Assessing the German Version of the Manchester Triage System
The German Version of the Manchester Triage System (GMTS) represents a critical adaptation of an internationally recognized patient prioritization tool for emergency departments (EDs) across German-speaking Europe.


The German Version of the Manchester Triage System (GMTS) represents a critical adaptation of an internationally recognized patient prioritization tool for emergency departments (EDs) across German-speaking Europe. Developed from the original Manchester Triage System (MTS), GMTS aims to standardize initial patient assessment, enhance patient flow, and improve safety outcomes in high-pressure clinical environments. This report evaluates the GMTS by examining its core principles, specific adaptations for the German context, its validated performance in terms of reliability and validity, the benefits it confers, and the inherent challenges and criticisms associated with its implementation.
Analysis indicates that GMTS effectively identifies patients requiring critical care, demonstrating strong predictive power for Intensive Care Unit (ICU) admission and a clear association with mortality. Its inter-rater reliability, as shown in initial studies, is exceptionally high, underscoring its consistency in patient categorization. The widespread adoption of GMTS in over 150 German hospitals reflects a proactive response to increasing patient volumes and resource limitations, aligning German emergency care with global best practices.
However, the report also highlights important considerations. The specific adaptations in GMTS, including variations in flowcharts and time allowances, necessitate independent validation and careful consideration for cross-national comparability. Performance nuances exist, particularly concerning its predictive power for general hospital admission and longer-term mortality, and its application in vulnerable patient populations like children and the elderly, where misclassification rates can be higher. Furthermore, the effectiveness of GMTS is significantly influenced by operational factors such as time constraints, resource limitations, and the human element of clinical decision-making by nurses.
Recommendations include developing targeted training for specific patient demographics, investing in systemic support for emergency nurses, and conducting continuous, large-scale, multi-center research to further validate and optimize GMTS across diverse German clinical settings. Policy considerations should focus on standardizing adaptations and encouraging comparative studies with alternative validated systems like the Emergency Severity Index (ESI) to ensure the most effective triage solutions are deployed throughout Germany's evolving healthcare landscape.
1. Introduction to Triage and the Manchester Triage System (MTS)
1.1. The Critical Role of Triage in Emergency Healthcare
In the dynamic and often resource-constrained environment of emergency departments (EDs), effective patient prioritization is paramount. The Manchester Triage System (MTS) emerged as a globally recognized tool designed to quickly assess patient urgency and allocate resources efficiently. It serves as a structured approach to ensure that the most critical cases receive immediate attention, while others are managed in a systematic order. This standardized initial assessment, or triage, is a fundamental prerequisite for initiating urgent medical treatment, especially when resources are limited. The core objective of MTS is to minimize variability in triage decisions, ensuring that patients with similar conditions are assessed and prioritized uniformly, regardless of the individual conducting the assessment.
The fundamental value of MTS extends beyond mere operational efficiency to encompass principles of equity and patient safety. By standardizing the assessment process, MTS aims to reduce human error and minimize the impact of individual bias in high-pressure settings. The system's design promotes fairness in access to care, ensuring that patients with comparable clinical needs receive consistent prioritization. This consistent application of clinical guidelines fosters a more reliable healthcare experience and builds public trust. Furthermore, MTS functions as a vital clinical risk management tool that enhances the resilience of emergency healthcare systems, particularly when clinical demand exceeds capacity. Its structured approach allows for safe patient flow management even under immense pressure, preventing system overload and ensuring critical care remains accessible. This positions MTS not merely as a day-to-day operational tool but as a critical infrastructure component that enables EDs to maintain functionality and patient safety during peak demand, mass casualty incidents, or other crises, acting as a buffer against potential system collapse by systematically allocating scarce resources.
1.2. Core Principles and Methodology of the International Manchester Triage System
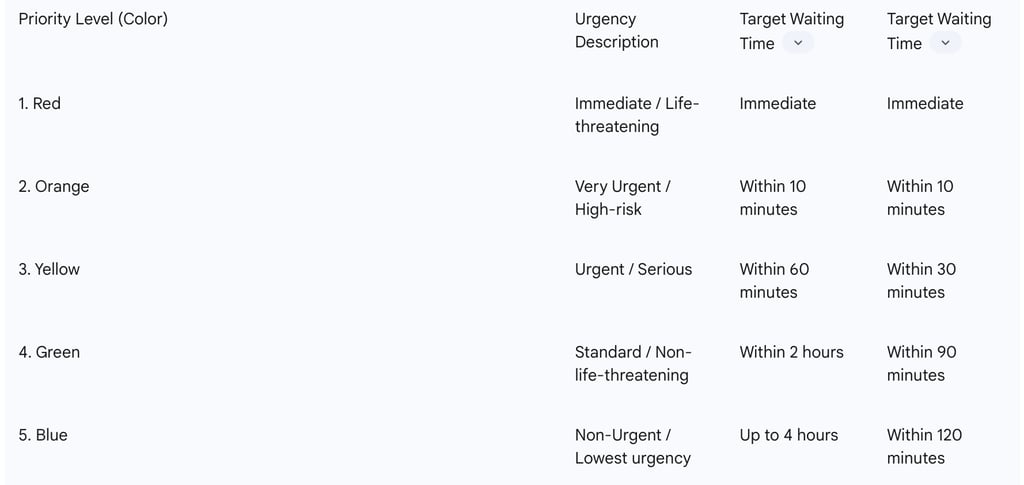
Developed in Manchester, England, during the 1990s, the MTS is a five-tiered clinical tool that categorizes patients based on their observed symptoms and condition. These categories are assigned a color code and a target waiting time for initial medical attention:
Red (Immediate): For life-threatening conditions, requiring immediate intervention.
Orange (Very Urgent): For high-risk conditions, requiring treatment within 10 minutes.
Yellow (Urgent): For serious but not immediately life-threatening conditions. Target waiting time is reported as within 60 minutes or 30 minutes.
Green (Standard): For less urgent conditions. Target waiting time is reported as within 2 hours or 90 minutes.
Blue (Non-Urgent): For conditions that can safely wait. Target waiting time is reported as up to 4 hours or 120 minutes.
The system employs "decision points" or "discriminators"—key symptoms or signs—to guide the triage nurse in assigning the appropriate category. Crucially, MTS is presentation-based, meaning it focuses on what the patient says is happening rather than attempting to diagnose the underlying cause. This approach allows for rapid, consistent assessment. It is also described as a "reductive system".
A notable aspect of the MTS is the observed variability in reported target waiting times across different sources, as illustrated in Table 1. For instance, the target waiting time for "Yellow" category patients is cited as both 60 minutes and 30 minutes , with similar discrepancies for "Green" and "Blue" categories. This variation suggests that while the five-tiered color-coded system is universal, the precise target waiting times may be subject to regional adaptation or evolution of the system over time. Such differences, if not clearly understood and accounted for, could lead to disparate performance benchmarks and patient expectations, complicating cross-institutional or international comparisons of efficiency or patient outcomes. The principle of MTS being "presentation, not diagnosis based" further underscores its primary function as a clinical risk management tool for patient flow and prioritization, rather than a diagnostic instrument. This deliberate design choice enables rapid assessment by non-physician staff, allowing trained nurses to quickly categorize patients without needing to perform a full diagnostic workup. This efficiency is vital for managing patient flow and identifying immediate risks , but it also defines the boundaries of its clinical utility at the initial triage stage, emphasizing its role in urgency assessment over definitive diagnosis.
Table 1: Manchester Triage System (MTS) Five Priority Levels and Target Waiting Times
1.3. Global Adoption and Continuous Evolution of MTS
The Manchester Triage System has achieved widespread international recognition and adoption, particularly across Europe, establishing itself as an "International Gold standard for Emergency Triage". Its success is attributed to its clear structure and focus on clinical decision-making. The system is not static; it undergoes regular reviews and updates to integrate the latest clinical evidence and best practices. Maintaining MTS Accreditation requires adherence to key governance elements, including software design, licensing, audit processes, and the timely implementation of these updates. Critically, using outdated versions of the system can lead to compromised patient outcomes, especially concerning conditions like adult and pediatric sepsis, due to outdated treatment and priority parameters. Beyond emergency departments, MTS has evolved into an integrated suite of tools, including applications for telephone triage, paramedic services (Pathfinder), nursing and residential homes (NaRT), and community-based healthcare professionals (SAFE pathways), indicating a broader application of its principles across the healthcare continuum.
The requirement for MTS Accreditation and the explicit warning against using outdated versions reveal a direct and critical link between system governance (updates, audits) and patient safety. The system's developers emphasize that MTS is not static, undergoing regular reviews and updates to incorporate the latest clinical evidence and best practices. Failure to implement these timely updates, particularly for evolving clinical guidelines (e.g., in sepsis management), can lead to mis-triage and directly compromise patient outcomes. This transforms system maintenance from an administrative task into a fundamental patient safety imperative, highlighting that neglecting governance can have severe clinical consequences. Furthermore, the expansion of MTS into various domains beyond the traditional ED, such as telephone triage, pre-hospital care, nursing homes, and community settings , signifies a broader strategic shift towards integrated, standardized urgency assessment across the entire patient journey. This evolution suggests that the principles of MTS are recognized as foundational for managing patient flow and risk throughout a connected healthcare network, not solely at the hospital front door. This implies a strategic move towards a more holistic and integrated healthcare system where standardized risk assessment and patient flow management are applied consistently from the first patient interaction, aiming to optimize care pathways and resource utilization across the entire network.
2. The German Version of the Manchester Triage System (GMTS): Development and Implementation
2.1. Historical Context and Introduction of GMTS in Germany
The German Version of the Manchester Triage System (GMTS) has seen widespread adoption in Emergency Departments across German-speaking Europe. While the original MTS was developed in Manchester, UK, between 1994 and 1995 , the German translation of its second edition became available in book form in 2006. A significant milestone was reached on April 1, 2008, when Charité - Universitätsmedizin Berlin became the first German university hospital to establish MTS across all its emergency department sites. Since then, GMTS has rapidly integrated into the German healthcare landscape, with over 150 German hospitals implementing it, establishing it as a standard system in their emergency rooms. This widespread implementation reflects a clear recognition within Germany of the need for standardized patient assessment to manage unpredictable patient volumes and limited resources effectively.
The swift and broad implementation of GMTS across more than 150 German hospitals within a few years of its translation (2006/2008 onwards) indicates a strong perceived need and readiness within the German healthcare system for a structured triage solution. This rapid uptake suggests that German EDs were actively seeking methods to improve patient flow and prioritization, likely driven by increasing patient numbers and the challenges of crowding. The speed of adoption highlights a proactive response to these systemic pressures. This successful widespread implementation also points to a notable level of organizational readiness and a willingness to adopt international best practices in German emergency medicine. Implementing a system like MTS requires significant training and operational changes. The fact that numerous hospitals embraced it implies that the German healthcare system, despite its inherent complexities, was receptive to a standardized, internationally recognized tool, demonstrating a pragmatic approach to enhancing emergency care standards.
2.2. Specific Adaptations and Key Differences from the Original MTS
The German version of the Manchester Triage System is not a direct, word-for-word translation of the original English version. Significant adaptations have been made to align with the German healthcare context and linguistic nuances. These differences notably include variations in "presentation diagrams and change indicators," which can have a substantial impact on the assigned triage category. Furthermore, new indicators and modified time allowances were introduced specifically for the Green and Blue (lower urgency) categories in the GMTS. Some concepts, such as "hot adult" and "young pain," which are present in the original MTS, are reportedly "unaccustomed" in the German context and may lead to errors in application. Charité - Universitätsmedizin Berlin, for instance, employs an "extended MTS" that incorporates additional objective clinical data. Beyond patient symptoms, this extended version includes the assessment of vital functions (respiration, circulation, consciousness) and vital parameters (pulse, blood pressure, respiratory rate, oxygen saturation, and level of consciousness), and in certain cases, body temperature. It also includes specific inquiries about symptoms indicative of a heart attack or stroke for early recognition.
The explicit differences in "presentation diagrams and change indicators," "new indicators and time allowances," and "translation nuances" mean that GMTS is a distinct variant, not a mere translation. This is a crucial distinction because if the core algorithms or thresholds for categorization are altered, then direct comparisons of performance metrics (e.g., validity, reliability, patient outcomes) between GMTS and other international MTS implementations become potentially misleading without careful consideration of these specific adaptations. This also raises questions about the fidelity of the German version to the original evidence base, necessitating independent validation studies for GMTS. The mention of "unaccustomed" concepts further highlights potential challenges in consistent application due to cultural or clinical differences. Charité's "extended MTS" exemplifies a local adaptation that adds objective vital sign data to the triage process. While incorporating vital parameters like blood pressure and oxygen saturation can undoubtedly enhance the accuracy of identifying critically ill patients (e.g., for sepsis, stroke, or heart attack), it also adds steps to the triage process. This could potentially increase the complexity and time required for initial assessment, creating a dynamic tension with the MTS's core principle of rapid, presentation-based triage. This adaptation highlights a trade-off between comprehensive clinical assessment and the need for speed in emergency triage, and it also implies a need for even more extensive training for triage nurses and could impact the overall efficiency of the ED intake process.
2.3. Implementation Strategies and Training Requirements in German Emergency Departments
The successful implementation of GMTS in Germany has relied on structured training programs and ongoing quality assurance. Upon its introduction, all care employees received a comprehensive 2.5-day in-house schooling on the Manchester Triage System, with new employees undergoing a several-day-long program before working in the ED. The Manchester Triage Group (MTG) explicitly states that MTS was developed solely for registered Healthcare Professionals (HCPs) (equivalent to UK Band 5 or higher internationally), emphasizing that the clinical skills and knowledge required for accurate triage assessment are substantial. MTG will not support organizations that allow non-HCPs to use the system, underscoring the professional nature of the triage role. To ensure correct implementation and consistency within Hospital Information Systems (HIS), an "Excel map" is provided to licensed software companies, which is regularly updated after international conferences. Manual entry from printed books is discouraged due to the risk of errors. Furthermore, quality improvement of triage is mandated through regular audits, with specific guidelines on sample size (2% of cases, minimum 10 episodes per user) and frequency (at least quarterly), ensuring continuous monitoring and adherence to standards.
The extensive training requirements and the strict mandate for registered Healthcare Professionals (HCPs) to perform triage highlight a clear recognition that effective triage is a complex clinical skill requiring significant judgment and knowledge, not merely a procedural task. This elevates the professional standing and responsibility of triage nurses within the emergency care team. The system's developers and implementers understand that accurate triage relies heavily on the clinical judgment and foundational medical knowledge of the assessor, not just rote application of rules. This professionalizes the role of the triage nurse as a critical decision-maker at the ED's front line. Furthermore, the reliance on a standardized "Excel map" for HIS integration and mandatory regular audits demonstrates a sophisticated approach to maintaining system integrity and consistency in practice. This proactive digital governance and continuous quality assurance mechanism directly addresses the inherent challenges of "Human Error" and "Bias" identified in emergency settings. By standardizing the digital implementation and regularly verifying adherence to protocols, the system aims to ensure that the theoretical consistency of MTS translates into consistent and objective real-world application, thereby safeguarding patient care.
3. Validity and Reliability of the German Manchester Triage System
3.1. Methodologies for Assessing GMTS Performance
Assessing the performance of any medical measuring methodology, including triage systems, fundamentally relies on evaluating its reliability and validity. Reliability pertains to the truthfulness and consistency of the data obtained, indicating the degree to which a tool controls random error and yields reproducible results. Validity, conversely, assesses what an instrument measures and how effectively it does so. For the German Manchester Triage System (GMTS), construct validity of the assigned MTS level has been assessed by comparing it against various outcome measures, which serve as surrogate markers for actual urgency due to the lack of a universally accepted "gold standard". These outcome measures include hospitalization rates (general and Intensive Care Unit - ICU), mortality, length of stay in the ED and hospital, level of prehospital care received, and the number of invasive diagnostics performed. Inter-rater reliability, a measure of consistency between different assessors, was evaluated by calculating the agreement between an expert and triage nurses for a subset of emergency patients. Initial studies on GMTS performance involved a substantial sample size of 45,469 patients for validity assessment and 167 patients for inter-rater reliability, with data collected during 24-hour shifts over a two-month period. Broader studies on MTS performance emphasize the need for large, multicenter cohorts to improve generalizability.
The necessity of using "surrogate markers" like hospitalization and mortality to assess GMTS validity highlights an inherent methodological challenge in evaluating triage systems: the absence of a direct, universally agreed-upon "gold standard for actual urgency". This means GMTS's validity is demonstrated by its ability to predict
clinical outcomes correlated with urgency, rather than directly measuring urgency itself. This nuance is important for interpreting the results, as it acknowledges the inherent complexities in measuring a concept like "medical urgency" and indicates that the system's effectiveness is measured by its predictive capacity for critical downstream events. Furthermore, the emphasis on "large, multicenter studies" to improve generalizability , despite existing studies, implies that the performance of triage systems can vary significantly across different emergency departments. This suggests that even a validated system like GMTS might not perform uniformly in all German clinical settings due to local factors such as patient demographics, resource availability, or specific operational protocols. This underscores the need for ongoing, broad-scale evaluation to ensure the system's effectiveness across the diverse healthcare landscape.
3.2. Construct Validity: Impact on Patient Outcomes (Hospitalization, Mortality, Length of Stay)
The initial assessment of the German Manchester Triage System (GMTS) demonstrated its construct validity by correlating triage levels with various patient outcomes.
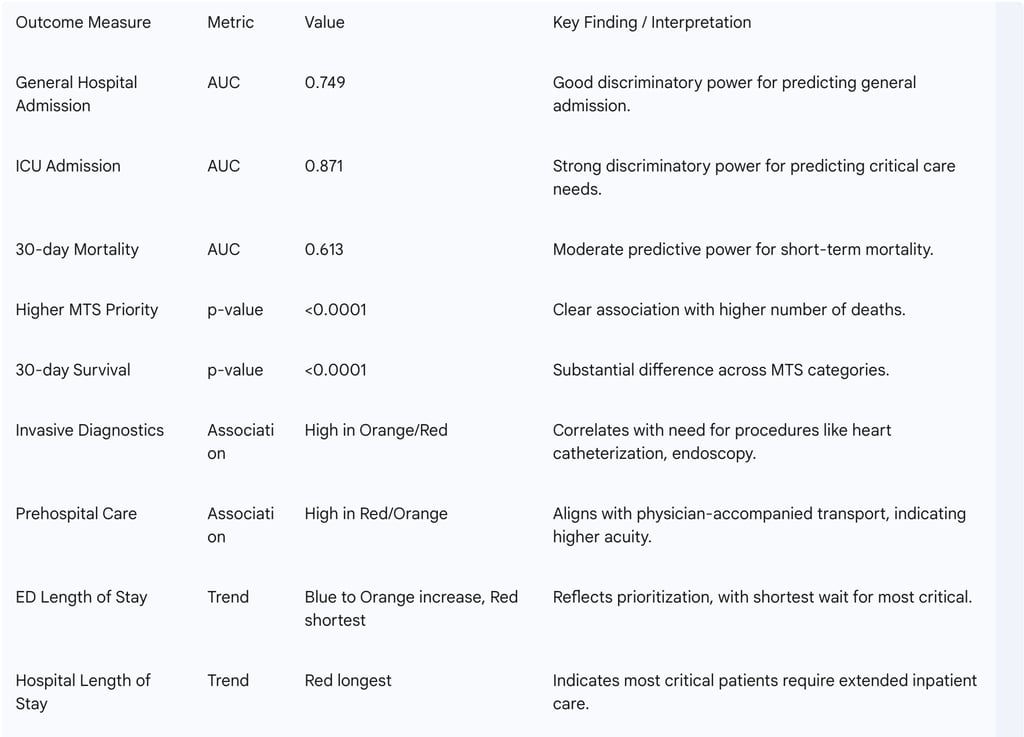
Hospital Admission: The system showed good discriminatory power for predicting hospital admission, with an Area Under the Curve (AUC) of the receiver operating characteristic of 0.749 for general hospital admission and a stronger AUC of 0.871 for admission to an Intensive Care Unit (ICU). This indicates GMTS is particularly effective at identifying patients likely to require critical care.
Patient disposition data revealed a clear gradient: 100% of patients in the Red category were admitted to hospital, 73% of Orange, and 31% of Yellow. For lower urgency, 91% of Blue and 87% of Green patients were discharged from outpatient clinics. ICU admission rates also strongly correlated with triage level: 78.57% of Red patients, 17.41% of Orange, and 1.79% of Yellow were admitted to ICU.
Mortality: A clear and statistically significant association was found between higher MTS priority levels and a higher number of deaths (p<0.0001). There was a substantial difference in 30-day survival rates among the five MTS categories (p<0.0001). The AUC for predicting 30-day mortality was 0.613. Survival rates ranged from 92.06% for Green to 59.93% for Red patients.
Invasive Diagnostics and Prehospital Care: Higher triage categories (Orange and Red) were associated with a higher incidence of invasive diagnostics, such as heart catheterizations and endoscopies. Similarly, patients triaged as Red or Orange were predominantly accompanied by an emergency physician, whereas Blue and Green category patients were typically walk-ins or transported by paramedics without prior physician contact, demonstrating alignment with the level of prehospital care received.
Length of Stay: ED length of stay generally increased from Blue to Orange categories, being shortest for Red patients. Red patients, as expected for critically ill individuals, had the longest overall hospital stays.
The validity assessment reveals a nuanced predictive power of GMTS. While the system demonstrates strong predictive capabilities for immediate, high-acuity outcomes, particularly ICU admission (AUC 0.871), its predictive capability for general hospital admission (AUC 0.749) and especially for 30-day mortality (AUC 0.613) is more moderate. This indicates that GMTS is highly effective at identifying patients requiring immediate critical intervention, aligning with its primary role as an initial urgency assessment tool. However, its precision for broader admission decisions or longer-term survival is less pronounced. The strong correlation between higher MTS categories and the intensity of subsequent medical interventions (e.g., invasive diagnostics like heart catheterizations and endoscopies for Orange and Red categories) and prehospital care (physician accompaniment for Red and Orange patients) provides robust validation for GMTS's utility in strategic resource allocation. This demonstrates that the system effectively directs high-cost, specialized resources to patients with the greatest clinical need, thereby optimizing efficiency and potentially improving outcomes by ensuring timely access to appropriate care.
Table 2: Key Validity Metrics of the German Manchester Triage System (GMTS)
3.3. Inter-Rater Reliability and Consistency of Triage Decisions
Inter-rater agreement between an expert and triage nurses for GMTS was found to be "almost perfect" with a Cohen's weighted kappa (κ) of 0.954 for a subset of 167 emergency patients. This study was conducted in September-October 2012. This exceptionally high kappa value for GMTS inter-rater reliability is particularly noteworthy, especially when compared to general MTS reliability reported in other studies, which often falls within a moderate range (κ 0.3-0.6). This significant difference suggests that the rigorous training programs for GMTS and the specific cultural adaptations for the German context may have contributed to this remarkable consistency. The study's design, involving an expert assessor and conducted at a single site after initial implementation, could also have influenced this outcome. This high reliability is a major strength for GMTS, as it ensures consistent patient categorization regardless of the individual triage nurse, which is fundamental for a standardized system.
However, while this initial study demonstrates excellent reliability, sustaining this level of consistency across all 150+ German hospitals over time, particularly with varying staff experience levels and turnover, presents an ongoing challenge. To maintain this high standard, continuous training, regular audits, and adherence to updated guidelines remain paramount, as emphasized by the MTS governance guidelines. The initial positive result sets a high benchmark, but its sustained performance requires vigilant operational oversight.
3.4. Performance Across Diverse Patient Demographics (e.g., Age Groups)
The validity of MTS (in general) is reported as moderate to good, with performance being lowest in very young and very old patients. In children, MTS showed sensitivity ranging from 0.65 to 0.83 and specificity from 0.83 to 0.89. However, studies have indicated a significant incidence of misclassification in pediatric cases, with over-triage occurring in 40-54% of children and under-triage in 12-15%. Consequently, authors have suggested modifications to MTS for use in children to attain higher validity. These findings are particularly relevant given that pediatric patients (<5 years) and older patients (>75 years) constitute "special patient groups" in German EDs.
The consistent finding that MTS performance is lowest in very young and very old patients points to a significant vulnerability in the system's application. These age groups often present with atypical or less clear symptoms, making standardized triage more challenging. This is a critical area for patient safety, as these populations are often more vulnerable to adverse outcomes from mis-triage. The fact that these are identified as "special patient groups" in German EDs further emphasizes this concern, implying a need for specialized training or adaptations within GMTS for these demographics. The suggestion for "modification of MTS for use in children" further indicates that a one-size-fits-all approach to triage, even with cultural adaptations, may not be sufficient for all patient sub-groups. This highlights a potential area for future GMTS development or specific guidelines for pediatric and geriatric emergency care to optimize its performance across the entire patient spectrum.
4. Benefits and Advantages of GMTS in German Clinical Practice
4.1. Enhancing Patient Prioritization and Optimizing Patient Flow
The Manchester Triage System plays a pivotal role in enhancing patient prioritization and optimizing patient flow within emergency departments. It empowers healthcare teams to quickly assess urgency and prioritize patients, ensuring that the most critical cases receive immediate attention. This structured approach streamlines emergency response, reducing potential downtime and enabling efficient care delivery. By optimizing patient flow, GMTS ensures that resources are allocated efficiently, directly contributing to reduced waiting times and faster access to necessary treatments. This capability is particularly vital in mitigating the global problem of ED crowding, which is often caused by rising patient volumes. The system effectively reduces queues in emergency unit facilities and aids in critical decision-making at the point of patient entry. Furthermore, it promotes a more organized and efficient method for nurses to review patient history, take vital signs, and perform initial physical assessments, ensuring a thorough evaluation of every patient.
While often framed as an efficiency tool, MTS's ability to streamline patient flow and reduce waiting times has a direct positive impact on the overall quality of care. Faster access to treatment, especially for critically ill patients, is consistently linked to improved survival rates and reduced long-term health complications. For less urgent cases, reduced waiting times also significantly enhance the patient experience. The structured approach of MTS, utilizing discriminators and systematic questions, inherently enhances the thoroughness of initial patient evaluation, thereby minimizing clinical risk. This indicates that a proactive patient safety mechanism is built directly into the system's methodology, guiding nurses to collect essential information systematically and reducing the chance of overlooking critical signs or symptoms in a high-pressure environment.
4.2. Improving Clinical Decision-Making and Patient Safety Outcomes
GMTS significantly improves clinical decision-making and contributes to enhanced patient safety outcomes. It demonstrably improves the caliber of clinical evaluations performed by nurses, facilitating prompt and well-informed decisions at the critical initial contact point. As a clinical risk management tool , GMTS assists in forecasting the severity of illnesses and predicting short-term mortality. Data show a clear correlation between higher MTS priority levels and a higher number of deaths, as well as lower 30-day survival rates, indicating its utility in identifying high-risk patients.
By providing a structured framework, GMTS empowers nurses to make critical initial decisions, enhancing their professional role in emergency care and potentially reducing immediate reliance on physician presence for initial categorization. Specially trained and experienced nursing staff are entrusted with determining patient severity , and MTS enables them to assign clinical priority based on presenting signs and symptoms without needing to make a definitive diagnosis. This robust, standardized tool allows nurses to perform a high-stakes function, increasing their autonomy and critical contribution to patient management, particularly in resource-constrained environments. The system's ability to predict outcomes such as ICU admission (with a strong AUC of 0.871 ) and mortality transforms it from a mere sorting mechanism into a critical risk prediction instrument. This predictive capability enables healthcare teams to anticipate needs, prepare specialized resources (e.g., operating rooms, critical care teams), and initiate life-saving interventions more rapidly, thereby actively mitigating clinical risk rather than merely reacting to it.
4.3. Strategic Resource Allocation and Operational Efficiency
GMTS plays a crucial role in strategic resource allocation and overall operational efficiency within German emergency departments. It facilitates efficient care delivery by ensuring that limited resources are allocated effectively. The system is designed to manage patient flow, particularly when clinical need exceeds available capacity. Its applicability extends to hospitals of all care levels and sizes , demonstrating its versatility. By reducing queues and optimizing waiting times, GMTS directly contributes to the efficient utilization of personnel and equipment. It supports comprehensive patient flow management and provides a basis for forecasting illness severity, which in turn informs resource planning.
By optimizing patient flow and resource allocation, GMTS inherently contributes to cost-effectiveness in ED operations. By ensuring high-cost resources are directed to those patients who truly need them, and by streamlining the management of low-acuity patients, the system helps reduce unnecessary resource utilization. This efficiency, coupled with reduced downtime , implicitly leads to economic benefits within the healthcare system. If less urgent cases are appropriately streamed away, for instance, to General Practice-led urgent care practices adjacent to ERs , it frees up expensive ED resources for critical cases, preventing crowding and its associated inefficiencies. Furthermore, the application of MTS principles across various care settings—including telephone triage, pre-hospital care, and community pathways —suggests a potential for system-wide optimization, not limited to the ED. If patients are appropriately triaged before even reaching the ED, it can significantly reduce the ED burden, improve pre-hospital care coordination, and ensure patients arrive at the most appropriate care setting. This signifies a move towards a more holistic and integrated approach to emergency and urgent care, leveraging triage as a central coordinating mechanism across the entire healthcare network.
5. Challenges, Limitations, and Criticisms of GMTS Implementation
5.1. Inherent Challenges in Emergency Triage Systems (e.g., Human Factors, Bias, Resource Constraints)
Despite its numerous benefits, GMTS, like any complex clinical system, faces inherent challenges rooted in human factors, potential biases, and resource limitations within the emergency care environment. Triage nurses operate under immense pressure, which can predispose them to errors in classification. Personal judgments and prejudices can inadvertently influence categorization, potentially leading to inconsistencies. Even with accurate categorization, resource constraints, such as limited staff or equipment, can result in unavoidable delays, especially during peak times or large-scale emergencies, creating patient flow bottlenecks. Beyond these, emergency nurses frequently encounter ambiguous clinical scenarios, suffer from insufficient patient history, and may have limited access to immediate diagnostic tools, all of which complicate their decision-making processes. Inexperience among newly qualified nurses, compounded by emotional stress and poor communication, further exacerbates these challenges. The presence of ethical dilemmas, cultural diversity among patients, and legal concerns also add layers of complexity to their practice.
The various challenges identified are not isolated but interact in complex ways, potentially modifying the real-world performance of GMTS. For instance, the combination of significant time constraints and emotional stress can heighten the likelihood of human error and introduce bias. Even if the triage process itself is theoretically perfect, pervasive resource limitations can create bottlenecks downstream, negating the benefits of accurate initial categorization and leading to "longer than acceptable delays". This implies that the effectiveness of GMTS is highly dependent on the broader operational environment and the adequacy of support systems within the ED, rather than solely on the tool itself. Addressing these challenges requires training that extends beyond the technical application of MTS. It necessitates comprehensive professional development that includes stress management techniques, enhanced communication skills, ethical reasoning, and strategies for managing clinical uncertainty, particularly for new nurses. This holistic approach is crucial to equip nurses to navigate the complex human and environmental factors that influence decision-making in high-pressure EDs.
5.2. Specific Criticisms and Identified Areas for Improvement within GMTS
Specific criticisms and areas for improvement have been identified within the German adaptation of the Manchester Triage System. The content of the German version differs from the English version regarding presentation diagrams and change indicators, which can significantly impact the assigned triage category. A word-for-word translation was not always possible, leading to phrasings adapted to the German context. More specifically, issues have been noted with the German translation, including only 50 instead of the original 52 flowchart diagrams, altered reaction times, and other modifications, particularly in pain evaluation. Concepts such as "hot adult" and "young pain," which are part of the original MTS, are reportedly "unaccustomed" in the German context and may lead to errors in application. While an initial assessment of GMTS validity and reliability was published in 2014 , earlier assessments noted a lack of published data on the validity and reliability of the German version , indicating a historical gap in its evidence base. Some studies continue to suggest that "sub-triage and super-triage (misclassification of severity) problems persist despite its efficacy".
The specific differences in flowcharts, indicators, and reaction times suggest that the GMTS is not merely a translation but a re-interpretation of the original MTS. This raises concerns about whether these adaptations fully maintain the integrity and evidence base of the original system, or if they introduce new areas for misinterpretation or error, particularly with concepts that are linguistically or clinically "unaccustomed". Such substantive changes could potentially alter the system's core logic, directly impacting its reliability and validity, and thus necessitating rigorous, independent validation specifically for the German version, rather than relying solely on international MTS data. The historical limitation of studies on GMTS validity and reliability , coupled with the persistence of misclassification problems , underscores the ongoing need for continuous, large-scale, independent research specific to the GMTS. This is particularly important given the identified differences from the original MTS and the varying performance observed across different EDs. Such research is crucial to fully understand its performance in the diverse German healthcare landscape and to address any persistent misclassification issues.
5.3. Practical Challenges Faced by Emergency Nurses in GMTS Application
Emergency nurses face numerous practical challenges in the daily application of GMTS, which can influence its effectiveness. They are consistently under immense pressure to make rapid decisions. This pressure is compounded by significant time constraints, the frequent presentation of ambiguous clinical scenarios, insufficient patient history, and often limited immediate access to comprehensive diagnostic tools. Inexperience among newly qualified nurses, coupled with the emotional stress inherent in emergency care and occasional poor communication within the healthcare team, further complicates their decision-making processes. Additionally, broader resource limitations, complex ethical dilemmas, the need to navigate cultural diversity among patients, and ever-present legal concerns all impact the nurses' ability to apply the triage system optimally.
These practical challenges are not merely individual issues but represent systemic factors that can significantly modify the real-world performance of GMTS, even if the system itself is well-designed. A theoretically perfect system applied within a flawed operational environment will inevitably yield suboptimal results. For example, if a nurse cannot obtain complete patient information or is operating under extreme time pressure, the accuracy of the assigned triage level, regardless of the system's inherent soundness, will suffer. This highlights that the effectiveness of GMTS is inextricably linked to the operational conditions within the ED, underscoring the critical need for systemic improvements alongside the tool's implementation. Consequently, simply providing the GMTS tool is insufficient. Hospitals must invest in comprehensive support systems for nurses, including adequate staffing levels, improved access to diagnostics, enhanced inter-professional communication protocols, and robust mental health support. These investments are crucial to maximize the system's effectiveness and ensure patient safety, recognizing that the human element is central to the successful application of any clinical risk management tool.
6. Comparative Analysis with Other Triage Systems in Germany
6.1. Overview of Prominent Five-Level Triage Systems (ATS, CTAS, ESI)
Globally, emergency departments utilize various triage systems to assess patient severity and assign treatment priorities. Beyond the Manchester Triage System (MTS), four other prominent five-level triage instruments are widely recognized: the Australasian Triage Scale (ATS), the Canadian Triage and Acuity Scale (CTAS), and the Emergency Severity Index (ESI). A general consensus in emergency medicine indicates that five-level triage systems are superior to three-level systems in both validity and reliability (p<0.01). These advanced systems are designed to correlate significantly with critical patient outcomes and resource utilization, including inpatient admission rates, duration of emergency treatment, frequency of transfer to intensive care, and mortality. The widespread adoption and proven superiority of these five-level triage systems underscore a global consensus on the optimal granularity for patient prioritization in emergency medicine. This indicates that Germany's decision to adopt a five-level system, GMTS, aligns with established international best practices in emergency care.
6.2. Comparative Assessment of Validity and Reliability
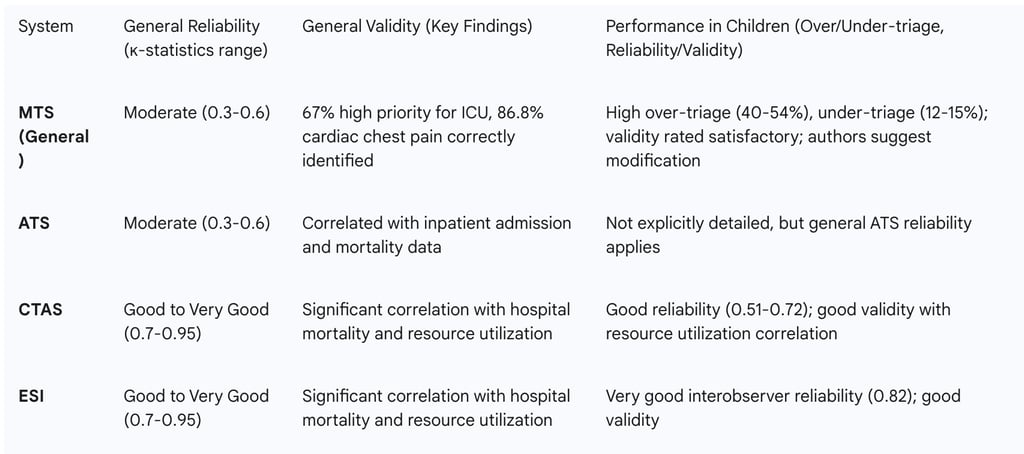
A comparative assessment of the validity and reliability of prominent five-level triage systems provides important context for evaluating GMTS.
MTS (general): Studies on the general MTS indicate moderate reliability (κ-statistics: 0.3 to 0.6) , with adult patient studies showing moderate to good reliability (κ = 0.31 to 0.62). Validity assessments descriptively show that 67% of high-priority patients were correctly identified for ICU transfer, and 86.8% of cardiac chest pain patients were correctly identified by nursing staff. However, in children, high rates of over-triage (40-54%) and under-triage (12-15%) have been reported.
ATS: The ATS also shows moderate reliability (κ-statistics: 0.3 to 0.6) , with adult reliability ranging from adequate to satisfactory (κ = 0.25 to 0.56). It has demonstrated poor agreement in psychiatric patients. Validity correlates with inpatient admission and mortality data.
CTAS: The Canadian Triage and Acuity Scale consistently demonstrates good to very good reliability (κ-statistics: 0.7 to 0.95). Interobserver reliability is reported as good to excellent in adults (κ = 0.68 to 0.89) and good in children (κ = 0.51 to 0.72). It shows a significant correlation with hospital mortality and resource utilization.
ESI: The Emergency Severity Index also exhibits good to very good reliability (κ-statistics: 0.7 to 0.95). Interobserver reliability is good to excellent in adults (κ = 0.46 to 0.91) and very good in children (κ = 0.82). ESI significantly correlates with hospital mortality and resource utilization.
Compared to CTAS and ESI, the general MTS (and by extension, potentially GMTS, given shared core principles and adaptations) appears to have moderately lower reported reliability. This suggests that while GMTS is effective, there might be other systems that offer higher consistency in triage decisions. While the initial GMTS study reported an "almost perfect" reliability (κ 0.954), this single study result might not be representative of widespread GMTS use across all German EDs. The varying performance, particularly in vulnerable populations like children and the elderly, implies that the choice of triage system, or its specific adaptations and training, should be tailored to the patient demographics and clinical context of the ED. For Germany, this means considering whether GMTS's adaptations sufficiently address these known weaknesses, or if complementary tools or different systems might be more suitable in certain contexts, particularly for specialized pediatric or geriatric emergency departments.
Table 3: Comparative Overview of Five-Level Triage Systems (MTS, ATS, CTAS, ESI)
6.3. Availability and Validation Status of Alternative Systems in the German Context
In the German context, both the Manchester Triage System (MTS) and the Emergency Severity Index (ESI) are available in German. A critical point regarding their validation status is that, as of 2010, only the ESI had been validated in German-speaking countries. Initial analyses confirmed the high validity and reliability of the German translation of the ESI, suggesting it could be adopted without modification and safely applied by nursing staff trained in Germany. However, it is important to note that the first assessment of validity and reliability for the German version of the MTS (GMTS) was subsequently published in 2014, based on data from 2012. This means that while earlier reports indicated a lack of specific German validation for MTS, this status has since changed. Charité - Universitätsmedizin Berlin, for example, has also implemented an extended MTS, incorporating additional vital sign assessments.
The historical contradiction in validation status highlights the dynamic nature of research and the importance of publication dates. The earlier claim that "only the ESI has been validated in German-speaking countries" was accurate at the time of its publication (2010) but was superseded by the foundational GMTS validation study published in 2014. This means that German hospitals now have at least two validated five-level triage systems available in their language. The fact that ESI was available and validated earlier suggests that German hospitals had, and still have, viable alternatives. The choice between GMTS and ESI might therefore depend on specific hospital needs, existing IT infrastructure, or the nuances of their respective validation data, especially for specific patient groups where MTS has known weaknesses. This situation presents a strategic decision point for German healthcare providers, allowing them to weigh the specific strengths and weaknesses of each system within their unique clinical and operational contexts.
7. Conclusion and Recommendations
7.1. Synthesis of Key Findings
The German Version of the Manchester Triage System has established itself as a widely adopted and generally effective tool for patient prioritization in German emergency departments. Its core benefits include standardizing patient assessment, optimizing patient flow, and enhancing patient safety by ensuring critical cases receive timely attention. The initial validation study for GMTS demonstrated strong predictive power for ICU admission and a clear association with mortality, alongside exceptionally high inter-rater reliability. This widespread implementation reflects a strategic alignment with international best practices in emergency medicine.
However, the assessment also reveals several important considerations. The specific adaptations of GMTS for the German context, including variations in flowcharts and time allowances, necessitate careful consideration for cross-national comparability and underscore the need for ongoing, independent validation. While effective for immediate acuity, GMTS's predictive power for general hospital admission and longer-term mortality is more moderate. Furthermore, its performance in vulnerable patient populations, such as children and the elderly, shows higher rates of misclassification, indicating a potential area for refinement. The real-world application of GMTS is also significantly influenced by the inherent challenges faced by emergency nurses, including time constraints, resource limitations, and human factors like stress and communication. The critical importance of robust training and continuous quality assurance through audits cannot be overstated for sustaining the system's benefits.
7.2. Recommendations for Further Optimization, Policy, and Future Research
Based on this assessment, the following recommendations are put forth for the further optimization of GMTS, informing policy, and guiding future research in Germany:
Optimization:
Targeted Training Modules: Develop and implement specialized training modules for triage nurses, specifically addressing the unique presentation and risk factors of vulnerable patient populations, particularly pediatric and geriatric patients. This will help mitigate the identified performance gaps and reduce misclassification rates in these groups.
Systemic Support for Nurses: Invest in improving the operational environment of emergency departments. This includes ensuring adequate staffing levels, enhancing immediate access to diagnostic tools, and establishing clearer communication protocols. Such systemic support is crucial to alleviate the immense pressure on nurses and mitigate the impact of human factors and resource constraints on GMTS application.
Continuous Quality Improvement Mechanisms: Maintain and strengthen rigorous, regular audits of GMTS application, adhering to established guidelines for sample size and frequency. This continuous quality assurance is vital for ensuring sustained reliability, identifying emerging issues in practice, and validating the system's effectiveness over time across diverse clinical settings.
Policy:
Standardization of German Adaptations: Policy bodies should evaluate the impact of specific German adaptations (e.g., variations in flowcharts, time allowances, and potentially "unaccustomed" concepts) on GMTS performance. The aim should be to establish clearer national guidelines for these variations or, where appropriate, to further standardize them across all German EDs to enhance consistency and comparability.
Encourage Inter-System Comparative Studies: Support and fund comparative studies between GMTS and other validated German-available triage systems, such as the Emergency Severity Index (ESI). Such research can provide valuable data to inform best practices and guide strategic decisions regarding system choice or complementary use in different regional or specialized hospital contexts.
Future Research:
Longitudinal Multi-center Studies: Conduct large-scale, prospective, multi-center studies on GMTS performance across a broader range of diverse German EDs. These studies should extend over longer periods to confirm the generalizability of initial validation findings, identify long-term trends in performance, and assess the system's adaptability to evolving healthcare demands.
Age-Specific Validation and Modification: Prioritize research focused specifically on the validity and reliability of GMTS in pediatric and geriatric populations. This research should aim to identify specific areas for modification within GMTS flowcharts or discriminators to improve accuracy and reduce misclassification rates for these vulnerable groups.
Patient Experience and Satisfaction: Investigate the impact of GMTS implementation on patient satisfaction and their perception of appropriate waiting times, particularly for low-urgency cases. Understanding the patient perspective is crucial for holistic system evaluation and continuous improvement.
