoring systems serve a distinct, higher-level function in trauma care. They are primarily prognostic and evaluative tools used for quality improvement, research, and system-level performance assessment, rather than for real-time decision-making regarding individual patient prioritization. This distinction is crucial for understanding the different layers of assessment and management in emergency medicine.
VI. Challenges and Best Practices in Emergency Triage
Common Challenges: Uncertainty, Resource Limitations, Overcrowding, and Bias
Emergency medical triage, despite its structured methodologies, faces numerous inherent challenges that can complicate effective patient sorting and care delivery.
Uncertainty: Emergency situations are often characterized by significant uncertainty, including unpredictable events, unconfirmed or contradictory information, and inherent difficulties in accurately assessing the number of injured or affected individuals. This ambiguity can lead to frustration among responders and complicate the determination of whether a situation truly constitutes a mass casualty incident.
Mismatch with Contingency Plans: Pre-established disaster contingency plans may prove inadequate or inapplicable in real-world scenarios. This can occur if public behavior deviates from plan assumptions (e.g., spontaneous evacuation of injured individuals to hospitals rather than waiting for pre-hospital care), or if the event unfolds in an unforeseen direction. Furthermore, plans often focus heavily on severely injured patients, yet many incidents involve a large proportion of individuals requiring basic medical care or psychosocial support, needs that may not be adequately covered in existing protocols.
Resource Limitations & Overcrowding: Mass casualty incidents are, by definition, situations where a sudden surge in patients overwhelms the capacity of local medical resources. Beyond disasters, emergency department overcrowding is a widespread global problem, leading to extended waiting times, compromised quality of care, potential patient safety risks, impaired staff morale, and increased healthcare costs.
Bias: Triage decisions, despite structured algorithms, can unfortunately be influenced by implicit biases related to race, age, gender, behavioral health issues, or substance use. Such biases can lead to unequal access to healthcare and disparities in care delivery.
Lack of Clinical Competency: A significant challenge arises when triage nurses lack sufficient clinical knowledge and experience. This deficiency can lead to errors in prioritizing patients, which in turn contributes to ED overcrowding and patient dissatisfaction.
The pervasive challenges such as "uncertainty," "mismatch between contingency plan and reality," and "bias" highlight the significant cognitive, emotional, and systemic pressures exerted on triage personnel. The identified "lack of clinical competency" directly links to the potential for human error within these demanding conditions. This implies that the effectiveness of triage, despite the presence of standardized protocols, remains highly dependent on the human element. These challenges underscore the psychological burden and the potential for human error. Therefore, robust training in algorithms must be complemented by education in critical thinking, adaptability, and bias mitigation strategies to adequately support triage personnel in high-stakes, ambiguous environments.
Strategies for Ensuring Triage Accuracy and Consistency
To mitigate the challenges inherent in emergency triage and enhance its effectiveness, several best practices and strategies are crucial for ensuring accuracy and consistency.
Standardized Algorithms: The widespread adoption and consistent application of evidence-based, standardized triage systems, such as ESI, START, JumpSTART, SALT, and MTS, are paramount. These algorithms provide a structured framework for decision-making, reducing variability and promoting uniformity in patient categorization.
Continuous Reassessment: Recognizing the dynamic nature of patient conditions, continuous reassessment of a patient's status is essential. As conditions change or additional resources become available, triage categories must be re-evaluated and adjusted accordingly.
Quality Improvement Reviews: Regular and systematic quality improvement reviews are vital to monitor the effectiveness and consistency of implemented triage systems. These reviews help identify areas for improvement, refine protocols, and ensure adherence to best practices.
Ethical Justifications: Triage decisions, particularly in resource-limited settings, must be guided by clear ethical justifications. The overarching principle is to make decisions that save the largest number of lives, even if this necessitates altering individual care pathways.
While individual skills and judgment are undeniably critical , the strong emphasis on "standardized algorithms," "continuous reassessment," and "quality improvement reviews" points to the necessity of systemic solutions to support and enhance individual performance. This suggests that achieving high triage accuracy is not solely a function of individual capability but also of robust organizational infrastructure. This implies that healthcare organizations must invest significantly in these systemic supports to empower triage personnel and ensure optimal patient outcomes, recognizing that individual competence thrives within a well-supported framework.
Importance of Training, Education, and Adaptability
The proficiency of triage personnel is directly linked to the quality and depth of their training and education. While comprehensive educational programs can partially bridge knowledge gaps for inexperienced clinicians, they cannot fully replace the invaluable knowledge gained through direct clinical experience. Therefore, a blend of formal training and practical exposure is crucial.
For instance, triage nurses often require specific ESI training in addition to at least one year of emergency department experience to effectively apply the system. Furthermore, consistent training across different healthcare providers, including EMS personnel, nurses, and physicians, using the same common triage criteria, is vital for seamless transitions and effective hand-offs of patient care between pre-hospital and in-hospital settings. Beyond adherence to protocols, the ability to adapt to the current situation is paramount, as every emergency scenario is unique and may not unfold as anticipated.
The consistent need for "specific ESI training," "at least one year ED experience" , and the explicit statement that training "does not replace knowledge gained through clinical experience" indicate that triage expertise is not a static achievement but a continuous journey of learning and practical application. This implies that triage is a domain demanding continuous professional development and lifelong learning, extending beyond initial certification. The dynamic nature of emergencies and the continuous evolution of medical knowledge necessitate ongoing education, mentorship, and practical experience to maintain and enhance the critical skills required for accurate, adaptable, and ethically sound triage decisions. This highlights the significant and ongoing investment required in human capital for effective emergency response.
VII. Ethical Dimensions of Medical Triage
Balancing Individual Needs with the Collective Good
Triage is fundamentally an ethical process, particularly when resources are limited. This ethical imperative became acutely evident during the COVID-19 pandemic, where healthcare providers faced the difficult task of allocating scarce resources like ventilators. In such situations, triage requires healthcare providers to make profound decisions about who receives treatment and who does not, often with incomplete information and under immense pressure. The underlying reality is that in conditions of scarcity, it is simply not possible for everyone who needs a particular form of healthcare to gain immediate access to it.
The core tension in triage is explicitly identified as "balancing individual needs with the collective good" , particularly when resources are scarce. This represents a fundamental ethical dilemma, where the pursuit of utilitarian outcomes—saving the most lives—can directly conflict with the principle of individual patient advocacy. This implies that triage, especially in mass casualty or resource-scarce situations, is an inherently ethical minefield. The principle of saving the most lives (utilitarianism) can conflict with the principle of individual patient care (e.g., non-abandonment or the rescue principle). This necessitates the development of clear ethical guidelines and robust decision-making frameworks to navigate these profound moral dilemmas.
Addressing Biases and Ensuring Fairness and Transparency
A critical ethical challenge in triage is the potential for decisions to be influenced by biases, including those related to race, age, gender, behavioral health status, or substance use. Such biases can lead to unequal access to healthcare and disparities in treatment outcomes. To counteract these issues, it is imperative to implement fair and transparent triage policies that are explicitly designed to be free from bias and discrimination. The use of objective criteria, such as the Sequential Organ Failure Assessment (SOFA) score, can help guide triage decisions. The SOFA score is a widely used system that evaluates the severity of organ dysfunction in critically ill patients, providing a standardized, objective measure that can inform prioritization.
The explicit mention of "biases and discrimination" and the call for "fair and transparent" policies highlight that ethical triage extends beyond simply maximizing the number of lives saved; it also encompasses ensuring equitable treatment for all individuals. This points to justice as a critical, and often overlooked, dimension of triage. This implies that beyond optimizing outcomes, ethical triage must actively combat biases to ensure equitable access to care. Transparency in decision-making processes and the consistent use of objective scoring systems, like SOFA, are not merely best practices but ethical imperatives to uphold the principles of justice and prevent discrimination in high-stakes situations.
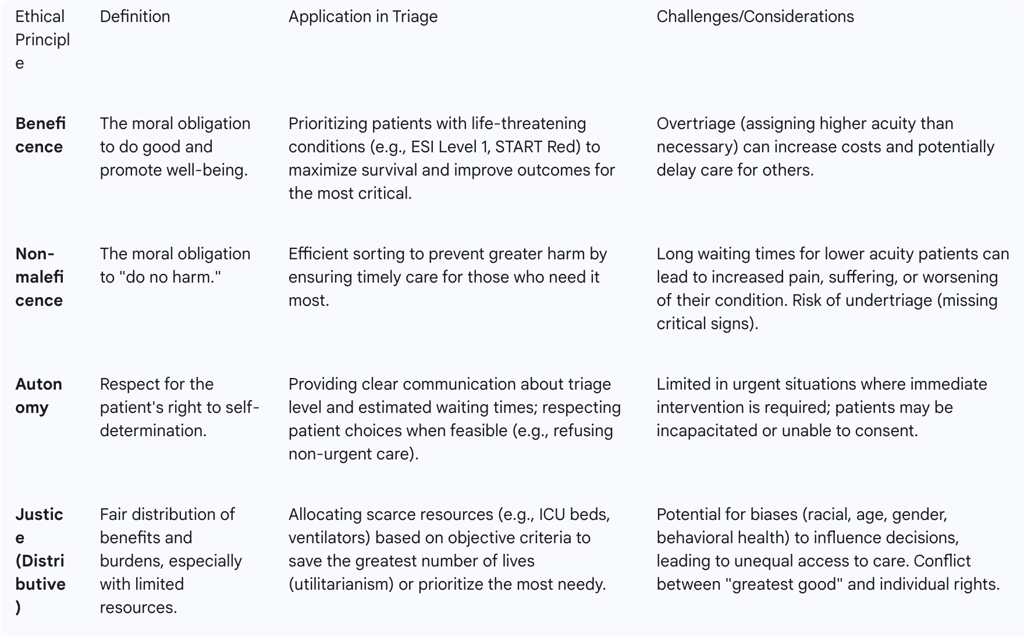
Ethical Principles Guiding Triage Decisions (Beneficence, Non-maleficence, Autonomy, Justice)
The ethical analysis of emergency department triage is guided by four foundational principles of biomedical ethics: beneficence, non-maleficence, autonomy, and justice. While these principles provide a crucial starting point for identifying ethical challenges, they alone may not offer a comprehensive ethical view, often presenting fragmented pieces of the triage puzzle.
Beneficence: This principle embodies the moral obligation to do good and promote the well-being of patients. In triage, beneficence guides the aim to improve the quality of care and preserve human lives by prioritizing those with immediate life-sustaining needs. The system strives to achieve the best possible outcome for the greatest number.
Non-maleficence: This principle dictates the moral obligation to "do no harm." While triage aims to prevent greater harm through efficient sorting, it can inadvertently cause indirect harm through prolonged waiting times, increased pain and suffering, or the worsening of conditions for those categorized as less urgent.
Autonomy: This principle respects the patient's right to self-determination and informed decision-making. While assessing and respecting autonomy can be challenging in urgent emergency department situations due to the immediate need for action, it is still considered. This involves clear and effective communication from triage officers, informing patients about their triage level and estimated waiting times to the extent possible.
Justice (Distributive Justice): This principle addresses how benefits and burdens should be distributed fairly within a population, particularly when resources are limited. It encompasses several sub-principles, including:
Equality: The idea that every person's life holds equal worth, and everyone should have an equal chance to receive necessary care.
Utility: The principle of achieving the greatest good for the greatest number, which serves as a primary rationale for triage systems in resource scarcity.
Priority to the Worst-Off: Prioritizing those with the most severe conditions, although this must be balanced against the likelihood of successful treatment to avoid inefficient resource allocation.
The observation that while these four principles are foundational, they "do not offer a comprehensive ethical view" and only provide "fragmented pieces of the triage puzzle" highlights the complexity of ethical decision-making in emergency medicine. This implies that ethical triage is not governed by a single principle but by a complex interplay of beneficence, non-maleficence, autonomy, and justice. Decision-makers must navigate the inherent tensions between these principles, especially when utilitarian goals (saving the most lives) conflict with individual rights or the desire to "do no harm" to a specific patient. This necessitates an integrated, clinically and ethically based framework for triage planning that considers the dynamic aspects of care.
To further illustrate the application and challenges of these principles in triage, the following table provides specific examples:
VIII. Conclusion and Recommendations for Enhanced Triage Processes
Summary of Key Learnings
Emergency medical triage stands as a cornerstone of effective healthcare delivery, fundamentally defined as the systematic sorting of patients based on clinical severity to optimize outcomes, particularly under resource constraints. This process is inherently dynamic, necessitating continuous reassessment as patient conditions evolve. Its historical roots in military medicine underscore its foundational role in crisis management, a principle now universally adapted for civilian emergency departments and mass casualty incidents. While distinct approaches exist for MCIs (e.g., START, JumpSTART, SALT) versus daily ED operations (e.g., ESI, MTS), all systems rely on rapid assessment of physiological indicators (such as ABC/RPM) and skilled personnel. The effectiveness of triage hinges on core competencies like clinical judgment, adaptability, and the ability to manage complex information under pressure. However, it is consistently challenged by uncertainty, resource limitations, overcrowding, and the potential for bias, necessitating robust ethical frameworks to guide decision-making.
Reinforce Importance
Accurate and ethical triage is not merely a procedural step but an imperative for ensuring patient safety, optimizing resource allocation, and building overall healthcare system resilience. Its proper execution directly impacts patient outcomes, operational efficiency, and the public's trust in emergency medical services.
Recommendations for Future Enhancement
To further enhance the efficacy, equity, and resilience of emergency medical triage processes, the following recommendations are put forth:
Standardized and Advanced Training & Education: Implement comprehensive, consistent training programs across all levels of emergency responders and healthcare professionals. These programs should emphasize not only strict adherence to established algorithms but also the critical development of nuanced clinical judgment, adaptability, and the ability to interpret subtle physiological cues. Training should specifically address the unique needs of vulnerable populations, such as pediatric and elderly patients, to mitigate the risk of undertriage.
Continuous Quality Improvement and Audit: Establish robust, ongoing audit and feedback mechanisms for triage accuracy and consistency. This involves regular reviews of triage decisions and patient outcomes, using collected data to identify systemic weaknesses, refine protocols, and ensure continuous improvement in practice. Such a system fosters a culture of learning and accountability.
Strategic Technological Integration: Explore and integrate advanced technologies to support triage personnel. This includes the judicious use of artificial intelligence (AI)-powered tools, such as KATE AI (mentioned in the context of ENA's offerings) , which can assist triage nurses by improving acuity assignment for high-risk patients, optimizing patient flow, and enhancing critical reasoning for new practitioners. Technology should augment, not replace, human expertise.
Robust Ethical Framework Development and Review: Develop and regularly review clear, transparent ethical guidelines for triage decision-making, particularly addressing scenarios of resource scarcity and the potential for implicit biases. This process should involve broad stakeholder participation, including medical ethicists, clinicians, administrators, and patient advocates, to ensure comprehensive and equitable policies.
Enhanced Interprofessional Collaboration and Communication: Foster seamless communication and collaboration between pre-hospital (EMS) and in-hospital teams. This ensures consistent application of triage principles, smooth patient transitions, and continuity of care, which is vital for optimal outcomes, especially in complex or mass casualty scenarios.
Targeted Protocols for Vulnerable Populations: Develop and implement specific protocols and training modules dedicated to addressing the unique physiological and psychological needs of pediatric, elderly, and behavioral health patient populations. This proactive approach aims to counteract known tendencies for undertriage or mis-triage in these groups.
The mention of AI in the context of ENA's offerings and the pervasive challenges of uncertainty and resource limitations indicate that the future of emergency medical triage will involve a synergistic integration of human expertise with advanced technology. This highlights that the future of emergency medical triage lies in a synergistic integration of human expertise with advanced technology (e.g., AI for decision support). This collaboration, coupled with continuous training, robust ethical frameworks, and adaptable protocols, will be crucial for building healthcare systems that are not only efficient in daily operations but also resilient and equitable in the face of unpredictable mass casualty events and persistent resource constraints.
Final Statement
Ultimately, effective triage is far more than a mere medical procedure; it is a dynamic, ethically complex, and continuously evolving discipline. It stands as a fundamental cornerstone of public health preparedness and a profound testament to the unwavering commitment of healthcare professionals to saving lives and optimizing care in the face of adversity.
Additional Resources
For readers interested in exploring the topic of triage further, the following resources provide valuable information:
Emergency Nurses Association: Triage Education Resources Comprehensive training materials and certification programs for emergency triage.
World Health Organization: Emergency Triage Assessment and Treatment (ETAT) Guidelines for triage in resource-limited settings, with a focus on pediatric care.
Agency for Healthcare Research and Quality: Emergency Severity Index Implementation Handbook Detailed guidance on implementing the ESI triage system in emergency departments.
International Federation of Red Cross: Triage in Mass Casualty Situations Resources for managing triage in disaster and mass casualty scenarios.
TriageIQ Resources: AI in Healthcare Triage Information on the latest developments in AI-assisted triage technology.
