Clinician Burnout Reduction: How AI Triage Tools Are Changing Frontline Work
Explore how AI triage tools are revolutionizing frontline healthcare work by reducing clinician burnout. Discover the latest innovations and their impact on workload, cognitive burden, and patient care.


Clinician burnout has reached epidemic proportions within the healthcare sector, profoundly impacting the well-being of healthcare professionals, compromising patient safety, and threatening the sustainability of healthcare systems. This pervasive issue is largely driven by systemic factors such as overwhelming administrative burdens, intense time pressures, loss of autonomy, and chaotic work environments. Artificial intelligence (AI) triage tools are emerging as a pivotal solution, offering a transformative approach to mitigate these stressors.
This report details how AI triage tools, leveraging advanced machine learning and natural language processing, are reshaping frontline healthcare by automating routine tasks, providing robust decision support, and optimizing resource allocation. By alleviating administrative overhead and reducing cognitive load, AI empowers clinicians to refocus on direct patient care, thereby enhancing professional autonomy and job satisfaction. While significant benefits are evident in improved patient flow, access, outcomes, and operational efficiencies, challenges related to data quality, algorithmic bias, and the imperative of fostering clinician trust and patient acceptance remain. The optimal path forward lies in a collaborative human-AI model, where technology augments, rather than replaces, human expertise, paving the way for a more resilient, efficient, and compassionate healthcare future.
The Pervasive Challenge of Clinician Burnout
A. Defining Clinician Burnout: A Multifaceted Syndrome
Clinician burnout is a profound, long-term stress reaction manifesting as a classic triad of emotional exhaustion, depersonalization (feelings of cynicism or detachment), and a diminished sense of personal accomplishment. This syndrome represents a direct response to sustained job stressors within the demanding healthcare environment, characterized by packed workdays, intense pace, time pressures, and high emotional intensity. It is not merely stress but a deep loss of enthusiasm for work and a low sense of personal achievement.
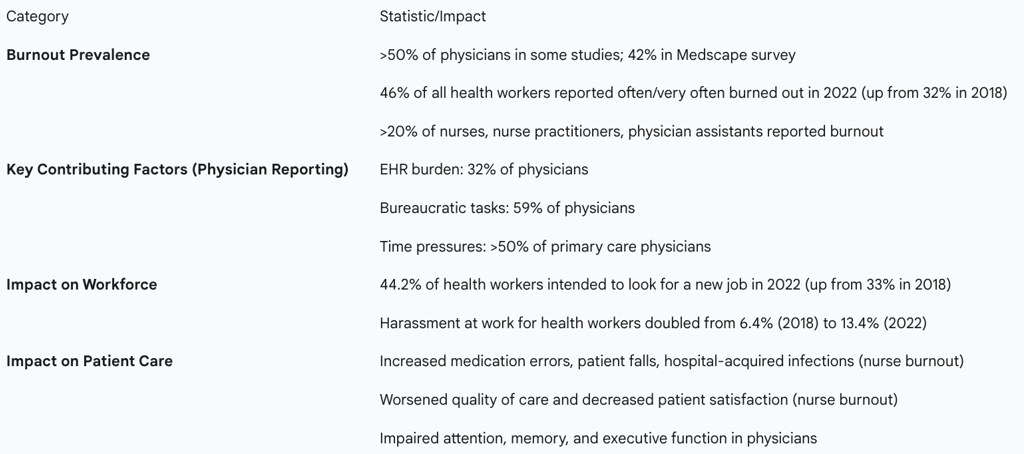
The prevalence of burnout among healthcare professionals has reached "epidemic proportions." Studies indicate that over 50% of physicians report experiencing burnout, with a recent Medscape survey finding 42% of physicians self-reporting symptoms. The situation has worsened significantly, with nearly half (46%) of all health workers reporting feeling burned out "often" or "very often" in 2022, a substantial increase from 32% in 2018. This rise is particularly pronounced in the percentage of health workers reporting burnout "very often," which increased from 11.6% to 19.0% during the same period. Nurses, nurse practitioners, and physician assistants also face high rates of burnout, with early findings showing over 20% affected, and rural clinicians reporting the highest rates. The COVID-19 pandemic is explicitly noted as having exacerbated this phenomenon.
The consistent description of burnout as a "long-term stress reaction" to "work conditions" and "problems with the U.S. medical system" underscores a crucial understanding: this widespread and increasing prevalence across diverse healthcare roles and over time indicates that the root causes are systemic and organizational, rather than isolated to individual clinicians. The observation that "it was the organization that burned doctors out that led to lower quality care, rather than the burned-out doctors themselves" further reinforces this organizational responsibility for the condition. Consequently, effective interventions must target the underlying structural and environmental flaws within the healthcare system that generate these stressors, rather than solely relying on individual coping mechanisms or "wellness" programs, which, while beneficial, do not address the fundamental drivers. This re-framing is essential for strategic decision-making in healthcare leadership.
B. Systemic Drivers of Burnout in Modern Healthcare
A significant portion of clinicians' time is consumed by extensive paperwork, detailed electronic health record (EHR) entries, and complex documentation requirements. EHR systems are a primary contributor to burnout, with 32% of surveyed physicians identifying it as the top factor. Federal and state laws impose duplicative and inconsistent documentation requirements, which are burdensome and time-consuming, draining both time and morale from physicians. Physicians spend nearly half (49%) of their time on EHRs and desk work, contrasting sharply with only 33% spent on direct patient interactions. This imbalance highlights how digital documentation demands interfere with patient care, with up to 70% of clinicians experiencing stress linked to health information technology, and EHR-related stress being an independent predictor of burnout.
Clinicians operate within demanding environments characterized by packed schedules and pressure to see a high volume of patients within limited timeframes. Over half of primary care physicians report stress due to time pressures, with nearly a third feeling they need at least 50% more time for physical examinations than allotted. Long working hours, including shifts up to 28 hours for residents who can work 80 hours a week, coupled with constant pressure and chronic fatigue, are major contributors to burnout. Staffing shortages further exacerbate chaotic work environments, increasing stress and fatigue.
Increasing administrative burdens and bureaucratic constraints frequently limit clinicians' autonomy in clinical decision-making, leading to frustration. Bureaucratic tasks were cited by 59% of physicians as a top burnout contributor. The necessity of managing multiple, frequently changing payment systems with complex rules, processes, metrics, and incentives, along with growing administrative requirements from laws and regulations, interferes with patient care and drains morale.
High patient volumes, staffing shortages, and limited resources create inherently chaotic work environments. Critically, a lack of trust in management, insufficient supervisor help, and a perception that the workplace does not support productivity are strongly associated with increased odds of burnout. Furthermore, reports of harassment at work among health workers more than doubled from 6.4% in 2018 to 13.4% in 2022. Early career clinicians, particularly general practitioners and nurses burdened with student loan debt (e.g., approximately $30,000 for nurses), often face significant financial pressure, which, when combined with long hours, can quickly lead to burnout.
The various research findings collectively demonstrate that the drivers of burnout are not isolated but form a complex, interconnected web. For instance, high patient volumes, a significant workload factor, directly contribute to time pressures, which in turn necessitates rapid and often burdensome EHR documentation, further increasing administrative load. This compounded pressure, coupled with a perceived loss of control or autonomy due to bureaucratic demands, creates a chaotic and unsupportive work environment. Data from the CDC explicitly quantifies how organizational factors like "enough time to complete work," "trusting management," and "supervisor help" significantly reduce burnout odds, illustrating the direct causal links between systemic support (or its absence) and clinician well-being. This intricate relationship suggests that a piecemeal approach to burnout reduction is unlikely to be effective. Instead, solutions must be holistic, addressing multiple, reinforcing stressors simultaneously. Technological interventions, such as AI triage, that alleviate one burden (e.g., administrative tasks) can create positive ripple effects across other areas (e.g., time pressure, cognitive load), thus offering a more comprehensive impact on clinician well-being.
C. Consequences for Clinicians, Patients, and Healthcare Systems
Burnout leads to significant dissatisfaction, chronic stress, and a strong intent to leave practice. The percentage of health workers "very likely" to seek a new job with another employer increased from 11.1% in 2018 to 16.5% in 2022, with 44.2% overall reporting an intention to look for a new job in 2022. Beyond professional dissatisfaction, burnout has severe health consequences for clinicians, acting as a significant predictor for heart disease, chronic pain, gastrointestinal distress, depression, and even mortality. Depressive disorders, a leading cause of disability, are associated with higher rates of absenteeism and presenteeism (working while physically ill) among health workers.
Burnout directly threatens patient safety and care quality. Depersonalization, a core component of burnout, can lead to poor interactions with patients, while impaired attention, memory, and executive function in burned-out physicians can compromise clinical judgment. Specifically, nurse burnout has been directly correlated with increased medication errors, patient falls, and hospital-acquired infections. It is also associated with a worsening quality of care and decreased patient satisfaction, as patients can readily sense a nurse's exhaustion, lack of meaningfulness in their work, or desire to quit.
The departure of burned-out doctors from practice reduces patients' access to and continuity of care, contributing to critical shortages, particularly in primary care physicians. System-wide, burnout results in increased absenteeism, higher staff turnover rates, and decreased job satisfaction, all of which negatively impact the overall functioning and sustainability of the healthcare system. The AMA emphasizes that addressing the systemic drivers of burnout is crucial for the health of medical practitioners and their practices.
The consequences of clinician burnout create a self-reinforcing negative feedback loop that actively degrades the healthcare system. Clinician attrition directly exacerbates staffing shortages, increasing the workload and pressure on remaining staff, thereby perpetuating and intensifying burnout. Simultaneously, the compromised quality of care and patient safety can lead to worse patient outcomes, potentially increasing demand on the system through complications or readmissions. The finding that "it was the organization that burned doctors out that led to lower quality care, rather than the burned-out doctors themselves" is a critical causal link, highlighting that organizational dysfunction is the root cause of both burnout and its detrimental effects on care quality. Therefore, investing in clinician burnout reduction is not merely a philanthropic endeavor or a staff welfare initiative; it is a fundamental strategic imperative for ensuring the long-term viability, safety, and quality of the entire healthcare system. It represents an investment in the foundational human capital that drives healthcare delivery.
Table 1: Key Statistics and Impacts of Clinician Burnout
AI Triage Tools: Capabilities and Current Landscape
A. What are AI Triage Tools? Core Concepts and Technologies
Triage is the critical process of rapidly assessing patients to determine the severity of their condition and prioritize their need for care, particularly vital in emergency rooms and other high-volume settings. AI triage tools are sophisticated software solutions that leverage advanced computational methods, including machine learning (ML) algorithms, natural language processing (NLP), and large language models (LLMs), to analyze vast amounts of patient health data. This data encompasses vital signs, medical history, reported symptoms, and even unstructured clinical notes.
Machine Learning (ML) models learn from extensive clinical datasets to identify intricate patterns and predict risks, continuously improving their accuracy as they process more cases. Natural Language Processing (NLP) enables AI systems to understand and extract relevant information from free-text patient narratives, physician notes, and patient descriptions, significantly streamlining documentation processes. Predictive analytics, a core component, allows AI algorithms to analyze historical and real-time patient data to forecast outcomes, predict the likelihood of patient deterioration, or identify the need for specific, timely interventions.
AI triage systems often combine two main approaches: Data-Driven AI, which learns from large clinical datasets to find patterns and predict risks, becoming more accurate with increased data exposure; and Model-Driven AI, which utilizes fixed rules based on established medical guidelines to ensure decisions adhere to standard care protocols. The synergy of these approaches allows AI triage systems to provide valuable data insights while maintaining adherence to healthcare regulations and best practices. These tools quickly process incoming information, suggest urgency levels, and identify potential serious conditions for prioritized attention. They can also forecast patient admissions, enabling administrators to proactively prepare resources such as staffing and equipment.
The detailed descriptions of AI triage tools reveal an evolution far beyond basic automation. The reliance on ML, NLP, and predictive analytics signifies that these tools are designed to learn, interpret complex, often unstructured data, and make probabilistic predictions. This indicates a fundamental shift from merely automating repetitive tasks to actively augmenting human cognitive processes in decision-making. The ability to "find patterns that may elude human clinicians" and "predict risks like heart attacks or infections" positions AI as a powerful cognitive assistant, not just a task manager. This fundamental transformation means AI triage is reshaping the nature of initial patient assessment from a purely human, often subjective, process to a data-driven, objective, and continuously improving system. This has profound implications for the speed, accuracy, and consistency of care delivery, especially in high-stakes environments.
B. Diverse Applications Across Healthcare Settings
AI plays a critical role in Emergency Departments (EDs) by rapidly sorting patients, which is especially vital during mass casualty events or peak hours, to identify those requiring immediate attention. These systems significantly reduce wait times, optimize resource allocation, and improve patient prioritization. Research indicates AI can outperform less experienced doctors in identifying urgent cases and reduce triage time. A UCSF-led study found an AI model was as effective as a physician at prioritizing ED patients (88% accuracy for AI vs. 86% for physician). Johns Hopkins researchers developed an AI tool that helps ED nurses confidently identify low-risk patients, leading to more efficient patient care pathways and improved patient flow.
In primary care, AI triage utilizes intelligent algorithms to assess patient symptoms and medical history, guiding them to the most appropriate care pathway. This automated initial assessment helps prioritize urgent cases, ensuring prompt attention, while directing less urgent cases to more suitable, often less resource-intensive, pathways. A study focusing on AI for respiratory symptoms in primary care demonstrated its precision in differentiating between low- and high-risk patients. AI also shows potential in managing specialist referrals more efficiently, potentially reducing unnecessary visits and alleviating the "gatekeeper" workload for primary care providers.
AI-powered virtual assistants and chatbots are increasingly common in outpatient clinics and care centers, offering 24/7 availability to answer patient questions, schedule appointments, assist with intake forms, and resolve billing inquiries. These tools can check symptoms, flag potential danger signs, and recommend appropriate actions, ranging from self-care to immediate clinic visits. Examples like Docus AI Symptom Checker and Ubie provide instant health insights and possible causes based on user input, empowering patients to better understand their symptoms.
Solutions such as Infermedica Intake and TMA's Patient Intake Assistant automate the collection and organization of essential health data prior to consultations. These systems efficiently gather demographic data, symptoms, risk factors, chronic disease history, medications, hospitalizations, and allergies. They integrate seamlessly with Electronic Health Records (EHRs) to pre-populate clinical notes and provide clinicians with lists of the most probable conditions, streamlining the pre-consultation process.
The broad array of applications, from initial symptom checking and appointment scheduling to pre-consultation data collection and critical care prioritization in EDs, demonstrates that AI triage is establishing itself as a comprehensive "digital front door" across the entire patient care continuum. This widespread integration allows for a more seamless and continuous patient journey, where early engagement and appropriate routing are facilitated from the very first interaction. The 24/7 availability further extends access beyond traditional operating hours, addressing a key patient need. This fundamental reshaping of how patients access and navigate healthcare services enables a more proactive and patient-centered model of care, where early intervention and efficient routing can prevent the escalation of conditions, reduce unnecessary healthcare utilization, and enhance the overall patient experience.
III. AI Triage as a Catalyst for Burnout Reduction
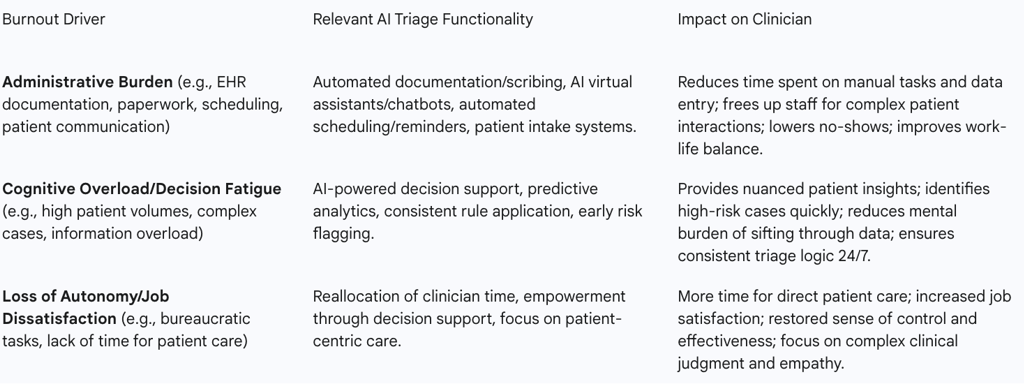
A. Alleviating Administrative Burden and Workload
AI significantly reduces the administrative burden by automating data entry, transcribing verbal notes into structured EHRs, and pre-populating forms. Natural language processing (NLP) tools, such as Nuance's Dragon Medical One, can transform doctor-patient conversations into comprehensive notes within EHRs, saving valuable time and minimizing errors. This capability holds substantial promise for reducing the extensive time healthcare professionals currently spend on manual documentation.
AI systems are adept at managing patient phone calls, answering routine questions, and automatically booking appointments, thereby significantly reducing patient wait times and freeing up reception and administrative staff. AI scheduling tools can notably lower no-show rates by up to 27% through intelligent appointment adjustments based on patient habits. A case study at The Groves Medical Centre demonstrated a 47% reduction in patient phone calls during busy periods after AI triage implementation.
By automating initial patient checks and bookings, AI tools directly lessen the workload on front-office staff. AI can automate up to 30% of routine patient interactions, including appointment scheduling and reminders, thereby reducing the overall administrative tasks for healthcare providers. This crucial shift allows nurses and doctors to reallocate their time and focus more on direct patient care, which is often the most satisfying aspect of their profession.
The pervasive administrative burden and relentless time pressures are consistently identified as primary drivers of clinician burnout. AI's capacity to automate these "low-value" yet time-consuming tasks directly addresses this core issue. By offloading activities such as documentation, scheduling, and routine patient communication, AI effectively "frees up valuable clinician time". This is not merely about increasing efficiency; it is about enabling clinicians to dedicate more time to the complex, human-centric aspects of patient care for which they were trained and which provide intrinsic professional satisfaction. This re-prioritization can alleviate the feeling of being "swamped with data" and enhance job satisfaction. Therefore, AI triage functions as a powerful force multiplier, allowing healthcare organizations to optimize their existing human capital. By reallocating clinician effort from administrative overhead to direct clinical engagement, AI directly combats a major systemic driver of burnout, contributing to a more sustainable and fulfilling work environment.
B. Mitigating Cognitive Overload and Decision Fatigue
AI-based decision support tools are instrumental in assisting nurses and doctors during the critical triage process. By analyzing intake form data and electronic health records (EHRs), AI platforms (e.g., KATE AI) generate objective urgency scores, such as the Emergency Severity Index (ESI). This provides clinicians with a more nuanced and comprehensive picture of a patient's condition, highlighting clinical subtleties or underlying chronic conditions that might otherwise be overlooked during initial manual assessments.
AI can be trained to flag potential serious conditions, such as sepsis, heart failure, or stroke, based on reported symptoms and medical history. This ensures that these high-risk patients are prioritized for immediate clinical attention. This capability significantly reduces the cognitive load on clinicians, who would otherwise have to manually identify such critical cases from a large volume of patient inquiries. Urgent alerts generated by AI can reach staff in less than 10 seconds, a substantial improvement compared to manual triage times of 3-5 minutes.
A key advantage of AI systems is their ability to apply consistent rules and algorithms to every patient interaction, 24/7, without experiencing fatigue or stress. This inherent consistency helps to minimize errors and variability in assessment that can arise from human factors such as exhaustion, subjective judgment, or workload pressures. By intelligently filtering out "low-value noise" and non-actionable alerts, AI can reduce the number of alerts clinicians need to review by approximately 30%. This directly addresses the problem of information overload, where doctors and nurses are often "swamped with data—labs, vitals, notes—all demanding review".
Clinicians routinely face immense pressure to make rapid, high-stakes decisions, often with incomplete information and in chaotic environments, leading to significant decision fatigue. AI triage directly mitigates this by automating the initial, data-intensive cognitive processing: it sifts through vast amounts of data, identifies critical patterns, and provides objective risk scores. This offloads the foundational cognitive burden, allowing clinicians to conserve their mental energy and focus their expertise on the truly complex cases that demand nuanced human judgment, critical thinking, and empathy. The "always-on consistency" of AI ensures that this decision support is reliable regardless of shift changes or individual fatigue levels, which is paramount in high-pressure settings like emergency departments. AI fundamentally shifts the cognitive burden in triage, enabling clinicians to operate at the "top of their license". This allows them to dedicate their finite cognitive resources to the "art" of medicine—complex diagnoses, ethical dilemmas, and personalized patient interaction—rather than the "mechanics" of initial data processing and risk assessment. The ultimate result is more accurate diagnoses, faster interventions, and improved patient outcomes, while simultaneously reducing a major, insidious source of clinician stress and burnout.
C. Enhancing Clinician Autonomy and Job Satisfaction
By automating repetitive and administrative tasks, AI enables healthcare workers to spend more quality time focused on direct patient care. This shift allows clinicians to engage more deeply with patients, which is a primary source of professional satisfaction and can help them "rediscover the Joy in Medicine®". The removal of a significant portion of repetitive administrative tasks directly translates to less stress and more dedicated time for patient diagnosis and treatment. Research indicates that when clinicians feel they have sufficient time to complete their work, trust management, and receive adequate supervisor support, their odds of experiencing burnout decrease significantly. AI's support in managing workloads contributes to creating a work environment where staff can more easily balance their professional responsibilities with their personal lives.
AI is positioned as a powerful decision-support tool that empowers clinicians, rather than seeking to replace their expertise. It provides data-driven insights and flags critical information, augmenting human decision-making and allowing clinicians to make more informed and confident choices. This restoration of a sense of control and effectiveness directly combats the "loss of personal accomplishment" and feelings of powerlessness that are central to burnout.
Clinician burnout is characterized by a "loss of enthusiasm for work" and a "low sense of personal accomplishment" , often stemming from systemic pressures that "erode and destroy intrinsic motivation". By significantly reducing administrative burdens and cognitive overload, AI allows clinicians to pivot back to the core, intrinsically rewarding aspects of their profession: direct patient interaction, complex problem-solving, and the profound impact of providing high-quality care. This "re-professionalization" of clinical work, by offloading the mundane and stressful tasks, can reignite passion, restore a sense of purpose, and directly counteract the depersonalization and reduced accomplishment associated with burnout. The AMA's objective to help doctors "rediscover the Joy in Medicine®" is a direct reflection of this potential. AI triage is not merely a technological fix for efficiency; it is a potential pathway to fundamentally restoring professional fulfillment and autonomy, which are critical for long-term clinician well-being, retention, and the overall attractiveness of healthcare careers. This has transformative implications for addressing the ongoing workforce crisis in healthcare.
Table 2: AI Triage Functionalities and Their Direct Impact on Burnout Drivers
Broader Benefits and Operational Efficiencies
A. Improving Patient Flow, Access, and Outcomes
AI triage significantly reduces unnecessary appointments and frees up valuable clinician time, leading to shorter waiting lists and quicker access to care for those who truly need it. At The Groves Medical Centre, patient waiting times for planned appointments dropped by a remarkable 73% (from a median of 11 days to 3 days) after AI implementation. In emergency departments, AI can substantially cut wait times by rapidly identifying critically ill patients who require immediate attention.
AI triage systems offer 24/7 accessibility from any location, making healthcare more convenient and accessible, particularly for individuals in rural areas or those with mobility challenges. The shift to digital engagement is evident, with online patient requests growing from 12% to 82% at one facility. Virtual triage tools empower patients to engage earlier in their care journey by providing immediate guidance on the appropriate acuity level of care to seek.
AI plays a crucial role in improving patient safety by identifying serious symptoms early and ensuring patients are directed to the correct level of care promptly. This capability reduces instances of unnecessary emergency care referrals and minimizes the risk of missing serious conditions. AI can identify high-risk patients who require immediate interventions, facilitating timely and potentially life-saving treatments. Studies also indicate that AI can improve diagnostic accuracy and reduce mis-triage rates.
The benefits of AI triage extend beyond merely supporting clinicians; they directly and positively impact the patient experience and clinical outcomes. Improved patient flow and reduced wait times are critical for time-sensitive conditions, leading to faster treatment and better prognoses. This, combined with AI's ability to enhance diagnostic support, reduce errors, and ensure consistent assessments, directly translates to improved patient safety and superior clinical outcomes. Furthermore, increased patient satisfaction and better outcomes can indirectly reduce the overall burden on the healthcare system by preventing complications and readmissions, thereby contributing to a less stressful environment for clinicians. AI triage represents a powerful "win-win" scenario. By leveraging technology to enhance operational efficiency and accuracy, healthcare systems can simultaneously elevate the quality, accessibility, and safety of patient care, creating a positive feedback loop that benefits both providers and patients.
B. Optimizing Resource Allocation and Operational Efficiency
AI significantly aids healthcare practices in managing their resources more effectively. By identifying the urgency and specific type of care required, AI allows for optimized allocation of staff (including GPs, nurses, and administrative personnel) and physical facilities. AI's predictive capabilities enable administrators to forecast patient volumes and needs, facilitating smarter planning for staff shifts, bed utilization, and equipment readiness, especially crucial during peak times or emergencies.
AI plays a vital role in minimizing instances of both over-triage (which wastes resources and exposes patients to unnecessary hospital environments) and under-triage (which delays urgent care and can worsen patient conditions). By using real-time data to predict patient risk, AI ensures that resources are directed precisely where they are most needed, allowing only the most severe patients to be treated first and thereby preventing overcrowding and prolonged wait times.
The implementation of AI has demonstrated tangible improvements in appointment management. At one medical center, 91% of appointments were automatically booked by AI, freeing up staff and allowing general practitioners (GPs) to extend their appointment times from 10 to 15 minutes. These longer, more thorough visits led to better initial care and a significant 70% reduction in patients requiring extra, follow-up visits.
Beyond the immediate benefits of workload reduction, AI triage offers profound strategic advantages in resource management. By providing predictive analytics on patient flow and demand patterns, AI enables healthcare administrators to transition from reactive crisis management to proactive, data-driven operational planning. This capability enhances the system's resilience, allowing it to effectively manage patient surges (e.g., during pandemics or flu seasons) without the need for additional staffing. This optimized resource utilization directly addresses the "chaotic work environments" and "staffing shortages" that are significant contributors to clinician burnout. AI triage transforms healthcare operations from a reactive, often strained model into a more agile, predictive, and resource-optimized system. This systemic efficiency, in turn, indirectly but powerfully supports clinician well-being by fostering a more orderly, predictable, and less stressful work environment, making the entire healthcare delivery system more sustainable.
C. Realizing Cost Savings within Healthcare Systems
Virtual triage systems are highly effective at reducing unnecessary emergency room visits, which are a significant financial drain on healthcare systems. For instance, Healthdirect Australia reported a 50% drop in emergency calls after implementing virtual triage, as patients were successfully redirected to less acute care settings. Clearstep's data further illustrates this, showing that virtual triage redirects approximately 45% of urgent ER visits to more appropriate care options, saving resources and costs while maintaining patient safety.
Automating routine tasks directly lowers operational costs and reduces the need for additional front-office or triage staff, especially during busy periods. A Juniper Research report highlighted substantial global annual cost savings from chatbot adoption in healthcare, reaching $3.6 billion by 2022. A U.S. healthcare system, Novant Health, reported a fourfold return on investment within just ten months of implementing AI virtual triage, achieving savings through reduced administrative work and fewer unnecessary urgent care visits. Studies indicate that approximately $175 can be saved per triage interview, and 57 nurse work hours can be saved for every 1,000 calls, translating into significant reductions in nurse overtime and overall labor costs for high-volume facilities.
AI's support in remote patient monitoring can lead to fewer preventable readmissions, thereby reducing associated costs. Furthermore, early detection and intervention facilitated by AI can improve patient outcomes and potentially avoid costly intensive care unit (ICU) admissions. AI's overall ability to reduce time in diagnosis and treatment contributes to cost savings.
Beyond the clinical and human benefits, the substantial financial advantages of AI triage provide a compelling business case for its widespread adoption. The direct cost savings from diverting unnecessary ER visits and automating administrative tasks are immediately impactful. Moreover, the indirect savings derived from improved patient outcomes (e.g., fewer complications, reduced readmissions) and optimized resource allocation contribute to the overall financial health and sustainability of healthcare organizations. This robust economic argument can significantly accelerate the adoption of AI solutions, as healthcare systems are continually seeking ways to enhance efficiency and reduce costs while simultaneously improving or maintaining the quality of care. AI triage is not merely a clinical enhancement; it is a strategic financial tool that can contribute significantly to the economic sustainability and operational resilience of healthcare organizations. This dual benefit of improving both care quality and financial performance makes AI an increasingly attractive and necessary investment for healthcare executives.
Challenges, Ethical Considerations, and the Imperative of Human-AI Collaboration
A. Data Quality, Integration Complexities, and Algorithmic Bias
The effectiveness of AI models is fundamentally dependent on the quality of the data they are trained on. A significant hurdle is the prevalence of missing, messy, or unorganized data within existing EHR systems, which can compromise AI predictions and potentially lead to erroneous medical decisions. Furthermore, achieving seamless integration of AI tools with diverse existing EHRs and complex IT infrastructures is a substantial technical challenge. Poor integration can impede workflow, counteracting AI's intended benefits.
A critical ethical concern is algorithmic bias. If AI models are trained on biased datasets (e.g., those that are non-representative of diverse populations or reflect historical healthcare inequities), their recommendations can inadvertently perpetuate or even amplify existing healthcare disparities. Research has shown that AI models can reproduce caregiver biases related to patient gender, for example, by underestimating the severity of conditions for women. This can lead to unequal treatment, misdiagnosis, or lower prioritization for marginalized groups. Continuous monitoring and rigorous ethical oversight are indispensable for identifying and mitigating these biases.
While vast amounts of data are the lifeblood of AI's predictive capabilities, they also represent its most significant vulnerability. Poor data quality directly translates to inaccurate predictions and potential patient harm. More profoundly, the historical biases embedded within existing healthcare data, if unaddressed during AI model training, can be amplified by AI, thereby exacerbating existing health inequities. The finding that AI can reproduce human biases underscores that simply automating current processes without critical re-evaluation and ethical intervention could worsen disparities. This necessitates a proactive, ethically driven approach to data collection, model development, and continuous monitoring. Successful and equitable AI implementation in healthcare demands substantial investment not only in the technological infrastructure but, more importantly, in robust data governance, sophisticated bias detection mechanisms, and an unwavering commitment to creating inclusive and representative datasets. Without this foundational ethical commitment, AI could inadvertently undermine the overarching goal of improving care for all populations.
B. Fostering Clinician Trust and Ensuring Patient Acceptance
Healthcare professionals must perceive AI as a supportive tool that augments, rather than replaces, clinical judgment. Barriers to trust include concerns about accuracy, safety, liability, and the "black box" nature of some AI decisions, where it is difficult to understand how the AI arrived at a particular recommendation. If emergency workers doubt AI's fairness or correctness, they might ignore its advice, negating its benefits.
Patient acceptance is equally crucial. Not all patients are comfortable with or have access to digital tools, requiring practices to ensure equitable access and support. Patients may worry about data privacy, device reliability, and the transparency of AI systems. Initial misconceptions about AI's capabilities, such as its ability to diagnose or prescribe without physician input, also need to be addressed through clear communication.
Clear communication about AI's role, functionalities, and limitations is vital for successful adoption by both clinicians and patients. Providing clear explanations for AI triage recommendations helps build clinician confidence. Comprehensive training programs that familiarize clinicians with AI processes and limitations are essential for smoother integration into workflows.
The successful integration of AI in healthcare hinges not just on its technical prowess but critically on the human element: trust. Both clinicians and patients harbor legitimate concerns about AI's accuracy, bias, and the implications for accountability and privacy. Without addressing these concerns through transparent explanations of AI's decision-making processes, robust educational initiatives, and continuous validation of its performance, AI tools risk underutilization or even rejection. The lack of trust can lead to over-reliance on traditional, less efficient methods, or, conversely, a dangerous blind trust in AI without critical human oversight. Therefore, building trust is not a secondary objective but a prerequisite for AI's transformative potential to be realized. Healthcare organizations must invest proactively in comprehensive change management strategies that prioritize education, transparent communication, and the active involvement of clinicians and patients in the AI implementation process. This collaborative approach is essential to foster confidence, ensure ethical deployment, and maximize the benefits of AI triage.
C. Regulatory and Ethical Frameworks for Responsible AI Deployment
AI systems rely on vast amounts of sensitive patient data, making privacy a paramount ethical concern. Regulations like HIPAA in the U.S. and GDPR in Europe aim to protect patient information, but challenges persist, including risks of unauthorized access, data misuse, and re-identification even from anonymized datasets. Robust cybersecurity measures, data anonymization, and encryption are crucial.
A significant question arises regarding who is responsible if an AI triage system makes an incorrect assessment that leads to a poor patient outcome. Clear rules are needed to determine accountability among clinicians, AI developers, and hospitals.
The regulatory landscape for AI in healthcare is still developing. Some countries regulate AI under Software as Medical Devices (SaMDs), while others use a risk-based approach. The World Health Organization (WHO) emphasizes the importance of establishing AI systems' safety and effectiveness, fostering dialogue among stakeholders, and developing robust legal and regulatory frameworks for safeguarding privacy, security, and integrity. Continuous monitoring and updates are needed to ensure AI tools remain effective and compliant over time.
The rapid advancement of AI technology often outpaces the development of comprehensive regulatory and ethical frameworks. The inherent complexities of AI, such as its "black box" nature and continuous learning capabilities, pose unique challenges for oversight, accountability, and long-term validation. The absence of clear guidelines creates legal ambiguities regarding liability and can hinder widespread adoption due to uncertainty and risk aversion among healthcare providers. Establishing robust, harmonized regulatory frameworks is not just about compliance; it is about building a foundation of trust and safety that will enable AI to reach its full potential responsibly. Proactive collaboration among policymakers, healthcare organizations, technology developers, and patient advocacy groups is essential to establish clear, adaptable, and internationally harmonized regulatory frameworks. These frameworks must balance innovation with patient safety, data privacy, and ethical considerations to ensure AI's responsible and equitable integration into healthcare.
D. Human-AI Collaboration: The Optimal Path Forward
The consensus among experts is that AI triage tools are most effective when viewed as powerful decision-support mechanisms that augment, rather than replace, human clinical judgment. AI excels at rapidly analyzing vast datasets and identifying patterns that humans might miss, providing objective risk assessments.
Human clinicians bring irreplaceable qualities to the triage process, including empathy, contextual understanding, the ability to interpret ambiguous information, and the capacity for nuanced judgment based on experience. They provide emotional support, build trust, and can adapt to unique patient circumstances that AI may overlook. The human element is crucial for validating or adjusting AI outputs based on clinical knowledge and ensuring patient safety.
The optimal approach involves a collaborative workflow where AI performs initial, data-intensive assessments, and human clinicians then take over for in-depth evaluations, personalized care, and final decision-making. This partnership allows clinicians to focus on complex cases requiring human expertise, while AI handles routine tasks and provides critical information. An "override" mechanism for clinicians to flag misrouted alerts and provide feedback for AI model refinement is crucial for continuous improvement.
The limitations of both purely human and purely AI-driven triage systems (e.g., human fatigue/bias versus AI's lack of context/empathy) necessitate a symbiotic relationship. The most effective and ethical future for healthcare triage lies in a model where AI acts as an intelligent co-pilot, enhancing human capabilities rather than displacing them. This collaborative model leverages AI's strengths in data processing and consistency while preserving the irreplaceable human attributes of empathy, contextual understanding, and ultimate accountability. This partnership is not just about efficiency; it is about elevating the overall quality and humanity of care. Healthcare organizations should prioritize the development and implementation of AI tools that are explicitly designed for human-AI collaboration. This includes intuitive interfaces, clear explanations of AI's reasoning, robust feedback mechanisms for continuous learning, and comprehensive training that empowers clinicians to effectively integrate AI into their practice, ultimately leading to superior patient outcomes and a more resilient healthcare workforce.
Conclusions
Clinician burnout is a systemic crisis in healthcare, driven by administrative overload, intense time pressures, and a perceived loss of autonomy. This widespread phenomenon severely impacts clinician well-being, compromises patient safety, and threatens the operational stability of healthcare systems. The evidence overwhelmingly demonstrates that addressing burnout is not merely a welfare concern but a strategic imperative for the long-term viability and quality of healthcare delivery.
AI triage tools offer a powerful and multifaceted solution to this crisis. By automating burdensome administrative tasks, providing consistent and objective decision support, and optimizing resource allocation, AI directly alleviates many of the primary stressors contributing to burnout. This reclaims valuable clinician time, reduces cognitive overload, and allows healthcare professionals to refocus on direct patient care—the core of their professional satisfaction. The adoption of AI triage has already demonstrated significant improvements in patient flow, reduced wait times, enhanced access to care, and improved clinical outcomes, while also generating substantial operational cost savings.
However, the transformative potential of AI is not without its complexities. Challenges related to data quality, the pervasive risk of algorithmic bias, and the critical need to foster clinician trust and patient acceptance must be proactively addressed. The regulatory landscape for AI in healthcare is still evolving, requiring continuous collaboration among stakeholders to ensure ethical and safe deployment.
The optimal future for healthcare triage is one where AI and human expertise work in a synergistic partnership. AI serves as an intelligent co-pilot, handling data-intensive tasks and providing objective insights, thereby augmenting human capabilities. This collaboration preserves the irreplaceable human elements of empathy, nuanced judgment, and ultimate accountability, leading to a more efficient, accurate, and humane healthcare system. By strategically investing in and thoughtfully implementing AI triage tools, healthcare organizations can not only mitigate the pervasive challenge of clinician burnout but also cultivate a more resilient, sustainable, and patient-centered future for frontline healthcare.
FAQ Section
Q: What are the primary causes of clinician burnout?
A: The primary causes of clinician burnout include long working hours, high-stress environments, limited personnel, and the burden of administrative tasks and clinical documentation in electronic health records (EHRs).
Q: How can AI triage tools streamline administrative tasks?
A: AI triage tools can streamline administrative tasks by automating data entry, documentation, and other administrative processes, allowing clinicians to focus more on patient care6.
Q: What are the benefits of AI-driven triage systems?
A: AI-driven triage systems can enhance patient prioritisation, reduce wait times, and optimise resource allocation by analysing real-time data such as vital signs, medical history, and presenting symptoms8.
Q: How does AI improve diagnostic accuracy?
AI tools can improve diagnostic accuracy by rapidly analysing patient data and medical literature, reducing the time spent on manual data entry and analysis, and alleviating the cognitive load on frontline workers6.
Q: What are the challenges in implementing AI triage tools?
A: Challenges in implementing AI triage tools include data quality issues, algorithmic bias, clinician trust, and ethical concerns8.
Q: How can data quality issues be addressed in AI triage tools?
A: Data quality issues can be addressed by ensuring AI algorithms are trained on diverse and representative datasets to avoid bias and ensure equitable implementation8.
Q: What are the ethical considerations in using AI in healthcare?
A: Ethical considerations in using AI in healthcare include developing ethical frameworks to address concerns surrounding the use of AI and ensuring clinician trust in AI-driven decisions8.
Q: How do AI triage tools impact patient care?
AI triage tools can improve patient care by reducing the administrative burden on clinicians, enhancing diagnostic accuracy, and optimising patient prioritisation in overcrowded emergency departments4.
Q: What is the role of AI in reducing clinician burnout?
A: AI can reduce clinician burnout by streamlining administrative tasks, enhancing patient triage, improving diagnostic accuracy, and addressing the underlying drivers of burnout, such as cognitive load and work burden4.
Q: How can healthcare organisations leverage AI to reduce burnout?
A: Healthcare organisations can leverage AI to reduce burnout by implementing AI triage tools, ensuring data quality, addressing ethical concerns, and fostering clinician trust in AI-driven decisions.
