Battlefield Healthcare: Lessons from Modern Conflicts in Triage, Evacuation, and Field Innovations
This report synthesizes critical lessons learned regarding triage under fire, evacuation logistics, and field innovations. It highlights the transformative evolution of Tactical Combat Casualty Care (TCCC) from a specialized skill to a universal competency, underscoring the imperative for data-driven adaptation in medical doctrine.


Recent military engagements, spanning from counter-insurgency operations in Iraq and Afghanistan to large-scale combat operations in Ukraine and complex peacekeeping missions, have profoundly reshaped the landscape of combat casualty care. This report synthesizes critical lessons learned regarding triage under fire, evacuation logistics, and field innovations. It highlights the transformative evolution of Tactical Combat Casualty Care (TCCC) from a specialized skill to a universal competency, underscoring the imperative for data-driven adaptation in medical doctrine. Persistent challenges in evacuation, particularly in contested environments, necessitate a shift towards prolonged casualty care at lower echelons and the adoption of creative, unconventional logistical solutions. Furthermore, a remarkable synergy between military and civilian medical advancements has driven innovations in hemorrhage control, telemedicine, and prosthetics. The report concludes with actionable recommendations for enhancing combat medical readiness, emphasizing continuous adaptation, comprehensive soldier care, and robust international collaboration to ensure optimal outcomes in the evolving global conflict environment.
The Evolving Landscape of Combat Trauma
Modern military conflicts, particularly those experienced since the turn of the millennium, have presented dynamic and often unpredictable operational environments, fundamentally altering the demands on combat medical systems. From the protracted counter-insurgency campaigns in Iraq and Afghanistan to the high-intensity, large-scale combat operations (LSCO) witnessed in Ukraine, and the complex humanitarian challenges in regions like Syria and the Sahel, the nature of warfare has directly impacted casualty patterns and medical response requirements. The lethality of modern weaponry has led to an increased frequency of severe injuries, including complex blast trauma, lumbopelvic dissociation, and multiple extremity amputations, posing significant challenges to traditional trauma care paradigms.
The human toll of these conflicts has been substantial. Between 2001 and 2021, approximately 1.9 to 3 million U.S. service members deployed to Iraq, Afghanistan, and associated theaters, with over half experiencing multiple deployments. This extensive exposure has contributed to higher rates of disability and a pronounced mental health crisis, including traumatic brain injury (TBI) and post-traumatic stress disorder (PTSD), compared to previous U.S. wars. The evolving nature of conflict, particularly the shift towards potential near-peer engagements, suggests that the traditional "golden hour" – the critical window for trauma patients to receive surgical intervention – may no longer be consistently achievable. Distances to higher levels of care are expected to be greater, and evacuation may rely on overland or water transport rather than rapid air assets, necessitating a fundamental rethinking of casualty care delivery. This represents a significant doctrinal adjustment, moving from an expectation of rapid evacuation to an imperative for prolonged care at lower echelons.
The insights gleaned from these diverse conflict zones are invaluable for shaping future military medical planning, training, and technological development. Military experience has historically been a wellspring for advancements in civilian trauma care, underscoring the reciprocal relationship between battlefield innovations and broader medical progress. A continuous cycle of performance improvement, driven by rigorous data analysis and the systematic reporting of casualty statistics and trends, is essential. This iterative process allows for the rapid advancement of diagnostics, therapeutics, and the refinement of tactics, techniques, and procedures (TTPs), ensuring that medical practices remain responsive to the realities of combat. The ability to adapt and integrate new knowledge quickly is paramount for maintaining medical readiness and ultimately, saving lives.
Triage Under Fire and Tactical Combat Casualty Care (TCCC)
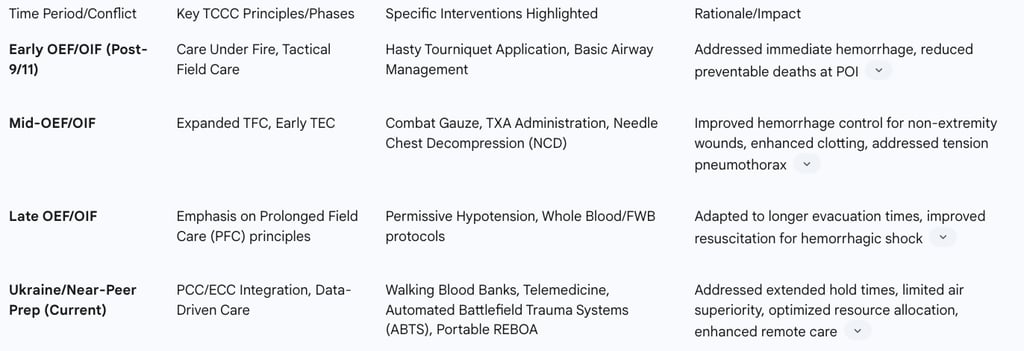
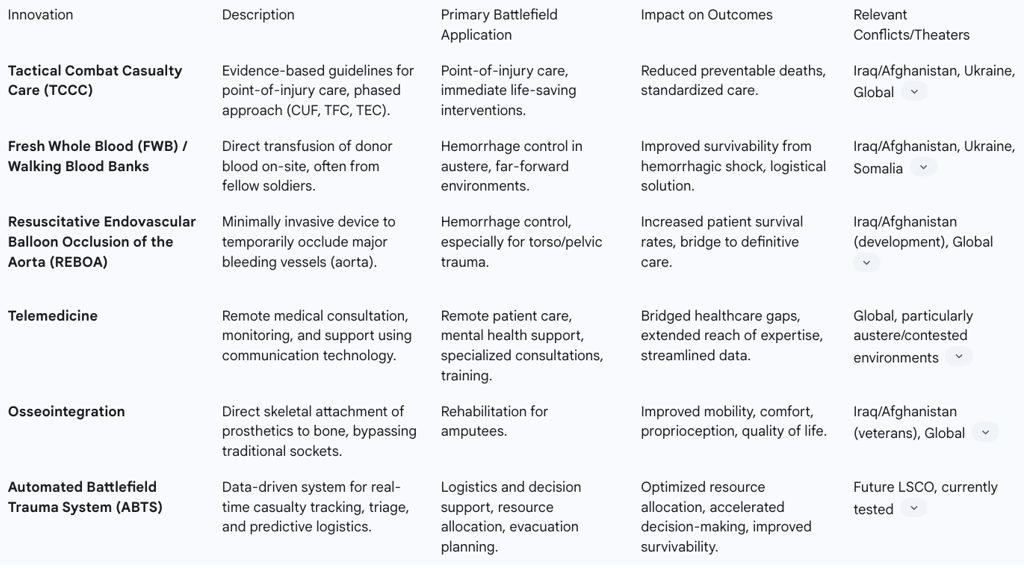
Tactical Combat Casualty Care (TCCC) represents a cornerstone of modern battlefield medicine, fundamentally transforming the approach to point-of-injury care. Developed in 1996 by special operations forces, TCCC guidelines are evidence-based and have been proven effective in reducing preventable deaths directly on the battlefield. Its widespread adoption is mandated for U.S. forces and NATO allies, reflecting a recognition that effective combat medicine must seamlessly integrate tactical considerations with medical interventions. The core philosophy of TCCC revolves around a phased approach: Care Under Fire (CUF), Tactical Field Care (TFC), and Tactical Evacuation Care (TEC). This structured methodology prioritizes interventions based on the immediate threat level, ensuring that the most critical, life-saving measures are performed first.
The emphasis on TCCC stems from a stark reality: nearly 90% of combat fatalities occur before a casualty can reach a medical treatment facility. This highlights the critical importance of immediate, effective care at the point of injury. TCCC employs mnemonic devices like MARCH (Massive hemorrhage, Airway, Respirations, Circulation, Head injury/Hypothermia) and PAWS (Pain, Antibiotics, Wounds, Splinting) to guide first responders through the proper sequence of interventions, ensuring that critical priorities like severe bleeding are addressed immediately.
Key Interventions and Their Impact on Survivability
Hemorrhage control remains the leading priority in TCCC, as uncontrolled bleeding is the primary cause of preventable death on the battlefield. Under fire, the hasty application of a Committee on Tactical Combat Casualty Care (CoTCCC)-approved tourniquet to life-threatening extremity hemorrhages is the recommended initial step, placed high and tight over clothing. Once behind cover, during Tactical Field Care, a more deliberate application of the tourniquet is performed, 2 to 3 inches above the wound, with the time of application clearly marked. Combat gauze is the hemostatic dressing of choice for non-extremity bleeding.
Beyond bleeding, TCCC addresses critical airway and breathing issues. This includes sealing open chest wounds with vented chest seals and decompressing suspected tension pneumothorax (PTX) using a needle chest decompression (NCD) procedure. For circulation and fluid resuscitation, controlling bleeding takes precedence over infusing fluids. Intravenous (IV) access is established only for individuals in shock or those requiring IV medications. Tranexamic acid (TXA), a medication that helps with clotting, is administered as soon as feasible to casualties at risk of hemorrhagic shock. This approach aligns with lessons from conflicts like Somalia, where selective fluid resuscitation, primarily for those in shock, was emphasized to conserve limited supplies and avoid hindering combatants who could continue fighting.
Training Paradigms for Medical and Non-Medical Personnel
A significant shift in military medical doctrine has been the evolution of combat medicine from a specialized skill set, primarily for medics, to a universal competency expected of all combatants. The 75th Ranger Regiment exemplifies this approach, having been a leading advocate for advancing TCCC. Their success is attributed to a command-owned casualty response system and a ubiquitous mastery of TCCC basics by all first responders, whether medical or non-medical personnel. This decentralization of immediate life-saving capability means that the initial responder to an injury is often a fellow combatant, not a dedicated medic. Evidence from mass casualty incidents shows the effectiveness of this approach, with over half of injured personnel in one event receiving self-aid and buddy care, which also serves as a form of auto-triage for minor injuries. This integration of medical training into core combat skills ensures that life-saving interventions can be initiated immediately, regardless of the presence of a trained medical professional.
Training programs now increasingly incorporate realistic scenarios, including the imposition of casualties at various points in mission rehearsals, to prepare personnel for the tactical implications of casualty management. Furthermore, the Medical Education and Training Campus (METC) has developed an "Introduction to Delayed Evacuation Care" component within its Combat Medic Specialist Training Program. This initiative aims to prepare medics for prolonged field care, a critical skill given the anticipated challenges of rapid evacuation in future near-peer conflicts.
The continuous refinement of TCCC guidelines demonstrates a highly adaptive and evidence-based medical system. Updates are not static but are driven by a constant flow of information from the battlefield, incorporating findings from Joint Trauma System performance improvement teleconferences, published case reports from war zones, breakthroughs in military medical research, and relevant civilian medical literature. This contrasts sharply with historical, slower doctrinal changes and highlights the critical role of real-time battlefield data in shaping medical practices. Maintaining robust data collection, analysis, and rapid dissemination mechanisms, such as the Joint Trauma System , is as vital as the medical interventions themselves, creating a feedback loop that allows for agile responses to new injury patterns and operational challenges, directly linking data to lives saved.
Table 1: Evolution of TCCC Guidelines and Key Interventions (2000-Present)
Evacuation Logistics: Challenges, Adaptations, and Prolonged Casualty Care
The efficacy of combat medical care is inextricably linked to robust and adaptable evacuation logistics. Modern conflicts, particularly those in contested and austere environments, have exposed significant vulnerabilities in traditional evacuation models, necessitating profound adaptations.
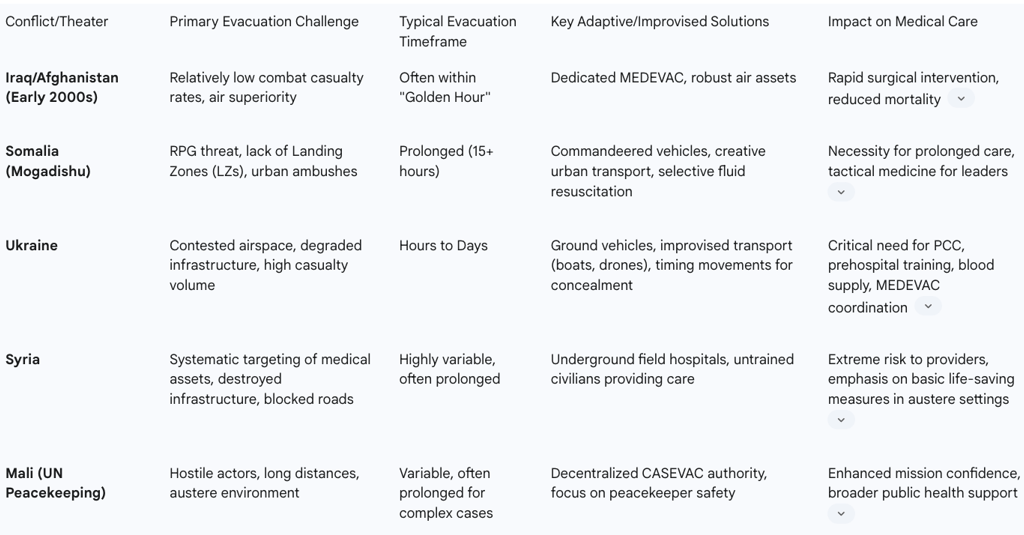
Challenges in Contested and Austere Environments
A recurring and critical challenge is the prevalence of prolonged evacuation times. The 15-hour delay experienced by casualties in Mogadishu, Somalia, starkly highlighted the inapplicability of civilian pre-hospital trauma management techniques, which typically assume hospital arrival within 15 minutes. More recently, in Ukraine, delays of hours to days are common due to contested airspace, which precludes aeromedical evacuation, and reliance on ground transport over degraded or destroyed roads. These conditions are often compounded by mass casualty incidents and adverse weather, further extending transport times.
Beyond environmental and tactical constraints, the deliberate targeting of medical assets has emerged as a grave concern in conflicts like Syria. Medical personnel and facilities have been systematically attacked, leading to a drastic reduction in available services and forcing the creation of improvised, often underground, field hospitals. This deliberate strategy of weaponizing healthcare infrastructure poses unique and severe challenges to the provision of care, moving beyond traditional rules of engagement and demanding innovative approaches to medical asset protection and clandestine care delivery. Such actions underscore the need for robust international legal frameworks to address these violations of medical neutrality.
Furthermore, lower echelons of care frequently face severe resource limitations, including shortages of medical equipment, supplies, and trained personnel. Small surgical teams deployed forward may lack the necessary critical care experience and equipment to provide prolonged post-operative care, creating a gap between immediate damage control procedures and definitive treatment.
Adaptive Strategies and Improvised Methods for Patient Movement
In response to these formidable challenges, military forces and humanitarian organizations have developed adaptive strategies and, at times, resorted to highly improvised methods for patient movement. Ground transportation remains the primary mode of evacuation in many contested environments, utilizing armored vehicles, ambulances, buses, minivans, and even trains. However, the most striking adaptations involve unconventional means. In Ukraine, battlefield constraints have led to the use of boats, quadricycles, and drones for evacuating casualties from the point of injury. Similarly, in urban environments where traditional transport is denied, commandeering civilian vehicles has proven to be a necessary, albeit improvised, solution. Tactical timing, such as conducting evacuation movements under the concealment of darkness, is also employed to mitigate risks.
A critical operational adjustment in resource-constrained, high-intensity environments has been the prioritization of transport over complete triage. When limited armored vehicles are available for evacuation, all patients who can fit are transported, even if initial assessment and triage are incomplete. This pragmatic decision is driven by the uncertainty of future vehicle availability and the imperative to move patients out of immediate danger. In peacekeeping contexts, such as the UN Multidimensional Integrated Stabilization Mission in Mali (MINUSMA), the high number of peacekeepers killed by hostile actors necessitated significant changes. MINUSMA decentralized the launch authority for casualty evacuation (CASEVAC) operations to speed up response times, recognizing that bureaucratic delays could cost lives.
The Imperative of Prolonged Casualty Care (PCC) and Expectant Casualty Care (ECC)
The realities of modern conflict dictate that military medics must be prepared to hold and treat patients for significantly longer periods than in the past, potentially for days, including those requiring surgical intervention. This shift elevates the importance of Prolonged Casualty Care (PCC) and, in extreme circumstances, Expectant Casualty Care (ECC). PCC training is now recognized as crucial, with a focus on "temporal fidelity" – extending the length of simulated encounters to mimic real-world delays. This approach helps providers navigate the profound effects of fatigue and resource limitations, while reinforcing the value of teamwork, communication, and meticulous documentation.
PCC fundamentally differs from typical medical care, as decision-making is often based on available resources rather than ideal clinical practice. There is a recognized gap in ECC training for Role 1 caregivers, which needs to be comprehensive and deliberate. Such training is vital not only for preparing providers for effective and ethical military medical decision-making in resource-scarce settings but also for addressing the profound psychological burden associated with death and dying on the battlefield, thereby building moral resilience within the medical corps. The need for prolonged care places significant psychological strain on providers, demanding that training addresses not just clinical competencies but also mental fortitude and ethical decision-making in high-stress, resource-constrained environments.
Table 2: Comparative Analysis of Evacuation Challenges and Solutions Across Modern Conflicts
Field Innovations in Combat Medicine
Modern conflicts have served as powerful catalysts for rapid innovation in military medicine, driving the development and adoption of technologies and practices that directly enhance survivability and long-term recovery. Many of these advancements have a bidirectional impact, benefiting both military and civilian trauma care.
Advancements in Blood Product Resuscitation
Hemorrhage remains the leading cause of preventable death on the battlefield, making effective blood product resuscitation a critical area of innovation. Fresh Whole Blood (FWB) transfusion has emerged as a vital solution, particularly in austere, far-forward environments where traditional blood banks are unavailable. Retrospective data from conflicts in Iraq and Afghanistan have shown a clear association between the use of FWB and improved survival rates. FWB offers several advantages: it requires minimal extra equipment to carry, contains increased clotting factor activity, is naturally warm (eliminating the need for fluid warmers), and provides fresh platelets, which are otherwise difficult to transport and use in forward settings.
The logistical challenges of providing blood in combat zones have led to the widespread adoption of "walking blood banks." This involves collecting fresh whole blood for direct transfusion from readily available donors on-site, a practice frequently noted in Ukraine due to the lack of standardized blood banking infrastructure. Predominantly, low titer group O whole blood (LTOWB) is used, as it can be transfused to any patient, making it a universal donor product. The ability to perform emergency fresh whole blood drives is now considered essential for medical facilities across all echelons of care, from Role 1 to Role 3.
Impact of Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA)
Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA) represents a significant advancement in hemorrhage control. This device is inserted into a major hemorrhaging vessel, typically the aorta, to temporarily stop or slow blood flow, particularly in the pelvic area and abdomen, without damaging vital organs. Developed by military researchers who identified a critical need for minimally invasive hemorrhage control on the battlefield, REBOA received FDA approval in 2015. Its application has dramatically increased patient survival rates, and it is now utilized in over 250 hospitals internationally, demonstrating a clear transfer of military innovation to civilian practice. Ongoing research continues to explore adaptations for prolonged use in austere settings, further extending its utility.
Role of Telemedicine in Remote and Austere Settings
Telemedicine has proven to be an invaluable tool for saving lives and extending medical reach in challenging conflict zones and disaster areas. It enables healthcare professionals to provide remote care, effectively bridging the gaps created by disruptions to traditional healthcare systems and the scarcity of medical personnel in war zones. Telemedicine applications are diverse, ranging from primary care and chronic condition management to mental health support, specialized consultations for complex cases, and even training and supporting local healthcare providers.
Technological advancements are streamlining telemedicine's battlefield application. New transport telemedicine systems are being developed to automatically document patient data and medication logs, thereby reducing the administrative burden on medics during evacuation missions and allowing them to focus more intently on patient care. This digital transformation addresses historical challenges where medics manually recorded patient information, often guessing weights for medication dosages, which slowed down treatment. While highly beneficial, challenges remain, including ensuring reliable communication in contested environments and tailoring solutions for vulnerable populations like refugees and internally displaced persons.
Innovations in Prosthetics and Rehabilitation (e.g., Osseointegration)
The long-term consequences of combat injuries, particularly limb loss, have driven significant innovations in prosthetics and rehabilitation since 9/11. These advancements aim to improve the quality of life and functional capabilities of warfighters. A notable breakthrough is the development of percutaneous osseointegrated prostheses (POP), or osseointegration (OI). This procedure involves the direct skeletal attachment of a prosthetic limb to the bone, offering a more stable and functional interface compared to traditional socket prostheses.
Benefits of osseointegration include improved mobility, enhanced comfort, a reduced risk of falls, and better proprioception, leading to a more natural and integrated experience for the patient. The OPRA™ Implant System, the first FDA-approved osseointegrated system, has shown promising clinical outcomes, with a 92% success rate at five years in one study. Despite these advancements, challenges persist, including the risk of infection at the transdermal implant site, limited access to multidisciplinary care, economic constraints, and the need for more long-term clinical evidence. Continued investment in regenerative medicine and advanced prosthetics remains crucial for the comprehensive care and rehabilitation of injured service members.
Data-Driven Systems for Casualty Management (e.g., Automated Battlefield Trauma System - ABTS)
The imperative for rapid, informed decision-making in large-scale combat operations has spurred the development of data-driven casualty management systems. The Automated Battlefield Trauma System (ABTS), pioneered by U.S. Army Col. Jay Baker, represents a significant digital transformation in battlefield medicine. This system is designed to enhance casualty care and logistics by collecting and estimating the number of wounded casualties by category, thereby informing predictive logistics and optimizing evacuation movements.
As a new component of the DoD's Joint Trauma System (JTS), which has already demonstrated a 44% decrease in deaths from battlefield trauma, ABTS aims to further refine care delivery. The system enables medics to quickly record patient data following the M.A.R.C.H. algorithm and automatically categorize casualties into triage groups, which then dictates the most appropriate evacuation facility based on their specific needs and available resources. By automating data collection and analysis, ABTS allows medical officers and non-commissioned officers to shift their focus from administrative tasks to direct patient care. This digital approach is critical for optimizing resource allocation, accelerating decision-making, and ultimately improving survivability and operational efficiency in future conflicts where casualty numbers are projected to be significantly higher. This represents a critical shift from manual, analog data collection to real-time, digital, and potentially AI-driven casualty management.
Table 3: Key Medical Innovations and Their Battlefield Application
Cross-Conflict Analysis: Case Studies and Unique Learnings
Analyzing medical lessons across various modern conflicts reveals both common challenges and unique adaptations, highlighting the dynamic nature of battlefield medicine.
Specific Lessons from Iraq and Afghanistan
The post-9/11 conflicts in Iraq and Afghanistan were pivotal in the development and widespread adoption of TCCC, contributing significantly to a reduction in preventable deaths. These conflicts saw the lowest combat mortality rates in military medical history, a success attributed in part to relatively low combat casualty rates, consistent air superiority that facilitated rapid evacuation, and high ratios of medical personnel to treated casualties. However, the prolonged nature of these deployments and repeated tours also led to a significant mental health crisis among service members, characterized by high rates of traumatic brain injury (TBI) and post-traumatic stress disorder (PTSD). A critical issue identified was the significant barriers to mental health care, largely due to the stigma associated with seeking such services. Furthermore, the experience in these theaters spurred the development of advanced prosthetics, such as osseointegration, which has dramatically improved the quality of life for amputees. The Joint Trauma System (JTS) was also created during this period to optimize care for the critically wounded, demonstrating a commitment to continuous performance improvement.
Insights from Ukraine
The ongoing conflict in Ukraine presents a different medical challenge, characterized by large-scale combat operations (LSCO) involving comparably armed military units and high-lethality weaponry. This environment generates a high volume of severely injured casualties that frequently overwhelm the capacity for effective and efficient combat casualty care. A key distinction from Iraq and Afghanistan is the absence of consistent air superiority, rendering aeromedical evacuation often impossible. This forces reliance on ground transport over poor and contested roads, resulting in prolonged evacuation times, often extending to hours or even days. This situation underscores the critical need for improved prehospital care training, the ability for safe patient movement without air superiority, robust prolonged casualty care (PCC) capabilities, a reliable blood supply, and enhanced MEDEVAC coordination. The reliance on "walking blood banks" for fresh whole blood has become a necessity due to these logistical constraints. The conflict also highlights an increased frequency of combat-blast exposure and high-acuity injuries compared to earlier conflicts. The medical environment in Ukraine demonstrates that adversaries can actively negate the advantages of air superiority and robust medical chains, creating asymmetric medical vulnerabilities that demand different approaches to care.
Lessons from Somalia (Battle of Mogadishu/Black Sea)
The Battle of Mogadishu (1993), often referred to as the Battle of the Black Sea, provided crucial early lessons that continue to resonate in modern combat medicine. It starkly emphasized the profound difference between civilian pre-hospital trauma management and the realities of a combat environment, particularly regarding prolonged evacuation delays, which in Mogadishu extended to 15 hours. This experience highlighted the critical need for tactical medicine instruction for small-unit leaders, as decisions regarding casualty management have significant tactical implications for the mission itself. The conflict reinforced the paramount importance of immediate hemorrhage control, particularly through the use of tourniquets, and demonstrated the necessity for creative, improvised evacuation methods when traditional options are denied due to intense hostile fire or blocked routes. Furthermore, lessons from Somalia informed the principle that fluid resuscitation should be selective, primarily for those in shock, to conserve limited supplies and avoid interfering with combatants who can continue fighting.
Challenges in Syria
The Syrian Civil War has presented a particularly grim scenario for combat medical care, characterized by the systematic targeting of medical personnel and facilities by government forces and their allies. This deliberate strategy has led to a devastating number of deaths among medical professionals and the decimation of healthcare infrastructure, forcing the creation of improvised "field hospitals" in hidden locations like basements. These clandestine facilities often operate without electricity, basic laboratory capabilities, or sufficient medical supplies. The conflict has seen untrained civilians stepping up to provide life-saving roles amidst the chaos. Patient transport is severely hampered by blocked roads and the constant threat of shelling. The situation in Syria serves as a stark example of the weaponization of healthcare as a tool of war, necessitating robust protection strategies for medical assets and the development of care delivery models in deliberately hostile and denied environments.
Medical Support and Evacuation in UN Peacekeeping Operations
UN peacekeeping missions, such as MINUSMA in Mali, face unique medical support and evacuation challenges, particularly due to the presence of hostile actors. Effective casualty evacuation systems are crucial for ensuring peacekeeper safety and maintaining mission confidence. In Mali, the decentralization of CASEVAC launch authority was implemented to speed up evacuations, recognizing the critical importance of rapid response for peacekeepers operating in high-risk environments.
Beyond direct combat trauma, UN peacekeeping operations in Africa, including the Central African Republic, Democratic Republic of Congo (DRC), and South Sudan, highlight a broader role for military medicine. These regions often grapple with universal healthcare challenges, inadequate infrastructure, shortages of trained healthcare professionals, and disruptions caused by political instability and conflict. In such contexts, UN peacekeepers, often from contributing nations like India and Bangladesh, frequently provide free medical care to displaced populations, effectively bridging critical gaps in local health services. This demonstrates that the military component in peacekeeping operations often undertakes peace-building activities beyond their explicit mandate, including providing essential medical support to local populations. This dual role suggests that military medical planning in stability or peacekeeping contexts must account for broader public health needs, infectious disease management, and humanitarian assistance, requiring different training and logistical considerations than purely combat-focused operations. The success of these medical interventions can also significantly contribute to stability and civil-military relations, indirectly supporting broader mission objectives.
Key Lessons Learned and Future Implications
The comprehensive review of recent conflicts reveals several overarching themes and critical takeaways that must inform future combat medical readiness.
Synthesis of Overarching Themes and Critical Takeaways
Adaptability is Paramount: Combat medicine must demonstrate extreme flexibility to respond to diverse and rapidly evolving conflict environments, ranging from asymmetric counter-insurgency to high-intensity, large-scale combat operations. The ability to pivot between different operational contexts and associated medical requirements is non-negotiable.
Decentralization of Care: The widespread adoption of TCCC for all combatants and the increasing necessity for prolonged casualty care at lower echelons signify a fundamental shift towards distributed medical capabilities. Immediate life-saving interventions are no longer solely the purview of dedicated medical personnel but a universal competency.
Data-Driven Improvement: The continuous collection, rigorous analysis, and rapid integration of battlefield medical data are indispensable for agile doctrinal and technological adaptation. This feedback loop ensures that medical practices are constantly refined based on real-world outcomes.
Logistical Resilience: Future conflicts will demand highly resilient and adaptable evacuation logistics. This includes the critical ability to operate effectively without air superiority and to leverage improvised transport methods when traditional logistical chains are disrupted or denied.
Holistic Soldier Care: Beyond immediate trauma management, comprehensive soldier care must encompass mental health support and long-term rehabilitation. The prevalence of PTSD and TBI from recent conflicts highlights the critical importance of addressing the invisible wounds of war and providing advanced rehabilitative solutions like osseointegration for force preservation and veteran well-being.
Protection of Medical Neutrality: The deliberate targeting of medical assets in conflicts like Syria underscores a concerning erosion of international humanitarian law. This necessitates robust protection strategies for medical personnel and facilities, alongside sustained international advocacy to uphold medical neutrality in armed conflict.
Anticipating Medical Challenges in Future Large-Scale Combat Operations
Looking forward, military medical systems must prepare for a new set of challenges inherent in potential large-scale combat operations:
Higher Casualty Volumes and Severity: The nature of near-peer conflict, with high-lethality weaponry, is expected to result in a significantly increased volume and severity of injuries, potentially overwhelming existing medical capacities.
Extended Evacuation Times and Limited Access to Definitive Care: Contested environments will likely restrict rapid aeromedical evacuation, leading to prolonged patient hold times at lower echelons and delayed access to surgical facilities.
Increased Demand for Prolonged Casualty Care (PCC) and Expectant Care (ECC): Medics will be required to manage critically injured patients for extended periods, demanding advanced skills in critical care and resource conservation.
Logistical Strain on Blood Products and Medical Supplies: Maintaining a consistent supply of blood products and essential medical equipment will be a major logistical hurdle in dispersed and contested battlefields.
Cyber and Information Warfare Impacts: Telemedicine and data-driven systems, while innovative, will be vulnerable to cyberattacks and information warfare, necessitating robust cybersecurity measures and resilient communication networks.
Recommendations for Enhancing Combat Medical Readiness
Based on the comprehensive analysis of lessons learned from recent conflicts, the following recommendations are put forth to enhance combat medical readiness for the evolving global security landscape:
Policy and Doctrine Adjustments
Revise "Golden Hour" Doctrine: Military medical doctrine must formally acknowledge and adapt to the realities of large-scale combat operations where the "golden hour" for surgical intervention may not be consistently achievable. This requires a doctrinal shift towards enabling prolonged casualty care at lower echelons as a standard operational capability.
Formalize PCC and ECC Guidelines: Comprehensive guidelines for Prolonged Casualty Care (PCC) and Expectant Casualty Care (ECC) should be formalized and integrated into standard military medical doctrine. This includes clear decision-making frameworks for resource-limited environments and ethical considerations.
Streamline Innovation Adoption: Policies should be developed to accelerate the adoption and widespread dissemination of battlefield-proven innovations, ensuring that lessons learned translate rapidly into updated TTPs and equipment procurement.
Strengthen Medical Neutrality Protections: Advocate for and reinforce adherence to international humanitarian law regarding the protection of medical personnel and facilities. Develop robust strategies for safeguarding medical assets and personnel in environments where medical neutrality may be deliberately violated.
Training and Education Enhancements
Expand Universal TCCC Training: Continue to expand and deepen TCCC training for all combatants, not just medical personnel, with increased emphasis on advanced life-saving skills for non-medical first responders. This fosters a distributed medical capability at the point of injury.
Incorporate Temporal Fidelity and Ethical Dilemmas: PCC and ECC training simulations should incorporate temporal fidelity (extended scenarios) and present realistic ethical dilemmas to prepare providers for the physical and psychological demands of prolonged care in resource-constrained settings.
Integrate Tactical Medicine into Leadership Training: Mandate tactical medicine instruction for small-unit leaders to ensure they understand the tactical implications of casualty management and can integrate medical considerations into mission planning effectively.
Address Mental Health Stigma: Implement comprehensive mental health literacy programs and anti-stigma campaigns across all service branches to encourage early help-seeking and ensure accessible, confidential mental health support for service members and veterans.
Cross-Train for Stability Operations: Military medical personnel should receive cross-training in public health, infectious disease management, and humanitarian assistance to effectively support both combat trauma and broader public health needs in stability and peacekeeping operations.
Technological Development and Procurement Priorities
Invest in Ruggedized Medical Devices: Prioritize the development and procurement of portable, ruggedized medical devices and equipment suitable for prolonged care at lower echelons, capable of functioning in austere and contested environments.
Advance Hemorrhage Control Solutions: Continue robust research and development into advanced hemorrhage control technologies, including prolonged use applications for REBOA and novel hemostatic agents.
Accelerate Digital Medical Systems: Expedite the development and deployment of secure, resilient telemedicine and data management systems, such as the Automated Battlefield Trauma System (ABTS), to optimize casualty tracking, predictive logistics, and resource allocation.
Ensure Robust Blood Supply Chains: Invest in resilient supply chains for blood products, including the capability for widespread use of Low Titer Group O Whole Blood (LTOWB) and the establishment of "walking blood bank" protocols in austere environments.
Sustain Rehabilitation Innovations: Maintain sustained investment in advanced prosthetics, regenerative medicine, and comprehensive rehabilitation programs to ensure optimal long-term recovery and quality of life for injured service members.
Interoperability and Collaboration
Foster Civilian-Military Synergy: Strengthen collaboration and knowledge transfer between military and civilian trauma systems through joint research initiatives, shared training platforms, and personnel exchanges to maximize innovation and improve overall trauma care capabilities.
Enhance Allied Interoperability: Improve interoperability among allied forces in medical planning, standards, equipment, and communication protocols to ensure seamless medical support in multinational operations.
Strengthen Partnerships with International Organizations: Reinforce partnerships with international organizations, such as the United Nations (UN) and the World Health Organization (WHO), to enhance medical support capabilities in complex humanitarian and peacekeeping operations, addressing broader public health challenges in conflict-affected regions.
Conclusion
The conflicts of the 21st century have profoundly impacted military medicine, driving an evolution from established doctrines to highly adaptive and innovative approaches. The experience in Iraq and Afghanistan, while showcasing remarkable advancements in rapid trauma care, also highlighted the long-term human costs, particularly in mental health. Subsequent conflicts, notably in Ukraine and Syria, have underscored the limitations of traditional medical support in contested and denied environments, necessitating a fundamental shift towards prolonged casualty care at the lowest echelons and the adoption of creative, unconventional logistical solutions.
The transformative power of Tactical Combat Casualty Care (TCCC), the emergence of advanced hemorrhage control techniques like Fresh Whole Blood and REBOA, the expanding role of telemedicine, and innovations in rehabilitation such as osseointegration, all demonstrate a dynamic and responsive medical community. Critically, the increasing reliance on data-driven systems, exemplified by the Automated Battlefield Trauma System, signals a future where medical decision-making and resource allocation are optimized through digital integration.
These lessons provide an invaluable roadmap for enhancing combat medical readiness. The imperative for continuous adaptation, comprehensive soldier care extending beyond physical injury, and robust collaboration across military, civilian, and international sectors is clear. By integrating these critical learnings into policy, training, technology, and partnerships, military medical systems can better prepare to mitigate casualties, preserve fighting strength, and ensure optimal outcomes for service members in the evolving and unpredictable landscape of global conflict.
